Vision for the Vale of Leven Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Joint Hospital, Dumbarton
Joint Hospital, Dumbarton At present the hospital provides Mental Health Services and Addiction Services to a population of approximately 80,000 people and covers the wide geographical areas of Alexandria, Patient Information Leaflet Dumbarton and Helensburgh. Developments within the hospital have seen the introduction of many services including drug and alcohol, mental health crisis team, out of hours services, dementia day hospital, community and in-patient dementia services to name but a few. The adult CMHT provide services from Riverview Resource Centre. Riverview Resource Centre Community Mental Health Team (Adult) for Dumbarton & Alexandria areas Riverview Resourc Centre Victoria Infirmary Community Mental Health Team (Adult) for the Helensburgh & Lochside areas. CMHT (Adult) Service Aims The aim is to provide a locally based responsive service which delivers high quality community care to adults and their families in their own homes who are experiencing Mental Health problems. They can offer a specialised mental health assessment and various different treatment approaches according to identified need. Treatments available include psychosocial interventions aimed at reducing symptoms and increasing coping skills. The local teams work with a range of local services including: Local Authority, Voluntary Services and Primary Health Care Teams. The Team consists of: Medical Staff Nursing staff . Admin & Clerical Social Workers MHOs SW Assistant Clinical Psychology Occupational Therapist Operational Aspects Flexible referral system Monday to Friday 9.00am-6.00pm Keyworker system/care management MDT assessment/reviews/care planning Discharge Planning/CPA Risk Assessment/management Services Provided Assessment clinics Operate a duty system/crisis services Diagnostics/Care Planning Supportive counselling Brief therapies Cognitive Behavioural Techniques Social Skills training Problem solving techniques Assertiveness/confidence building Independent living skills Anxiety Management Referral to other appropriate services i.e. -

Glasgow City Community Health Partnership Service Directory 2014 Content Page
Glasgow City Community Health Partnership Service Directory 2014 Content Page About the CHP 1 Glasgow City CHP Headquarters 2 North East Sector 3 North West Sector 4 South Sector 5 Adult Protection 6 Child Protection 6 Emergency and Out-of-Hours care 6 Addictions 7 - 9 Asylum Seekers 9 Breast Screening 9 Breastfeeding 9 Carers 10 - 12 Children and Families 13 - 14 Dental and Oral Health 15 Diabetes 16 Dietetics 17 Domestic Abuse / Violence 18 Employability 19 - 20 Equality 20 Healthy Living 21 Health Centres 22 - 23 Hospitals 24 - 25 Housing and Homelessness 26 - 27 Learning Disabilities 28 - 29 Mental Health 30 - 40 Money Advice 41 Nursing 41 Physiotherapy 42 Podiatry 42 Respiratory 42 Rehabilitation Services 43 Sexual Health 44 Rape and Sexual Assault 45 Stop Smoking 45 Transport 46 Volunteering 46 Young People 47-49 Public Partnership Forum 50 Comments and Complaints 51-21 About Glasgow City Community Health Partnership Glasgow City Community Health Partnership (GCCHP) was established in November 2010 and provides a wide range of community based health services delivered in homes, health centres, clinics and schools. These include health visiting, health improvement, district nursing, speech and language therapy, physiotherapy, podiatry, nutrition and dietetic services, mental health, addictions and learning disability services. As well as this, we host a range of specialist services including: Specialist Children’s Services, Homeless Services and The Sandyford. We are part of NHS Greater Glasgow & Clyde and provide services for 584,000 people - the entire population living within the area defined by the LocalAuthority boundary of Glasgow City Council. Within our boundary, we have: 154 GP practices 136 dental practices 186 pharmacies 85 optometry practices (opticians) The CHP has more than 3,000 staff working for it and is split into three sectors which are aligned to local social work and community planning boundaries. -

