Uterus, Endometrium – Metaplasia, Squamous
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genetic Markers in Lung Cancer Diagnosis: a Review
International Journal of Molecular Sciences Review Genetic Markers in Lung Cancer Diagnosis: A Review Katarzyna Wadowska 1 , Iwona Bil-Lula 1 , Łukasz Trembecki 2,3 and Mariola Sliwi´ ´nska-Mosso´n 1,* 1 Department of Medical Laboratory Diagnostics, Division of Clinical Chemistry and Laboratory Haematology, Wroclaw Medical University, 50-556 Wroclaw, Poland; [email protected] (K.W.); [email protected] (I.B.-L.) 2 Department of Radiation Oncology, Lower Silesian Oncology Center, 53-413 Wroclaw, Poland; [email protected] 3 Department of Oncology, Faculty of Medicine, Wroclaw Medical University, 53-413 Wroclaw, Poland * Correspondence: [email protected]; Tel.: +48-71-784-06-30 Received: 1 June 2020; Accepted: 25 June 2020; Published: 27 June 2020 Abstract: Lung cancer is the most often diagnosed cancer in the world and the most frequent cause of cancer death. The prognosis for lung cancer is relatively poor and 75% of patients are diagnosed at its advanced stage. The currently used diagnostic tools are not sensitive enough and do not enable diagnosis at the early stage of the disease. Therefore, searching for new methods of early and accurate diagnosis of lung cancer is crucial for its effective treatment. Lung cancer is the result of multistage carcinogenesis with gradually increasing genetic and epigenetic changes. Screening for the characteristic genetic markers could enable the diagnosis of lung cancer at its early stage. The aim of this review was the summarization of both the preclinical and clinical approaches in the genetic diagnostics of lung cancer. The advancement of molecular strategies and analytic platforms makes it possible to analyze the genome changes leading to cancer development—i.e., the potential biomarkers of lung cancer. -

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

Reproductive System, Day 2 Grades 4-6, Lesson #12
Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Reproductive System, day 2 Grades 4-6, Lesson #12 Time Needed 40-50 minutes Student Learning Objectives To be able to... 1. Distinguish reproductive system facts from myths. 2. Distinguish among definitions of: ovulation, ejaculation, intercourse, fertilization, implantation, conception, circumcision, genitals, and semen. 3. Explain the process of the menstrual cycle and sperm production/ejaculation. Agenda 1. Explain lesson’s purpose. 2. Use transparencies or your own drawing skills to explain the processes of the male and female reproductive systems and to answer “Anonymous Question Box” questions. 3. Use Reproductive System Worksheets #3 and/or #4 to reinforce new terminology. 4. Use Reproductive System Worksheet #5 as a large group exercise to reinforce understanding of the reproductive process. 5. Use Reproductive System Worksheet #6 to further reinforce Activity #2, above. This lesson was most recently edited August, 2009. Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 1 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Materials Needed Classroom Materials: OPTIONAL: Reproductive System Transparency/Worksheets #1 – 2, as 4 transparencies (if you prefer not to draw) OPTIONAL: Overhead projector Student Materials: (for each student) Reproductive System Worksheets 3-6 (Which to use depends upon your class’ skill level. Each requires slightly higher level thinking.) Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 2 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -

Invasive Cervical Cancer Audit; EU Guidelines for Quality Assurance
The 4th EFCS Annual Tutorial Ospedale Universitario di Cattinara, Strada di Fiume, Trieste Handouts for lectures and workshops – I I - Gynaecological cytopathology Mrs Rietje Salet‐van‐de Pol, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands Gynecological cytology: technical aspects ............................................................................... 2 Non‐neoplastic gynecological cytology .................................................................................... 6 • Dr Giovanni Negri, General Hospital of Bolzano, Bozano SIL and cancer; ASC‐US, ASC‐H, diagnostic pitfalls and look‐alikes; glandular abnormalities 11 • Dr Amanda Herbert, Guy’s & St Thomas’ NHS Foundation Trust, London Invasive cervical cancer audit; EU guidelines for quality assurance ...................................... 17 1 Gynecological cytology: technical aspects Rietje Salet-van de Pol Important in specimen processing is to obtain as much as possible well preserved cells for microscopically evaluation. The quality of the smear depends on cell sampling, fixation and staining. For obtaining enough cervical material you are dependent on the cell sampler. For cervical cytology two types of specimen are available: conventional smears and liquid based cytology (LBC). Conventional, Thinprep and Surepath slides In conventional cytology the cell sampler makes the smear and is responsible for the fixation of the cells. Reasons for unsatisfactory conventional smears can be obscuring blood or inflammatory cells, thick smears with overlapping cells, poor preservation of the cells due to late fixation and low cellularity. In LBC the cell sampler immediately transferred the cellular material into a vial with fixative (fixating solution) which gives a better preservation of the cells. The laboratory is responsible for processing of the smear. LBC gives equally distribution of the cells in a thin cell layer of well preserved cells. The rate of unsatisfactory smears is lower. -

