Chapter 1 Cellular Reaction to Injury 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Genotoxicity and Cytotoxicity Amongst in Dental
Dental, Oral and Craniofacial Research Research Article ISSN: 2058-5314 Evaluation of genotoxicity and cytotoxicity amongst in dental surgeons and technicians by micronucleus assay Molina Noyola Leonardo Daniel1,2, Coronado Romo María Eugenia3, Vázquez Alcaraz Silverio Jafet4, Izaguirre Pérez Marian Eliza1,2, Arellano-García Evarista5, Flores-García Aurelio6 and Torres Bugarín Olivia1* 1Laboratorio de Evaluación de Genotóxicos, Programa Internacional de Medicina, Universidad Autónoma de Guadalajara, Mexico 2Facultad de Medicina, Universidad Autónoma de Guadalajara, Mexico 3Departamento de Ortodoncia, Facultad de Odontología, Universidad Autónoma de Guadalajara, Mexico 4Departamento de Endodoncia, Facultad de Odontología, Universidad Autónoma de Guadalajara, Mexico 5Facultad de Ciencias, Universidad Autónoma de Baja California, Mexico 6Unidad Académica de Medicina, Universidad Autónoma de Nayarit, Tepic, Nayarit, Mexico Abstract Introduction: Dental surgeons and technicians are continuously exposed to agents could be affect the genetic material and induce mutations. The aim of this study was to evaluate the genotoxic and cytotoxic occupational risk of dental surgeons and technicians through the micronucleated cells (MNC) and nuclear abnormalities (NA) assay in oral mucosa. Methods: Case-control study. We have collected a buccal mucosa from dental surgeons, dental technicians and healthy individuals (matched by BMI, age and gender). The smears were fixed (ethanol 80%/48 h), stained (orange acridine) and analyzed (microscope, 100×). The frequency of MNC and NA (binucleated cells [BNC], lobulated nucleus [LN], condensed chromatins [CC], karyorrhexis [KR], pyknosis (PN) and karyolysis [KL] were counted in 2,000 cells per participant. Results: 90 samples were collected (26 surgeons, 19 technicians and 45 controls). Compared with controls, exception of PN, in surgeons was higher frequency and positive association of MNC and all NA (p<0.05). -
Efficacy of Texture and Color Enhancement Imaging In
www.nature.com/scientificreports OPEN Efcacy of Texture and Color Enhancement Imaging in visualizing gastric mucosal atrophy and gastric neoplasms Tsubasa Ishikawa1, Tomoaki Matsumura1*, Kenichiro Okimoto1, Ariki Nagashima1, Wataru Shiratori1, Tatsuya Kaneko1, Hirotaka Oura1, Mamoru Tokunaga1, Naoki Akizue1, Yuki Ohta1, Keiko Saito1, Makoto Arai1,2, Jun Kato1 & Naoya Kato1 In 2020, Olympus Medical Systems Corporation introduced the Texture and Color Enhancement Imaging (TXI) as a new image-enhanced endoscopy. This study aimed to evaluate the visibility of neoplasms and mucosal atrophy in the upper gastrointestinal tract through TXI. We evaluated 72 and 60 images of 12 gastric neoplasms and 20 gastric atrophic/nonatrophic mucosa, respectively. The visibility of gastric mucosal atrophy and gastric neoplasm was assessed by six endoscopists using a previously reported visibility scale (1 = poor to 4 = excellent). Color diferences between gastric mucosal atrophy and nonatrophic mucosa and between gastric neoplasm and adjacent areas were assessed using the International Commission on Illumination L*a*b* color space system. The visibility of mucosal atrophy and gastric neoplasm was signifcantly improved in TXI mode 1 compared with that in white-light imaging (WLI) (visibility score: 3.8 ± 0.5 vs. 2.8 ± 0.9, p < 0.01 for mucosal atrophy; visibility score: 2.8 ± 1.0 vs. 2.0 ± 0.9, p < 0.01 for gastric neoplasm). Regarding gastric atrophic and nonatrophic mucosae, TXI mode 1 had a signifcantly greater color diference than WLI (color diferences: 14.2 ± 8.0 vs. 8.7 ± 4.2, respectively, p < 0.01). TXI may be a useful observation modality in the endoscopic screening of the upper gastrointestinal tract. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -

Membrane Attack Complex in Myocardial Ischemia/Reperfusion Injury: a Systematic Review for Post Mortem Applications
