Compassion Fatigue
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Enneagram-Type-2.Pdf
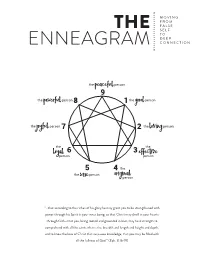
M O V I N G F R O M F A L S E THE S E L F T O D E E P ENNEAGRAM CONNECTION the PEACEFUL person 9 the POWERFUL person 8 1 the GOOD person the JOYFUL person 7 2 the LOVING person the 6 3 the LOYAL person EFFECTIVE person 5 4 the the person WISE ORIGINAL person “…that according to the riches of his glory he may grant you to be strengthened with power through his Spirit in your inner being, so that Christ may dwell in your hearts through faith—that you, being rooted and grounded in love, may have strength to comprehend with all the saints what is the breadth and length and height and depth, and to know the love of Christ that surpasses knowledge, that you may be filled with all the fullness of God.” (Eph. 3:16-19) In the early hours of April 15, 1912, on its maiden voyage from South Hampton to New York City, the Titanic sank when it collided “... THAT ACCORDING TO THE RICHES with an iceberg in the cold waters of the North Atlantic Ocean. OF HIS GLORY HE MAY GRANT Tragically, more than 1,500 people lost their lives. At the time, YOU TO BE STRENGTHENED WITH the Titanic was the largest, most well-built and luxurious ship ever POWER THROUGH HIS SPIRIT IN conceived. It was thought to be unsinkable. As one crew member YOUR INNER BEING ... TO KNOW THE reportedly said, “Not even God himself could sink this ship.” But LOVE OF CHRIST THAT SURPASSES what those aboard the Titanic didn’t know was that hidden beneath KNOWLEDGE .. -

We Value Humility) Pastor Dave Lomas, Reality San Francisco
Sermon Transcript from October 16th, 2016 God Is God and I’m Not (We Value Humility) Pastor Dave Lomas, Reality San Francisco We are in a series now on our vision statement. So, we're in a vision and values series that we started last week. Here's the vision of our church. If you are new to our church, if you've not been to Welcome to Reality or if you have been a part of this church but don't know it yet, here it is. Our vision statement, it's on our website and we communicate this all sorts of ways when we do events. It's like the grid that we see everything through as a church. Here it is. The first part of this has been our vision from the very beginning, since before the church was even started. This was the vision. Then, we added the second part of it just a couple years into the church. It's this: "We are a community following Jesus, seeking renewal in our city." A community following Jesus, seeking renewal in our city. I love that. I love the simplicity of it. I also think it's very profound as well. I hope that you would commit it to memory. A few years ago, we wanted to know what it would feel like in the culture of our church, in our lives, like felt experience or collective experience of what it would feel like to live into this vision. What would it be if that's the vision? We say that. -

“Me”: the Nature of Conceit
Living Word of the Buddha SDvol 19 no 2a “Me”: The nature of conceit “Me” The Nature of Conceit [The psychological complexes and narcissism] by Piya Tan ©2007 “What is in our mind appears more real than what is outside of it.” [7.5] 1 Complexes 1.1 STATUS AND CONCEIT. The Alagaddûpama Sutta (M 22) teaches that the five aggregates, each and every one of them, should be regarded as ‘This is not mine, this I am not, this is not my self.’1 These statements are the opposite of the threefold graspings (ti,vidha gāha), namely, “Thisismine” (etam mama) (arises through craving, tahā,gāha) = “mine-making”; “This I am” (eso’ham asmi) (arises through conceit, māna,gāha) = “conceit”;and “Thisismyself” (eso me attā) (arises through wrong view, dihi,gāha) = “I-making.” (Anattā,lakkhaa Sutta, S 3:68 = SD 1.2) These three wrong attitudes are also known as the “latent tendencies to ‘I’-making, ‘mine’-making and conceit” (aha.kāra,mama.kāra,mānnusaya).2 These threefold graspings are the main factors behind conception (maññana) (M 1) and mental proliferation (papañca) (M 18). In short, such experiences are not merely “beliefs” but are direct reactions to reality.3 In this essay, we shall discuss the second of the threefold graspings—that of “This I am” (eso’ham asmi)—which arises because of grasping through conceit (māna,gāha). When we hold the view, “This I am,” we are clinging to the notion of duality, that is, there is an “I” and “other” beyond the mere conven- tional usage of the words. -