Pelvic Anatomyanatomy
PelvicPelvic AnatomyAnatomy RobertRobert E.E. Gutman,Gutman, MDMD ObjectivesObjectives UnderstandUnderstand pelvicpelvic anatomyanatomy Organs and structures of the female pelvis Vascular Supply Neurologic supply Pelvic and retroperitoneal contents and spaces Bony structures Connective tissue (fascia, ligaments) Pelvic floor and abdominal musculature DescribeDescribe functionalfunctional anatomyanatomy andand relevantrelevant pathophysiologypathophysiology Pelvic support Urinary continence Fecal continence AbdominalAbdominal WallWall RectusRectus FasciaFascia LayersLayers WhatWhat areare thethe layerslayers ofof thethe rectusrectus fasciafascia AboveAbove thethe arcuatearcuate line?line? BelowBelow thethe arcuatearcuate line?line? MedianMedial umbilicalumbilical fold Lateralligaments umbilical & folds folds BonyBony AnatomyAnatomy andand LigamentsLigaments BonyBony PelvisPelvis TheThe bonybony pelvispelvis isis comprisedcomprised ofof 22 innominateinnominate bones,bones, thethe sacrum,sacrum, andand thethe coccyx.coccyx. WhatWhat 33 piecespieces fusefuse toto makemake thethe InnominateInnominate bone?bone? PubisPubis IschiumIschium IliumIlium ClinicalClinical PelvimetryPelvimetry WhichWhich measurementsmeasurements thatthat cancan bebe mademade onon exam?exam? InletInlet DiagonalDiagonal ConjugateConjugate MidplaneMidplane InterspinousInterspinous diameterdiameter OutletOutlet TransverseTransverse diameterdiameter ((intertuberousintertuberous)) andand APAP diameterdiameter ((symphysissymphysis toto coccyx)coccyx) -
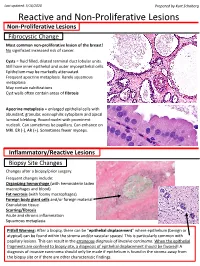
Reactive and Non-Proliferative Lesions
Last updated: 5/16/2020 Prepared by Kurt Schaberg Reactive and Non-Proliferative Lesions Non-Proliferative Lesions Fibrocystic Change Most common non-proliferative lesion of the breast! No significant increased risk of cancer. Cysts = fluid filled, dilated terminal duct lobular units. Still have inner epithelial and outer myoepithelial cells. Epithelium may be markedly attenuated. Frequent apocrine metaplasia. Rarely squamous metaplasia May contain calcifications Cyst walls often contain areas of fibrosis Apocrine metaplasia = enlarged epithelial cells with abundant, granular, eosinophilic cytoplasm and apical luminal blebbing. Round nuclei with prominent nucleoli. Can sometimes be papillary. Can enhance on MRI. ER (-), AR (+). Sometimes fewer myoeps. Inflammatory/Reactive Lesions Biopsy Site Changes Changes after a biopsy/prior surgery. Frequent changes include: Organizing hemorrhage (with hemosiderin laden macrophages and blood) Fat necrosis (with foamy macrophages) Foreign body giant cells and/or foreign material Granulation tissue Scarring/fibrosis Acute and chronic inflammation Squamous metaplasia Pitfall Warning: After a biopsy, there can be “epithelial displacement” where epithelium (benign or atypical) can be found within the stroma and/or vascular spaces! This is particularly common with papillary lesions. This can result in the erroneous diagnosis of invasive carcinoma. When the epithelial fragments are confined to biopsy site, a diagnosis of epithelial displacement should be favored! A diagnosis of invasive carcinoma should -