diagnostics Review Membrane Attack Complex in Myocardial Ischemia/Reperfusion Injury: A Systematic Review for Post Mortem Applications Cristina Mondello 1,*, Elvira Ventura Spagnolo 2,*, Luigi Cardia 3 , Daniela Sapienza 1, Serena Scurria 1, Patrizia Gualniera 1 and Alessio Asmundo 1 1 Department of Biomedical and Dental Sciences and Morphofunctional Imaging, University of Messina, via Consolare Valeria, 1, 98125 Messina, Italy; [email protected] (D.S.); [email protected] (S.S.); [email protected] (P.G.); [email protected] (A.A.) 2 Section Legal Medicine, Department of Health Promotion Sciences, Maternal and Infant Care, Internal Medicine and Medical Specialties (PROMISE), University of Palermo, Via del Vespro, 129, 90127 Palermo, Italy 3 IRCCS Centro Neurolesi Bonino-Pulejo, 98100 Messina, Italy; [email protected] * Correspondence: [email protected] (C.M.); [email protected] (E.V.S.); Tel.: +39-347062414 (C.M.); +39-3496465532 (E.V.S.) Received: 19 October 2020; Accepted: 31 October 2020; Published: 2 November 2020 Abstract: The complement system has a significant role in myocardial ischemia/reperfusion injury, being responsible for cell lysis and amplification of inflammatory response. In this context, several studies highlight that terminal complement complex C5b-9, also known as the membrane attack complex (MAC), is a significant contributor. The MAC functions were studied by many researchers analyzing the characteristics of its activation in myocardial infarction. Here, a systematic literature review was reported to evaluate the principal features, advantages, and limits (regarding the application) of complement components and MAC in post mortem settings to perform the diagnosis of myocardial ischemia/infarction. The review was performed according to specific inclusion and exclusion criteria, and a total of 26 studies were identified. -

Tumor Destruction and Kinetics of Tumor Cell Death in Two Experimental Mouse Tumors Following Photodynamic Therapy1
[CANCER RESEARCH 45, 572-576, February 1985] Tumor Destruction and Kinetics of Tumor Cell Death in Two Experimental Mouse Tumors following Photodynamic Therapy1 Barbara W. Henderson,2 Stephen M. Waldow, Thomas S. Mang, William R. Potter, Patrick B. Malone, and Thomas J. Dougherty Division ot Radiation Biology, Department of Radiation Medicine, Roswell Park Memorial Institute, Buffalo, New York 14263 ABSTRACT rapid tumor necrosis (8, 11). Preceding tumor necrosis are pronounced changes in the vascular system of the tumor (3, 5, The effect of photodynamic therapy (PDT) on tumor growth 23). as well as on tumor Å“il survival in vitro and in vivo was studied In vitro, dose-dependent (photosensitizer + light) photody in the EMT-6 and RIF experimental mouse tumor systems. In namic cell killing is characterized by cell lysis within 1 hr after a vitro, RIF cells were more sensitive towards PDT than were lethal PDT dose (1) and can be achieved in all cell types studied EMT-6 cells when incubated with porphyrin (25 u,g/m\, dihema- thus far, normal as well as malignant (2, 6,14). toporphyrin ether) and subsequently given graded doses of light. Despite extensive in vivo and in vitro studies, it has not yet In vivo, both tumor types responded to PDT (EMT-6, dihemato- been established whether tumor cell killing in vivo is governed porphyrin ether, 7.5 mg/kg; RIF, dihematoporphyrin ether, 10 by the same mechanism as is cell killing in vitro. To answer this mg/kg; both followed 24 hr later by 135 J of light at 630 nm/sq question, we studied the relationship between tumor destruction, cm) with severe vascular disruption and subsequent disappear tumor cure, and tumor cell survival kinetics in 2 experimental ance of tumor bulk. -

71182407Ad80c7abf430b599eb
