Cdr Clinical Review Report for Incruse Ellipta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
New Zealand Data Sheet
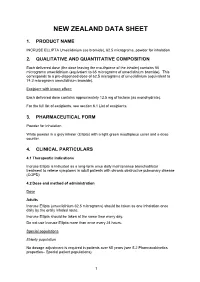
NEW ZEALAND DATA SHEET 1. PRODUCT NAME INCRUSE ELLIPTA Umeclidinium (as bromide), 62.5 micrograms, powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 55 micrograms umeclidinium (equivalent to 65 micrograms of umeclidinium bromide). This corresponds to a pre-dispensed dose of 62.5 micrograms of umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide). Excipient with known effect: Each delivered dose contains approximately 12.5 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for Inhalation White powder in a grey inhaler (Ellipta) with a light green mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Incruse Ellipta is indicated as a long-term once daily maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). 4.2 Dose and method of administration Dose Adults Incruse Ellipta (umeclidinium 62.5 micrograms) should be taken as one inhalation once daily by the orally inhaled route. Incruse Ellipta should be taken at the same time every day. Do not use Incruse Ellipta more than once every 24 hours. Special populations Elderly population No dosage adjustment is required in patients over 65 years (see 5.2 Pharmacokinetics properties– Special patient populations). 1 Renal impairment No dosage adjustment is required in patients with renal impairment (see 5.2 Pharmacokinetics properties – Special patient populations). Hepatic impairment No dosage adjustment is required in patients with mild or moderate hepatic impairment. Incruse Ellipta has not been studied in patients with severe hepatic impairment (see 5.2 Pharmacokinetics properties– Special patient populations). -

Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5
ANTICHOLINERGICS: Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5 J Bareham BSP © www.RxFiles.ca Aug 2021 WHENEVER POSSIBLE, AVOID DRUGS WITH MODERATE TO HIGH ANTICHOLINERGIC ACTIVITY IN OLDER ADULTS (>65 YEARS OF AGE) Low Anticholinergic Activity; Moderate/High Anticholinergic Activity -B in combo Beers Antibiotics Antiparkinsonian Cardiovascular Agents Immunosuppressants ampicillin *ALL AVAILABLE AS amantadine SYMMETREL atenolol TENORMIN azaTHIOprine IMURAN cefOXitin GENERIC benztropine mesylate COGENTIN captopril CAPOTEN cyclosporine NEORAL clindamycin bromocriptine PARLODEL chlorthalidone GENERIC ONLY hydrocortisone CORTEF gentamicin (Oint & Sol’n NIHB covered) carbidopa/levodopa SINEMET digoxin LANOXIN, TOLOXIN methylprednisolone MEDROL piperacillin entacapone COMTAN dilTIAZem CARDIZEM, TIAZAC prednisone WINPRED dipyridamole PERSANTINE, ethopropazine PARSITAN vancomycin phenelzine NARDIL AGGRENOX disopyramide RYTHMODAN Muscle Relaxants pramipexole MIRAPEX Antidepressants baclofen LIORESAL ( on intrathecal only) procyclidine KEMADRIN furosemide LASIX amitriptyline ELAVIL cyclobenzaprine FLEXERIL selegiline ELDEPRYL hydrALAZINE APRESOLINE clomiPRAMINE ANAFRANIL isosorbide ISORDIL methocarbamol ROBAXIN OTC trihexyphenidyl ARTANE desipramine NORPRAMIN metoprolol LOPRESOR orphenadrine NORFLEX OTC doxepin >6mg SINEQUAN Antipsychotics NIFEdipine ADALAT tiZANidine ZANAFLEX A imipramine TOFRANIL quiNIDine GENERIC ONLY C ARIPiprazole ABILIFY & MAINTENA -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME TRELEGY ELLIPTA 100/62.5/25 fluticasone furoate (100 micrograms)/umeclidinium (as bromide) (62.5 micrograms)/vilanterol (as trifenatate) (25 micrograms), powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 92 micrograms fluticasone furoate, 55 micrograms umeclidinium (equivalent to 65 micrograms umeclidinium [as bromide]) and 22 micrograms vilanterol (as trifenatate). This corresponds to a pre-dispensed dose of 100 micrograms fluticasone furoate, 62.5 micrograms umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide) and 25 micrograms vilanterol (as trifenatate). Excipient with known effect: Each delivered dose contains approximately 25 milligrams of lactose (as monohydrate). For the full list of excipients, see Section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for inhalation. White powder in a light grey inhaler (Ellipta) with a beige mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications TRELEGY ELLIPTA is indicated for the maintenance treatment of adults with moderate to severe chronic obstructive pulmonary disease (COPD) who require treatment with a long- acting muscarinic receptor antagonist (LAMA) + long-acting beta2-receptor agonist (LABA) + inhaled corticosteroid (ICS). TRELEGY ELLIPTA should not be used for the initiation of COPD treatment. 4.2. Dose and method of administration Patients can be changed from their existing inhalers to TRELEGY ELLIPTA at the next dose. However it is important that patients do not take other LABA or LAMA or ICS while taking TRELEGY ELLIPTA. A stepwise approach to the management of COPD is recommended, including the cessation of smoking and a pulmonary rehabilitation program. -

FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting
FDA Briefing Document Pulmonary-Allergy Drugs Advisory Committee Meeting August 31, 2020 sNDA 209482: fluticasone furoate/umeclidinium/vilanterol fixed dose combination to reduce all-cause mortality in patients with chronic obstructive pulmonary disease NDA209482/S-0008 PADAC Clinical and Statistical Briefing Document Fluticasone furoate/umeclidinium/vilanterol fixed dose combination for all-cause mortality DISCLAIMER STATEMENT The attached package contains background information prepared by the Food and Drug Administration (FDA) for the panel members of the advisory committee. The FDA background package often contains assessments and/or conclusions and recommendations written by individual FDA reviewers. Such conclusions and recommendations do not necessarily represent the final position of the individual reviewers, nor do they necessarily represent the final position of the Review Division or Office. We have brought the supplemental New Drug Application (sNDA) 209482, for fluticasone furoate/umeclidinium/vilanterol, as an inhaled fixed dose combination, for the reduction in all-cause mortality in patients with COPD, to this Advisory Committee in order to gain the Committee’s insights and opinions, and the background package may not include all issues relevant to the final regulatory recommendation and instead is intended to focus on issues identified by the Agency for discussion by the advisory committee. The FDA will not issue a final determination on the issues at hand until input from the advisory committee process has been considered -

Drug Tariff Part VIIIA December 2019
12/2019 Part VIIIA BASIC PRICES OF DRUGS Drug Quantity Basic Price Category Part VIIIA - Basic Prices of Drugs Product List Part VIIIA products A Abacavir 600mg / Lamivudine 30 19000 C Lupin Healthcare 300mg tablets (UK) Ltd Abatacept 125mg/1ml solution for 4 120960 C Orencia ClickJect injection pre-filled disposable devices Abatacept 125mg/1ml solution for 4 120960 C Orencia injection pre-filled syringes Acacia spray dried powder 250 g 1632 C J M Loveridge Ltd Acamprosate 333mg gastro- 168 3770 K A resistant tablets Acarbose 100mg tablets 90 2529 A Acarbose 50mg tablets 90 1458 A Acebutolol 100mg capsules 84 1497 C Sectral Acebutolol 200mg capsules 56 1918 C Sectral Acebutolol 400mg tablets 28 1862 C Sectral Aceclofenac 100mg tablets 60 962 A Acenocoumarol 1mg tablets 100 462 C Sinthrome Acetazolamide 250mg modified- 30 1666 C Diamox SR release capsules Acetazolamide 250mg tablets 112 1029 M Acetic acid 2% ear spray S 5ml 410 C EarCalm Acetone liquid 50 ml 112 A Acetylcysteine 200mg oral powder 30 11250 A sachets sugar free Acetylcysteine 2g/10ml solution for 10 2126 C Martindale infusion ampoules Pharmaceuticals Ltd Acetylcysteine 5% eye drops S 10 ml 3346 C Ilube Acetylcysteine 600mg capsules 30 3998 A Acetylcysteine 600mg effervescent 30 550 C tablets sugar free Aciclovir 200mg dispersible tablets 25 147 A Aciclovir 200mg tablets 25 133 M Aciclovir 200mg/5ml oral 125 ml 3578 A suspension sugar free Aciclovir 3% eye ointment S 4.5 g 934 C Zovirax Aciclovir 400mg dispersible tablets 56 1199 A Aciclovir 400mg tablets 56 310 M Aciclovir -