Primary Immature Teratoma of the Thigh Fig
CORRESPONDENCE 755 8. Gray W, Kocjan G. Diagnostic Cytopathology. 2nd ed. London: Delete all that do not apply: Elsevier Health Sciences, 2003; 677. 9. Richards A, Dalrymple C. Abnormal cervicovaginal cytology, unsatis- Cervix, colposcopic biopsy/LLETZ/cone biopsy: factory colposcopy and the use of vaginal estrogen cream: an obser- vational study of clinical outcomes for women in low estrogen states. Diagnosis: NIL (No intraepithelial lesion WHO 2014) J Obstet Gynaecol Res 2015; 41: 440e4. LSIL (CIN 1 with HPV effect WHO 2014) 10. Darragh TM, Colgan TJ, Cox T, et al. The lower anogenital squamous HSIL (CIN2/3 WHO 2014) terminology standardization project for HPV-associated lesions: back- Squamous cell carcinoma ground and consensus recommendation from the College of American Immature squamous metaplasia Pathologists and the American Society for Colposcopy and Cervical Adenocarcinoma in situ (AIS, HGGA) e Adenocarcinoma Pathology. Arch Pathol Lab Med 2012; 136: 1267 97. Atrophic change 11. McCluggage WG. Endocervical glandular lesions: controversial aspects e Extending into crypts: Not / Idenfied and ancillary techniques. J Clin Pathol 2013; 56: 164 73. Epithelial stripping: Not / Present 12. World Health Organization (WHO). Comprehensive Cervical Cancer Invasive disease: Not / Idenfied / Micro-invasive Control: A Guide to Essential Practice. 2nd ed. Geneva: WHO, 2014. Depth of invasion: mm Transformaon zone: Not / Represented Margins: DOI: https://doi.org/10.1016/j.pathol.2019.07.014 Ectocervical: Not / Clear Endocervical: Not / Clear Circumferenal: Not / Clear p16 status: Negave / Posive Primary immature teratoma of the thigh Fig. 3 A proposed synoptic reporting format for pathologists reporting colposcopic biopsies and cone biopsies or LLETZ. Sir, Teratomas are germ cell tumours composed of a variety of HSIL, AIS, micro-invasive or more advanced invasive dis- somatic tissues derived from more than one germ layer 12 ease. -

Clinical Pelvic Anatomy
SECTION ONE • Fundamentals 1 Clinical pelvic anatomy Introduction 1 Anatomical points for obstetric analgesia 3 Obstetric anatomy 1 Gynaecological anatomy 5 The pelvic organs during pregnancy 1 Anatomy of the lower urinary tract 13 the necks of the femora tends to compress the pelvis Introduction from the sides, reducing the transverse diameters of this part of the pelvis (Fig. 1.1). At an intermediate level, opposite A thorough understanding of pelvic anatomy is essential for the third segment of the sacrum, the canal retains a circular clinical practice. Not only does it facilitate an understanding cross-section. With this picture in mind, the ‘average’ of the process of labour, it also allows an appreciation of diameters of the pelvis at brim, cavity, and outlet levels can the mechanisms of sexual function and reproduction, and be readily understood (Table 1.1). establishes a background to the understanding of gynae- The distortions from a circular cross-section, however, cological pathology. Congenital abnormalities are discussed are very modest. If, in circumstances of malnutrition or in Chapter 3. metabolic bone disease, the consolidation of bone is impaired, more gross distortion of the pelvic shape is liable to occur, and labour is likely to involve mechanical difficulty. Obstetric anatomy This is termed cephalopelvic disproportion. The changing cross-sectional shape of the true pelvis at different levels The bony pelvis – transverse oval at the brim and anteroposterior oval at the outlet – usually determines a fundamental feature of The girdle of bones formed by the sacrum and the two labour, i.e. that the ovoid fetal head enters the brim with its innominate bones has several important functions (Fig. -

Squamous Metaplasia of the Tracheal Epithelium in Children
Thorax: first published as 10.1136/thx.31.2.167 on 1 April 1976. Downloaded from Thorax (1976), 31, 167. Squamous metaplasia of the tracheal epithelium in children AVINASH MITHAL' and JOHN L. EMERY2 The Chest Clinic, Lincoln' and The Children's Hospital, Sheffield' Mithal, A. and Emery, J. L. (1976). Thorax, 31, 167-171. Squamous metaplasia of the tracheal epithelium in children. Thirty-seven (16%) tracheas from 2170 children showed squamous metaplasia. (Cases with tracheo-oesophageal fistula and congenital heart disease were excluded.) The metaplasia extended into the bronchi in 15 cases. Features of pulmonary retention were present in seven cases. Respiratory infection, probably viral, seemed to be the most significant causative factor in 20 children, including those with cystic fibrosis. Tracheal instrumentation was a possible factor in 11 cases but oxygen therapy alone did not seem important. The metaplasia was almost certainly congenital in one child and probably in two others but no stillborn infants showed metaplasia. In many children the metaplasia seemed to be due to a combination of factors. Squamous metaplasia of the trachea in childhood Tracheas from children with tracheo-oesophageal has been described in cases of measles (Gold- fistula and those with congenital heart disease or zieher, 1918), influenza (Askanazy, 1919), cystic other gross deformities were excluded. There were fibrosis of the pancreas (Zuelzer and Newton, thus 2331 tracheas available for study. Epithelium 1949), and following intubation of the trachea was absent in 16 cases. This left 2170 tracheas for http://thorax.bmj.com/ (Rasche and Kuhns, 1972) and tracheostomy histological analysis. (Sara, 1967; Sara and Reye, 1969). -