Mediator Complex Or Empathy Sickness and Judge Complex
Case Report ERA’S JOURNAL OF MEDICAL RESEARCH VOL.8 NO.1 DOI:10.24041/ejmr2021.18 MEDIATOR COMPLEX OR EMPATHY SICKNESS AND JUDGE COMPLEX Ismael Tabuñar Fortunado Department of Industrial and Engineering Research National Research Council of the Philippines, University of Santo Tomas Philippines Received on : 31-05-2021 Accepted on : 05-06-2021 ABSTRACT Address for correspondence We put ourselves in others shoes. How often? Does it bring pain? Does it Dr. Ismael T. Fortunado affect our mood? Mediator is defined as a person who attempts to make Department of Industrial and people involved in a conflict come to an agreement; a go-between while Engineering Research complex is an abnormality, most often a serious one. Judge on the other University of Santo Tomas Philippines hand, decides cases. This is an introduction to a proposed complex wherein Email: [email protected] the author is admitted to have some symptoms of which may be considered. Contact no: +63-9952862597 That we often derive sorrow from the sorrow of others, is a matter of fact too obvious to require any instances to prove it. – Adam Smith KEYWORDS: Complex, Empathy Sickness, Judge complex, Mediator complex, Sickness. INTRODUCTION means, and professionals are often unwilling to use A god complex is an unshakable belief characterized the label because it is considered vague and by the consistently inflated feelings of personal ability, derogatory. (McIntosh 1989 and Alder 1992) Being privilege, or infallibility. A person with a god complex spoiled is not recognized as a mental disorder in any may refuse to admit the possibility of their error or of the medical manuals, such as the ICD-10 (Many failure, even in the face of irrefutable evidence, Authors 2021a) or the DSM-IV (Many Authors intractable problems or difficult or impossible tasks. -

Dark Lonerism: Self-Sabotage, Apathy, And
DARK LONERISM: SELF-SABOTAGE, APATHY, AND UNCANNY WHITENESS by CHRIS BOLLINI (Under the Direction of John Wharton Lowe) ABSTRACT Commenting on the literary trope of loneliness that can spark action or epiphany, Robert A. Ferguson accounts for the many “fables” in America about the “solitary adventurer and its social variant, the self-made man,” by suggesting individualism can be the “answer as well as the problem to feeling alone.” This dissertation explores a similar paradox: how can an intense self- interest, aloof to the struggles of others, become the answer as well as the problem to feeling disempowered? In a certain strain of American literature from the Great Depression through the early post-war period, depictions of the aloof and brooding male protagonist ironicize as much as they romanticize the angst of ensuring one’s integrity within a chaotic world. The irony exposed in such texts inevitably becomes layered and multivalent because the presence of a loner- protagonist creates a schism between external reality and his troubled, obsessive mindset. As this study argues, the loner-protagonist may stubbornly fantasize about opting out of society and seeking confirmation of his exceptional status, yet he can only test this sense of the world by deconstructing his preferred state of apartness, surveillance, and hypervigilance. Despite being tormented by his concessions to normativity as he enters the crucible of social life, the loner- protagonist capitalizes on the promise of control inherent in white privilege, or what this project conceptualizes as the masked persona of uncanny whiteness. By exposing the performative undercurrents to an otherwise austere and seemingly unknowable archetype, Dark Lonerism encompasses both a healthy skepticism of the loner-protagonist’s self-isolating pose and a sympathetic interrogation of the pathological psychology underlying his many acts of self- sabotage. -
Showing Compassion
A QUARTERLY PUBLICATION OF ADVENTIST CHAPLAINCY MINISTRIES ISSUE 2 2014 Showing Compassion PERSPECTIVE COMPASSION By Larry A. Roth, B.D. CORE INGREDIENT IN ALL Assistant Director, Adventist Chaplaincy Ministries CHAPLAINCY MINISTRIES Central and Northwest United States n every type of military personnel, inmates in prison chaplaincy ministry, and the many others in their own world Ifrom health care, have very different problems, but they corrections, campus are all human stories of despair. Of to the military, and course it isn’t only chaplains who hear many forms of local these stories. All personnel in these law enforcement, fire, institutions where people come for airport, and others, all institutions help, nurses, doctors, police, wardens, seek chaplains with the highest levels teachers, counselors, social workers, of compassion. and even parents, all hear troubling Compassion is more complex in stories, and are moved to provide help. definition than one at first expects. They all need compassion. And that is One dictionary defines compassion why the Greater Good Science Center as “a feeling of deep sympathy and and their team of researchers and sorrow for another who is stricken by educators have formed their center. misfortune, accompanied by a strong They are seeking and providing ways desire to alleviate the suffering.” for a wide group of professionals to The founders at the Greater Good better understand themselves and Science Center, UC Berkeley, say expand their capacities for compassion. that compassion simply means, “to Many if not most of the institutions suffer together.” This includes more we have mentioned have learned that than merely feeling sorry together, chaplains are the ones they call on but being committed to finding a to hear these deepest expressions of solution together. -