Journal name: International Journal of Nanomedicine Article Designation: Original Research Year: 2017 Volume: 12 International Journal of Nanomedicine Dovepress Running head verso: Yang et al Running head recto: HA-SPIONs for effective cancer diagnosis and treatment open access to scientific and medical research DOI: http://dx.doi.org/10.2147/IJN.S121249 Open Access Full Text Article ORIGINAL RESEARCH Hyaluronan-modified superparamagnetic iron oxide nanoparticles for bimodal breast cancer imaging and photothermal therapy Rui-Meng Yang1,* Abstract: Theranostic nanoparticles with both imaging and therapeutic abilities are highly Chao-Ping Fu2,* promising in successful diagnosis and treatment of the most devastating cancers. In this study, Jin-Zhi Fang1 the dual-modal imaging and photothermal effect of hyaluronan (HA)-modified superparamag- Xiang-Dong Xu1 netic iron oxide nanoparticles (HA-SPIONs), which was developed in a previous study, were Xin-Hua Wei1 investigated for CD44 HA receptor-overexpressing breast cancer in both in vitro and in vivo Wen-Jie Tang1 experiments. Heat is found to be rapidly generated by near-infrared laser range irradiation of HA- SPIONs. When incubated with CD44 HA receptor-overexpressing MDA-MB-231 cells in vitro, Xin-Qing Jiang1 HA-SPIONs exhibited significant specific cellular uptake and specific accumulation confirmed Li-Ming Zhang2 by Prussian blue staining. The in vitro and in vivo results of magnetic resonance imaging and 1Department of Radiology, Guangzhou photothermal ablation demonstrated that HA-SPIONs exhibited significant negative contrast First People’s Hospital, Guangzhou enhancement on T -weighted magnetic resonance imaging and photothermal effect targeted Medical University, 2School of 2 Materials Science and Engineering, CD44 HA receptor-overexpressing breast cancer. -

Absolute Measurement of the Tissue Origins of Cell-Free DNA in the Healthy State and Following Paracetamol Overdose Danny Laurent1, Fiona Semple1, Philip J
Laurent et al. BMC Medical Genomics (2020) 13:60 https://doi.org/10.1186/s12920-020-0705-2 RESEARCH ARTICLE Open Access Absolute measurement of the tissue origins of cell-free DNA in the healthy state and following paracetamol overdose Danny Laurent1, Fiona Semple1, Philip J. Starkey Lewis2, Elaine Rose1, Holly A. Black1, Jennifer Coe1, Stuart J. Forbes2, Mark J. Arends3, James W. Dear4 and Timothy J. Aitman1* Abstract Background: Despite the emergence of cell-free DNA (cfDNA) as a clinical biomarker in cancer, the tissue origins of cfDNA in healthy individuals have to date been inferred only by indirect and relative measurement methods, such as tissue-specific methylation and nucleosomal profiling. Methods: We performed the first direct, absolute measurement of the tissue origins of cfDNA, using tissue-specific knockout mouse strains, in both healthy mice and following paracetamol (APAP) overdose. We then investigated the utility of total cfDNA and the percentage of liver-specific cfDNA as clinical biomarkers in patients presenting with APAP overdose. Results: Analysis of cfDNA from healthy tissue-specific knockout mice showed that cfDNA originates predominantly from white and red blood cell lineages, with minor contribution from hepatocytes, and no detectable contribution from skeletal and cardiac muscle. Following APAP overdose in mice, total plasma cfDNA and the percentage fraction originating from hepatocytes increased by ~ 100 and ~ 19-fold respectively. Total cfDNA increased by an average of more than 236-fold in clinical samples from APAP overdose patients with biochemical evidence of liver injury, and 18-fold in patients without biochemically apparent liver injury. Measurement of liver-specific cfDNA, using droplet digital PCR and methylation analysis, revealed that the contribution of liver to cfDNA was increased by an average of 175-fold in APAP overdose patients with biochemically apparent liver injury compared to healthy subjects, but was not increased in overdose patients with normal liver function tests. -
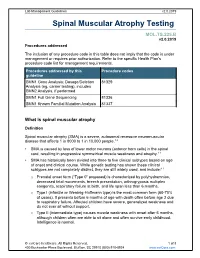
Spinal Muscular Atrophy Testing