Squamous Metaplasia of Normal and Carcinoma in Situ of HPV 16-Immortalized Human Endocervical Cells1
[CANCER RESEARCH 52. 4254-4260, August I, 1992] Squamous Metaplasia of Normal and Carcinoma in Situ of HPV 16-Immortalized Human Endocervical Cells1 Qi Sun, Kouichiro Tsutsumi, M. Brian Kelleher, Alan Pater, and Mary M. Pater2 Division of Basic Medical Sciences, Faculty of Medicine, Memorial University of Newfoundland, St. John's, Newfoundland, Canada A1B ÌV6 ABSTRACT genomic DNA, most frequently of HPV 16, has been detected in 90% of the cervical carcinomas and are found to be actively The importance of cervical squamous metaplasia and human papil- expressed (6, 7). HPV 16 DNA has been used to transform lomavirus 16 (HPV 16) infection for cervical carcinoma has been well human foreskin and ectocervical keratinocytes (8, 9). It immor established. Nearly 87% of the intraepithelial neoplasia of the cervix occur in the transformation zone, which is composed of squamous meta- talizes human keratinocytes efficiently, producing cell clones plastic cells with unclear origin. HPV DNA, mostly HPV 16, has been with indefinite life span in culture. Different approaches have found in 90% of cervical carcinomas, but only limited experimental data been taken to examine the behavior of these immortalized cell are available to discern the role of HPV 16 in this tissue specific onco- lines in conditions allowing squamous differentiation (10, 11). genesis. We have initiated in vivo studies of cultured endocervical cells After transplantation in vivo, the HPV 16-immortalized kerat as an experimental model system for development of cervical neoplasia. inocytes retain thépotential for squamous differentiation, Using a modified in vivo implantation system, cultured normal endocer forming abnormal epithelium without dysplastic changes at vical epithelial cells formed epithelium resembling squamous metapla early passages and with various dysplastic changes only after sia, whereas those immortalized by HPV 16 developed into lesions long periods of time in culture (10). -

Squamous Cell Carcinoma of the Breast As a Clinical Diagnostic Challenge
582 MOLECULAR AND CLINICAL ONCOLOGY 8: 582-586, 2018 Squamous cell carcinoma of the breast as a clinical diagnostic challenge KATARZYNA JAKUBOWSKA1, LUIZA KAŃCZUGA‑KODA1, WOJCIECH KISIELEWSKI2, MARIUSZ KODA3 and WALDEMAR FAMULSKI1,2 1Department of Pathomorphology, Comprehensive Cancer Center, 15‑027 Białystok; Departments of 2Medical Pathomorphology and 3General Pathomorphology, Medical University of Białystok, 15‑269 Białystok, Poland Received September 17, 2017; Accepted December 14, 2017 DOI: 10.3892/mco.2018.1581 Abstract. Squamous cell carcinoma (SqCC) of the breast metaplasia of ductal and lobular epithelial cells can be should be differentiated between the primary skin keratinizing linked with fat necrosis and infracted ademonas. Squamous squamous carcinoma and squamous metaplastic cancer. In the cell carcinoma should be differentiated between lesions of current study, the cases of two patients who were diagnosed keratinizing squamous carcinoma and squamous metaplasia with SqCC originated from skin and the breast were discussed. associated to mammary carcinoma (2). The characteristic A fine-needle aspiration biopsy confirmed the presence features of metaplastic cell carcinoma include: i) primary of atypical squamous cells. In both cases, the microscopic carcinoma without other neoplastic components such as ductal examination of the surgical specimen revealed a malignant or mesenchymal elements, ii) the tumor origin is independent neoplasm differentiated into SqCC characterized by keratin- of the overlying skin and nipple and iii) absence of primary izing cancer cells with abundant eosiphilic cytoplasm with epidermoid tumors present in other site (oral cavity, bronchus, large, hyperchromatic vesicular nuclei. Immunohistochemical esophagus, bladder, cervix ect.) (3). However, squamous studies showed negative for progesterone and estrogen recep- metaplastic carcinoma should be also differentiated with pure tors and human epidermal growth factor receptor 2.