Glasgow Pulmonary Rehabilitation Service
Glasgow and Clyde Pulmonary Rehabilitation Service Pulmonary rehabilitation is a comprehensive, multidisciplinary programme of exercise and education that should: Improve functional exercise capacity Improve health status Reduce dyspnoea Inclusion Criteria Exclusion Criteria Diagnosis of COPD Successful Completion of pulmonary rehabilitation MRC grade 3 or greater programme within the past 2 years (See Maintenance below) On optimum drug therapy Psychiatric, cognitive or locomotor problems that would Motivated to participate prevent participation in exercise or in a group setting Decompensate heart failure MRC dysnoea scale (must be 3 or greater) Grade 1: Not troubled by breathlessness except on strenuous exercise Grade 2: Short of breath when hurrying or walking up a slight hill Grade 3: Walks slower than contemporaries on level ground because of breathlessness, or has to stop for breath when walking at own pace Grade 4: Stops for a breath after walking about 100m or after a few minutes on level ground Grade 5: Too breathless to leave the house or breathlessness when dressing or undressing The Following Do Not Exclude Rehabilitation Transport Age Hypoxia or oxygen dependence Continued smoking Referral Guidance All patients should be referred using online or paper referral Patients will receive an invite for assessment at their local hospital within 4/6 weeks of receipt of the referral form. Patients failing to respond will be sent a second letter then discharged if no response. Assessment Sites Gartnavel General Hospital -

Mental Health Bed Census
Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Data Collection Documentation Document Type: Guidance Notes Collections: 1. Mental Health and Learning Disability Bed Census: One Day Audit 2. Mental Health and Learning Disability Patients: Out of Scotland and Out of NHS Placements SG deadline: 30th November 2014 Coverage: Census date: Midnight, 29th Oct 2014 Page 1 – 10 Nov 2014 Scottish Government One Day Audit of Inpatient Bed Use Definitions for Data Recording VERSION 2.4 – 10.11.14 Document Details Issue History Version Status Authors Issue Date Issued To Comments / changes 1.0 Draft Moira Connolly, NHS Boards Beth Hamilton, Claire Gordon, Ellen Lynch 1.14 Draft Beth Hamilton, Ellen Lynch, John Mitchell, Moira Connolly, Claire Gordon, 2.0 Final Beth Hamilton, 19th Sept 2014 NHS Boards, Ellen Lynch, Scottish John Mitchell, Government Moira Connolly, website Claire Gordon, 2.1 Final Ellen Lynch 9th Oct 2014 NHS Boards, Further clarification included for the following data items:: Scottish Government Patient names (applicable for both censuses) website ProcXed.Net will convert to BLOCK CAPITALS, NHS Boards do not have to do this in advance. Other diagnosis (applicable for both censuses) If free text is being used then separate each health condition with a comma. Mental Health and Learning Disability Bed Census o Data item: Mental Health/Learning Disability diagnosis on admission Can use full description option or ICD10 code only option. o Data item: Last known Mental Health/Learning Disability diagnosis Can use full description option or ICD10 code only option. -