3. the Leadership Contest: an End to the 'Messiah Complex'?
3. The Leadership Contest: An end to the ‘messiah complex’? Paul Strangio and James Walter Prime Minister Kevin Rudd had only just fired the starting gun on the 2013 election campaign, but commentators were already in no doubt about the nature of the campaign that would unfold during the ensuing five weeks: ‘This federal election will be the most presidential in style, communications and frenzy in our history’ (Dusevic 2013). In Australia we have grown accustomed over recent decades to media representations of each national election as a new high water mark in ‘presidential’ campaigning. The 2013 campaign was certainly no exception; the term ‘presidential’ was a ubiquitous reference point for journalists, especially in their descriptions of the Labor Party’s pitch for re- election (see the controversy between Kefford and Dowding in theAustralian Journal of Political Science 2013). Given the tumultuous backstory to the election this was hardly surprising. While the roles of the executed and the executioner had been reversed in a reprisal of the dynamics of the 2010 federal poll, the 2013 election was announced within a handful of weeks of a party room coup to depose another Labor prime minister. On this occasion, caucus had voted to overthrow Julia Gillard and reinstate Kevin Rudd after a lengthy campaign of internal destabilisation by the Rudd-aligned forces (see Walsh 2013) against Gillard and escalating panic at published and internal opinion polling suggesting that the ALP faced electoral annihilation if it persisted with her leadership. If Gillard’s (2013) subsequent assessment of the rationale for her removal glossed over her missteps in office, she nonetheless was correct in her assertion that the party room had capitulated to Rudd’s apparent popularity: ‘it was not done because caucus now believed Kevin Rudd had the greater talent for governing … It was done—indeed expressly done—on the basis that Labor might do better at the election’. -

Know Thy Enemy Profiles of Adversary Leaders and Their Strategic Cultures
Know Thy Enemy Profiles of Adversary Leaders and Their Strategic Cultures Edited by Barry R. Schneider and Jerrold M. Post, eds. US Air Force Counterproliferation Center Maxwell Air Force Base, Alabama KNOW THY ENEMY Profiles of Adversary Leaders and Their Strategic Cultures Edited by Barry R. Schneider and Jerrold M. Post USAF Counterproliferation Center 325 Chennault Circle Maxwell Air Force Base, Alabama 36112-6427 July 2003 (Second Edition) Disclaimer The views expressed in this publication are those of the authors and do not necessarily reflect the official policy or position of the U.S. Government, Department of Defense, or the USAF Counterproliferation Center. For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: toll free (866) 512-1800; DC area (207) 512-1800 Fax: (202) 512-2250 Mail: Stop SSOP, Washington, DC 20401-0001 ISBN 0-9747403-0-6 ii Contents Chapter Page Disclaimer .............................................................................................. ii Acknowledgments...................................................................................v 1 Deterring International Rivals From War and Escalation .......................1 Barry R. Schneider 2 Killing In The Name of God: Osama Bin Laden and Al Qaeda...........17 Jerrold M. Post 3 The Muslim Brotherhood and Islamic Radicalism................................41 Gary M. Servold 4 Struggle for the Control of Pakistan: Musharraf Takes On the Islamist Radicals ...........................................85 -

Understanding Madmen: a DSM-IV Assessment of Adolf Hitler
Individual Differences Research www.idr-journal.com 2007, Vol. 5, No. 1 ISSN: 1541-745X pp. 30-43 Copyright © 2007 IDR Understanding Madmen: A DSM-IV Assessment of Adolf Hitler Frederick L. Coolidge*, Felicia L. Davis, & Daniel L. Segal University of Colorado at Colorado Springs *Frederick L. Coolidge, PhD; Psychology Department; P. O. Box 7150; University of Colorado at Colorado Springs; Colorado Springs, CO 80933-7150; [email protected] (email). ABSTRACT - Adolf Hitler’s personality was investigated posthumously through the use of an informant version of the Coolidge Axis II Inventory (CATI), which is designed for the assessment of personality, clinical, and neuropsychological disorders. Five academic Hitler historians completed the CATI. The overall mean inter-rater correlation was moderately high for all 38 CATI scales’ T scores (median r = .72). On Axis I, the highest mean T scores across raters were Posttraumatic Stress Disorder (76), Psychotic Thinking (73) and Schizophrenia (69). On Axis II, the highest mean T scores were Paranoid Personality Disorder (78), Antisocial Personality Disorder (78), Narcissistic Personality Disorder (77), and Sadistic Personality Disorder (76). Results of the present study support the reliability and preliminary validity of informant reports for psychological investigations of historical or contemporary figures. The name Adolf Hitler conjures-up images of a madman in power, Nazi concentration camps in Germany and Europe, and an evil of such magnitude that millions of Jewish people and others were subjected to unimaginable torture, terror and death. The present study attempts to evaluate posthumously Adolf Hitler’s personality according to the current Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2000). -