Lab Management Guidelines v2.0.2019 Spinal Muscular Atrophy Testing MOL.TS.225.B v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline SMN1 Gene Analysis; Dosage/Deletion 81329 Analysis (eg, carrier testing), includes SMN2 Analysis, if performed SMN1 Full Gene Sequencing 81336 SMN1 Known Familial Mutation Analysis 81337 What is spinal muscular atrophy Definition Spinal muscular atrophy (SMA) is a severe, autosomal recessive neuromuscular disease that affects 1 in 8000 to 1 in 10,000 people.1,2 SMA is caused by loss of lower motor neurons (anterior horn cells) in the spinal cord, resulting in progressive symmetrical muscle weakness and atrophy.1-3 SMA has historically been divided into three to five clinical subtypes based on age of onset and clinical course. While genetic testing has shown these clinical subtypes are not completely distinct, they are still widely used, and include:1-3 o Prenatal onset form (“Type 0” proposed) is characterized by polyhydramnios, decreased fetal movements, breech presentation, arthrogryposis multiplex congenita, respiratory failure at birth, and life span less than 6 months. o Type I (infantile or Werdnig-Hoffmann type) is the most common form (60-70% of cases). It presents before 6 months of age with death often before age 2 due to respiratory failure. Affected children have severe, generalized weakness and do not ever sit without support. -

Università Degli Studi Di Milano
UNIVERSITÀ DEGLI STUDI DI MILANO SCUOLA DI DOTTORATO IN MEDICINA MOLECOLARE CICLO XXVIII Anno Accademico 2014/2015 TESI DI DOTTORATO DI RICERCA MED09 STUDIES OF HEME-REGULATED eIF2α KINASE STRESS SIGNALING ON MATURATION OF MACROPHAGES AND ERYTHROBLASTIC ISLAND FORMATION IN IRON RESTRICTIVE ERYTHROPOIESIS Dottorando : Elena PALTRINIERI Matricola N° R10203 TUTORE : Chiar.ma Prof.ssa Maria Domenica CAPPELLINI CO-TUTORE: Prof.ssa Jane-Jane CHEN DIRETTORE DEL DOTTORATO: Chiar.mo Prof. Mario CLERICI ABSTRACT Iron is the most important metal for the human body. Different states of iron deficiency have long existed and remain very common in today’s population. The vast majority of cases of iron deficiency are acquired as a result from blood loss. Any condition in which dietary iron intake does not meet the body’s demands will result in iron deficiency. Iron and heme are both fundamental in hemoglobin synthesis and erythroid cell differentiation. In addition to act as a prosthetic group for hemoglobin, heme regulates the transcription of globin genes and controls the translational activity in erythroid precursors through modulation of the kinase activity of the eIF2α kinase HRI which is regulated by heme. HRI, the heme-regulated inhibitor of translation, was first discovered in reticulocytes under the conditions of iron and heme deficiencies. During heme deficiency conditions, in the erythroid precursors protein synthesis is inhibited by phosphorylation of the α-subunit of the eukaryotic initiation factor 2 (eIF2α) as the result of the activation of HRI. The role of HRI is to control that the amount of globin chains synthesized are not in excess of what can be utilized for hemoglobin tetramers depending of heme available. -
Understanding Cancer Tutorial Information for Teachers
Understanding Cancer Tutorial Information for Teachers Understanding Cancer Tutorial • This tutorial was adapted from the Understanding Cancer: Cancer Tutorial available at http://www.cancer.gov/cancertopics/ understandingcancer/cancer • There are two forms for this PPT: – Teacher Presentation version (with a script) – Student Handout version (if printing, specify black/ white on print menu) R Understanding Cancer Tutorial Information for Teachers • The National Cancer Institute has produced a series of cancer related PowerPoint tutorials. These are available as downloadable format at http://www.cancer.gov/cancertopics/ understandingcancer. • Each PowerPoint in this series includes a teacher script. Once these have been downloaded, you may modify the slide show and print student handouts. R Understanding Cancer Teacher Information Developed by: Lewis J. Kleinsmith, Ph.D. Donna Kerrigan, M.S. Jeanne Kelly Brian Hollen Discusses and illustrates what cancer is, explains the link between genes and cancer, and discusses what is known about the causes, detection, and diagnosis of the disease. These PowerPoint slides are not locked files. You can mix