PDF Timetable
Ref. LS022E/07/18 Route Map Service 340 Whilst every effort will be made to adhere to the scheduled times, the Partnership disclaims any liability in respect of loss or inconvenience arising from any failure to operate journeys as published, changes in timings or printing Bus Timetable errors. From 15 July 2018 340 Helensburgh Vale of Leven For more information visit spt.co.uk Hospital Alternatively, for all public transport enquiries, call: Royal Alexandra Hospital This service is operated by McColl’s Travel This service is operated by Limited on behalf of Strathclyde McColl’s Travel Limited on Partnership for Transport. If you have any behalf of SPT. comments or suggestions about the service(s) provided please contact: SPT McColl’s Travel Limited Bus Operations Block 4 131 St. Vincent St Vale of Leven Ind. Est. Glasgow G2 5JF Dumbarton G82 3PD t 0345 271 2405 0141 333 3690 t 01389 754 321 e [email protected] e [email protected] Please note – Calls to 0845 271 2405 will be charged at 2p per min (inc. VAT) plus your Telecoms Providers Access Charge Service 340 Helensburgh – Vale of Leven Hospital – Royal Alexandra Hospital Operated by McColl’s Travel Limited on behalf of SPT Route Service 340: from Helensburgh Rail Station via Princes Street East, Sinclair Street, Luss Road, A818, Crosskeys Roundabout, A818 Arden Roundabout, A82, A811, Luss Road, North Main Street, Vale of Leven Hospital access road (clockwise), North Main Street, Bank Street, B857, Main Street, Lennox Street, Renton Road, Glasgow Road, High Street, Church Street, Glasgow Road, Dumbarton Road, Great Western Road, A898, Erskine Bridge, M898, M8, St James Interchange, A726, Greenock Road, Caledonia Street, Underwood Road, B7050, Maxwellton Street, Corsebar Road, access road to Paisley, Royal Alexandria Hospital. -
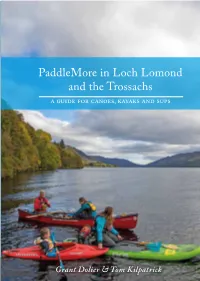
Paddlemore in Loch Lomond and the Trossachs a Guide for Canoes, Kayaks and Sups Paddlemore in Loch Lomond and the Trossachs a Guide for Canoes, Kayaks and Sups
PaddleMore in LochTrossachs PaddleMore Lomond and the PaddleMore in Loch Lomond and the Trossachs a guide for canoes, kayaks and sups PaddleMore in Loch Lomond and the Trossachs a guide for canoes, kayaks and sups Whether you want hardcore white water, multi-day touring Kilpatrick Tom & Dolier Grant trips or a relaxing afternoon exploring sheltered water with your family, you’ll find all that and much more in this book. Loch Lomond & The Trossachs National Park is long estab- lished as a playground for paddlers and attracts visitors from all over the world. Loch Lomond itself has over eighty kilometres of shoreline to explore, but there is so much more to the park. The twenty-two navigable lochs range from the vast sea lochs around Loch Long to small inland Loch Lomond bodies such as Loch Chon. & the Trossachs The rivers vary from relaxed meandering waterways like the Balvaig to the steep white water of the River Falloch and 9 781906 095765 everything in between. Cover – Family fun on Loch Earn | PaddleMore Back cover – Chatting to the locals, River Balvaig | PaddleMore Grant Dolier & Tom Kilpatrick Loch an Daimh Loch Tulla Loch Also available from Pesda Press Bridge of Orchy Lyon Loch Etive Loch Tay Killin 21b Tyndrum River Dochart River Loch 21a Fillan Iubhair Loch Awe 20 LOCH LOMOND & Crianlarich Loch Lochearnhead Dochart THE TROSSACHS 19 Loch NATIONAL PARK Earn Loch 5 River Doine 17 River Falloch Loch 32 Voil Balvaig 23 Ardlui 18 Loch Loch Sloy Lubnaig Loch Loch Katrine Arklet 12 Glen Finglas Garbh 3 10 Reservoir Uisge 22 Callander -

Essential NHS Information About Hospital Closures Affecting
ESSENTIAL NHS INFORMATION ABOUT HOSPITAL CLOSURES AFFECTING YOU Key details about your brand-new South Glasgow University Hospital and new Royal Hospital for Sick Children NHS GGC SGlas Campus_D.indd 1 31/03/2015 10:06 The new hospitals feature the most modern and best-designed healthcare facilities in the world Your new hospitals The stunning, world-class £842 million There is an optional outpatient self hospitals, we are closing the Western south Glasgow hospitals – South Glasgow check-in system to speed up patient flows. Infirmary, Victoria Infirmary including the University Hospital and the Royal Hospital On the first floor there is a 500-seat hot Mansionhouse Unit, Southern General and for Sick Children – are located on the food restaurant and a separate café. The Royal Hospital for Sick Children at Yorkhill. former Southern General Hospital bright and airy atrium features shops and The vast majority of services from campus in Govan. banking machines and a high-tech lift these hospitals will transfer to the new They will deliver local, regional and system that will automatically guide you south Glasgow hospitals, with the national services in some of the most to the lift that will take you to your remainder moving to Glasgow Royal modern and best-designed healthcare destination most quickly. Infirmary and some services into facilities in the world. Crucially, these two The children’s hospital features 244 Gartnavel General Hospital. brand-new hospitals are located next to a paediatric beds, with a further 12 neonatal Once these moves are complete, first-class and fully modernised maternity beds in the maternity unit next door. -