University of Huddersfield Repository
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Huddersfield Repository University of Huddersfield Repository Hyland, Philip, Boduszek, Daniel and Kielkiewicz, Krzysztof Psycho-Historical Analysis of Adolf Hitler: the Role of Personality, Psychopathology and Development Original Citation Hyland, Philip, Boduszek, Daniel and Kielkiewicz, Krzysztof (2011) Psycho-Historical Analysis of Adolf Hitler: the Role of Personality, Psychopathology and Development. Psychology and Society, 42 (2). pp. 58-63. ISSN 2041-5893 This version is available at http://eprints.hud.ac.uk/15881/ The University Repository is a digital collection of the research output of the University, available on Open Access. Copyright and Moral Rights for the items on this site are retained by the individual author and/or other copyright owners. Users may access full items free of charge; copies of full text items generally can be reproduced, displayed or performed and given to third parties in any format or medium for personal research or study, educational or not-for-profit purposes without prior permission or charge, provided: • The authors, title and full bibliographic details is credited in any copy; • A hyperlink and/or URL is included for the original metadata page; and • The content is not changed in any way. For more information, including our policy and submission procedure, please contact the Repository Team at: [email protected]. http://eprints.hud.ac.uk/ A Psycho-Historical Analysis of Adolf Hitler: The Role of Personality, Psychopathology, and Development PHILIP HYLAND University Of Ulster DANIEL BODUSZEK University Of Ulster KRZYSZTOF KIELKIEWICZ All Hallows College Abstract The present paper presents a psycho-historical analysis of Adolf Hitler with reference to multiple psychological theories which attempts to briefly elucidate the contributing personality and psychosocial developmental factors that likely contributed to the development of severe psychopathology. -

Counseling in the Urban Church
HEALING FOR THE CITY Counseling in the Urban Setting Craig W. Ellison & Edward S. Maynard Chapter III- Counseling in the Urban Church Copyright 1992 Used by permission of Zondervan Publishing House, Grand Rapids, Michigan CHURCHES AND PARACHURCH settings offer a variety of healing intervention possibilities that traditional professional counseling does not. In this chapter we will answer such questions as: Are counseling and discipleship related? What is the possible role of the laity? Are preaching and counseling complementary or conflicting? What can the urban church do in the way of preventive counseling? What are the limitations of the counselor? COUNSELING AND DISCIPLESHIP At first glance, counseling and discipleship do not seem to be closely related.1 Counseling has to do with helping people straighten out the emotional and relational distortions of their lives when they are unable to find constructive ways to cope with pain. They are usually experiencing intense negative emotions or emotional numbing and they are trying to clarify confusion, find comfort, or somehow bring about changes in their experience of life. Discipleship, on the other hand, has to do with the development of a person from spiritual infancy to spiritual adulthood. It is a process of spiritual parenting and spiritual formation that we usually do not view in terms of pain and crisis, but in terms of growth. When we look more closely, however, the differences between counseling and discipleship may not be as discrete as they appear. Ministry in the urban setting presents us with the reality of suffering—a reality that the suburban church has not had to face to the same degree. -

Abstract the X-Men and Stereotypes of Dominant
ABSTRACT THE X-MEN AND STEREOTYPES OF DOMINANT AND SUBORDINATE GROUPS This study examined the use of stereotypes in the graphic novel X-Men: Messiah Complex. Taking both quantitative and qualitative approaches to analyzing content, the author found that the X-Men characters that appeared most frequently and most often in positions of leadership were White heterosexual males. Female and racial minority X-Men characters appeared least frequently and most often as followers. Sexual minorities did not appear at all. These patterns of representation are reflective of patterns found in other media, which tend to focus on and emphasize the positive qualities of members of dominant groups while ignoring or negatively portraying members of subordinate ones. This research discovered that racial and religious themes often strengthened or provided a backdrop for these stereotypes. Grant George Bedrosian December 2011 THE X-MEN AND STEREOTYPES OF DOMINANT AND SUBORDINATE GROUPS by Grant George Bedrosian A thesis submitted in partial fulfillment of the requirements for the degree of Master of Arts in Mass Communication and Journalism in the College of Arts and Humanities California State University, Fresno December 2011 APPROVED For the Department of Mass Communication and Journalism: We, the undersigned, certify that the thesis of the following student meets the required standards of scholarship, format, and style of the university and the student's graduate degree program for the awarding of the master's degree. Grant George Bedrosian Thesis Author Kelley McCoy (Chair) Mass Communication and Journalism Tamyra Pierce Mass Communication and Journalism Brian Agbayani Linguistics For the University Graduate Committee: Dean, Division of Graduate Studies AUTHORIZATION FOR REPRODUCTION OF MASTER’S THESIS X I grant permission for the reproduction of this thesis in part or in its entirety without further authorization from me, on the condition that the person or agency requesting reproduction absorbs the cost and provides proper acknowledgment of authorship.