and match slides from different tutorials as you prepare your own lectures. In the Notes section, you will find explanations of the graphics. The art in this tutorial is copyrighted and may not be reused for commercial gain. Please do not remove the NCI logo or the copyright mark from any slide. These tutorials may be copied only if they are distributed free of charge for educational purposes. R Cancer R Understanding Cancer Developed by: Lewis J. Kleinsmith, Ph.D. Donna Kerrigan, M.S. Jeanne Kelly Brian Hollen Discusses and illustrates what cancer is, explains the link between genes and cancer, and discusses what is known about the causes, detection, and diagnosis of the disease. -

General Pathology
Jordan University of Science and Technology Faculty of Medicine 2018-2019 COURSE TITLE : GENERAL PATHOLOGY. COURSE CODE : MED 231. CREDIT HOURS : 3 CREDIT HOURS SEQUENCE : YEAR 2, FIRST SEMESTER COURSE COORDINATOR: Dr. Alia AlMuhtaseb; Dr. Mohammad Orjani CONTACT: [email protected]; [email protected] Course Description: This course deals with the investigation of those pathological mechanisms common to all tissue-cell pathology. Attention is paid to the processes of cellular adaptation, inflammation, repair, immunology, cellular accumulation, and neoplasia. Lecture will attempt first to familiarize the student with our basic layers of defense. Next those vocabulary terms and concepts relevant to the disease process will be introduced. The terminology employed is both medical and chiropractic. Processes and concepts will be developed with the aid of Data show. An interactive format is employed in which the instructor poses questions to enable the student to self-test their knowledge prior to exams and develop skills in communicating these basic pathological concepts to others. During the course and whenever relevant the students are exposed to clinical problems to emphasize the explanations of symptoms, signs, investigations and forms of treatments. Practical sessions are planned to give students the opportunity to expose their knowledge for discussion and confirm concepts learned in lectures. Small group discussions of clinical cases are planned at the end of the course were students are divided into small groups and with the help of an instructor they analyze and discuss the problem. The course will be given through 28 lectures, 7 practical (laboratory) sessions, and one small group discussion activity over 15 weeks and for one whole semester. -

Mycobacterium Tuberculosis Scott M
© 2015. Published by The Company of Biologists Ltd | Disease Models & Mechanisms (2015) 8, 591-602 doi:10.1242/dmm.019570 RESEARCH ARTICLE Presence of multiple lesion types with vastly different microenvironments in C3HeB/FeJ mice following aerosol infection with Mycobacterium tuberculosis Scott M. Irwin1, Emily Driver1, Edward Lyon1, Christopher Schrupp1, Gavin Ryan1, Mercedes Gonzalez-Juarrero1, Randall J. Basaraba1, Eric L. Nuermberger2 and Anne J. Lenaerts1,* ABSTRACT reservoir (Lin and Flynn, 2010). Since 2008, the incidence of Cost-effective animal models that accurately reflect the pathological multiple-drug-resistant (MDR) tuberculosis (TB) in Africa has progression of pulmonary tuberculosis are needed to screen and almost doubled, while in southeast Asia the incidence has increased evaluate novel tuberculosis drugs and drug regimens. Pulmonary more than 11 times (World Health Organization, 2013). Globally, disease in humans is characterized by a number of heterogeneous the incidence of MDR TB increased 42% from 2011 to 2012, with lesion types that reflect differences in cellular composition and almost 10% of those cases being extensively drug-resistant (XDR) organization, extent of encapsulation, and degree of caseous TB. With the rise in MDR and XDR TB, new drugs and especially necrosis. C3HeB/FeJ mice have been increasingly used to model drugs with a novel mechanism of action or drugs that can shorten the tuberculosis infection because they produce hypoxic, well-defined duration of treatment are desperately needed. granulomas