SLR I15 March April 03.Indd
scottishleftreview comment Issue 15 March/April 2003 A journal of the left in Scotland brought about since the formation of the t is one of those questions that the partial-democrats Scottish Parliament in July 1999 Imock, but it has never been more crucial; what is your vote for? Too much of our political culture in Britain Contents (although this is changing in Scotland) still sees a vote Comment ...............................................................2 as a weapon of last resort. Democracy, for the partial- democrat, is about giving legitimacy to what was going Vote for us ..............................................................4 to happen anyway. If what was going to happen anyway becomes just too much for the public to stomach (or if Bill Butler, Linda Fabiani, Donald Gorrie, Tommy Sheridan, they just tire of the incumbents or, on a rare occasion, Robin Harper are actually enthusiastic about an alternative choice) then End of the affair .....................................................8 they can invoke their right of veto and bring in the next lot. Tommy Sheppard, Dorothy Grace Elder And then it is back to business as before. Three million uses for a second vote ..................11 Blair is the partial-democrat par excellence. There are David Miller two ways in which this is easily recognisable. The first, More parties, more choice?.................................14 and by far the most obvious, is the manner in which he Isobel Lindsay views international democracy. In Blair’s world view, the If voting changed anything...................................16 purpose of the United Nations is not to make a reasoned, debated, democratic decision but to give legitimacy to the Robin McAlpine actions of the powerful. -

Prescribed Footwear Step 1 Wear for ½ Glasgow Royal Infirmary Hour
How to Contact Us Wearing Advice Call the referral management centre This footwear is for your use only. on: 0141 347 8909 or email: Your Orthotist or Health Care [email protected] Professional will advise you how This number should be used for all often to wear your footwear initially Advice about your and for how long. General advice is enquiries from the following clinics: included below. Gartnavel General Hospital Prescribed Footwear Step 1 Wear for ½ Glasgow Royal Infirmary hour. Queen Elizabeth University Step 2 1 hour Hospital New Stobhill Hospital Step 3 3 hours New Victoria Hospital Wear all day Vale of Leven Hospital Wear as needed Inverclyde Royal Hospital Further Information Royal Alexandra Hospital For further information please Renfrewshire Health and to go to Social Care Centre https://www.nhsggc.org.uk/your- health/health-services/orthotics/ Department of Orthotics Tel No: 0141 347 8909 Review Date: March 2022 • 203956A v2.1 Introduction Care of Your Footwear What to do if you have This leaflet provides basic It is important that you take good a Problem information on the correct use and care of your footwear, as this should • If you feel that your footwear care of your footwear. If you have maximise your comfort and make is uncomfortable. any further questions or concerns, them last longer. • If a fault develops (for example please contact us. Keep them clean and polish leather worn or broken straps). Skin Care shoes with a good quality polish. Contact us by calling To minimise the risk of problems If your footwear gets wet, pack with 0141 347 8909 to book a return occurring you should carry out newspaper and allow it to dry appointment. -

Inventory Acc.3721 Papers of the Scottish Secretariat and of Roland
Inventory Acc.3721 Papers of the Scottish Secretariat and of Roland Eugene Muirhead National Library of Scotland Manuscripts Division George IV Bridge Edinburgh EH1 1EW Tel: 0131-466 2812 Fax: 0131-466 2811 E-mail: [email protected] © Trustees of the National Library of Scotland Summary of Contents of the Collection: BOXES 1-40 General Correspondence Files [Nos.1-1451] 41-77 R E Muirhead Files [Nos.1-767] 78-85 Scottish Home Rule Association Files [Nos.1-29] 86-105 Scottish National Party Files [1-189; Misc 1-38] 106-121 Scottish National Congress Files 122 Union of Democratic Control, Scottish Federation 123-145 Press Cuttings Series 1 [1-353] 146-* Additional Papers: (i) R E Muirhead: Additional Files Series 1 & 2 (ii) Scottish Home Rule Association [Main Series] (iii) National Party of Scotland & Scottish National Party (iv) Scottish National Congress (v) Press Cuttings, Series 2 * Listed to end of SRHA series [Box 189]. GENERAL CORRESPONDENCE FILES BOX 1 1. Personal and legal business of R E Muirhead, 1929-33. 2. Anderson, J W, Treasurer, Home Rule Association, 1929-30. 3. Auld, R C, 1930. 4. Aberdeen Press and Journal, 1928-37. 5. Addressall Machine Company: advertising circular, n.d. 6. Australian Commissioner, 1929. 7. Union of Democratic Control, 1925-55. 8. Post-card: list of NPS meetings, n.d. 9. Ayrshire Education Authority, 1929-30. 10. Blantyre Miners’ Welfare, 1929-30. 11. Bank of Scotland Ltd, 1928-55. 12. Bannerman, J M, 1929, 1955. 13. Barr, Mrs Adam, 1929. 14. Barton, Mrs Helen, 1928. 15. Brown, D D, 1930. -

206 Bus Time Schedule & Line Route
206 bus time schedule & line map 206 Westcliff - Haldane View In Website Mode The 206 bus line (Westcliff - Haldane) has 5 routes. For regular weekdays, their operation hours are: (1) Dumbarton: 6:00 PM (2) Dumbarton: 7:20 PM (3) Haldane: 6:21 AM - 6:35 PM (4) Levenvale: 10:24 AM - 6:43 PM (5) Westcliff: 6:50 AM - 6:30 PM Use the Moovit App to ƒnd the closest 206 bus station near you and ƒnd out when is the next 206 bus arriving. Direction: Dumbarton 206 bus Time Schedule 47 stops Dumbarton Route Timetable: VIEW LINE SCHEDULE Sunday 11:11 AM - 6:11 PM Monday 6:05 PM Shandon Brae, Haldane Haldane Terrace, Scotland Tuesday 6:00 PM Mcgregor Avenue, Haldane Wednesday 6:00 PM Brown Street, Haldane Thursday 6:00 PM Friday 6:00 PM Main Street, Haldane Saturday 6:05 PM Smith Crescent, Balloch Balloch Bus Terminus, Balloch Carrochan Crescent, Balloch 206 bus Info Lomond Road, Alexandria Direction: Dumbarton Stops: 47 Ben Lomond Walk, Balloch Trip Duration: 30 min Line Summary: Shandon Brae, Haldane, Mcgregor Lomond Drive, Levenvale Avenue, Haldane, Brown Street, Haldane, Main Street, Haldane, Smith Crescent, Balloch, Balloch Bus Lomond Drive, Alexandria Terminus, Balloch, Carrochan Crescent, Balloch, Ben Cameron Drive, Tullichewan Lomond Walk, Balloch, Lomond Drive, Levenvale, Cameron Drive, Tullichewan, Broomley Crescent, Tullichewan, Cullen Street, Tullichewan, Mccoll Broomley Crescent, Tullichewan Avenue, Tullichewan, Bromley Crescent, Tullichewan, Craig Avenue, Alexandria Ambulance Station, Levenvale, King Edward Street, Alexandria, Wilson -

PPF 2017 MASTER.Pmd
WEST DUNBARTONSHIRE Planning and Perfomance Framework Planning and Building Standards Service July 2017 Planning Performance Framework Foreword This is the sixth reporting year of the an exciting opportunity for the service to be Dumbarton waterfront is also progressing Planning Performance Framework which in the heart of Council services and to work with three out of the four sites having outlines our performance and showcases in a modern purpose built Council office submitted detailed applications for our achievements and improvements in with A listed façade. The new Council development. 2016-17. It also outlines our service office is due to be opened on January Progress of these key development sites improvements for 2017-18. 2018. It will be good to occupy a building has put increased pressure on the service which our service has had a major influence Last year’s Planning Performance as we try to support the development of on its design. Framework was peer reviewed by Glasgow these sites with the same resources as City Council who are part of our Solace As this is the sixth Planning Performance before. The Service has been successful Benchmarking Group. This exercise was Framework I took the opportunity to revisit this year in securing the funding for a part- very useful with good feedback being our first Planning Performance Framework time Planning Compliance Officer and the received. This has helped to shape the back in September 2012. It was good to Strategic Lead of Regeneration has agreed format and content of this year’s Planning see how much progress has been made in to fund a Lead Planning Officer post for 2 Performance Framework.