(Lamas) a New Frontier for COPD and Asthma Treatment
White Paper Long-Acting Muscarinic Agents (LAMAs) A New Frontier for COPD and Asthma Treatment LAMAs in Asthma and COPD Table of Contents 1. Introduction ............................................................................................. 3 2. Tiotropium Bromide ................................................................................. 4 3. Tiotropium + Olodaterol .......................................................................... 7 4. Aclidinium Bromide ................................................................................. 8 5. Aclidinium + Formoterol (ACLIFORM) ....................................................... 9 6. Glycopyrronium Bromide ....................................................................... 10 © 7. Glycopyrronium Bromide + Indacaterol (ULTIBRO )............................... 11 8. Glycopyrronium Bromide + Formoterol .................................................. 13 9. Umeclidinium ........................................................................................ 13 10. Umeclidinium + Vilanterol ..................................................................... 14 11. Triple Therapy ........................................................................................ 16 12. Conclusions ............................................................................................ 16 13. About the Author ................................................................................... 17 14. About CROMSOURCE ............................................................................ -

Pipelinetr Ends
June 2011 PIPELINE TRxENDS PIPELINE TR ENDS is produced by the x 1-3 Promising New Agents 5 Industry Trends University of Massachusetts Medical School’s 4 Projected Generic Entry 5 Additional Promising Clinical Pharmacy Services division and 4 Investigational Indications New Agents distributed to our clients twice yearly. 4 FDA Updates In This Issue Promising New Promising New Agents Agents Aflibercept Drug Name: Aclidinium bromide Drug Name: Aflibercept BLA submitted Manufacturer: Almirall, Forest Manufacturer: Regeneron, Bayer for wet age- Phase III Indication: COPD BLA Indication: Wet AMD related macular Formulation: Dry powder inhaler Formulation: Intravitreal injection degeneration Dimethyl fumarate Aclidinium bromide, a long-acting, inhaled Aflibercept is under FDA review for the treatment NDA submission anticholinergic bronchodilator, is an antagonist at of the neovascular form of age-related macular planned for the M2 and M3 muscarinic receptors. It is being degeneration (wet AMD). By inhibiting vascular relapsing-remitting multiple sclerosis studied for the treatment of chronic obstructive endothelial and placental growth factors, aflibercept pulmonary disease (COPD). may reduce the abnormal growth of blood vessels Projected Three Phase III, randomized, double-blind trials that damage the retina through blood and fluid leaks. Generic Entry compared aclidinium bromide 200 μg and 400 μg In two double-blind, non-inferiority, Phase III ® Nasacort AQ twice daily to placebo in patients with moderate to studies, VIEW 1 (N=1,217) and VIEW 2 (N=1,240), Levaquin® severe COPD. In each study, the primary endpoint patients with wet AMD were randomized to Uroxatral® Anzemet® was the change in morning trough forced expiratory intravitreal aflibercept 0.5 mg monthly, 2 mg monthly, Zyprexa® volume in one second (FEV1), from baseline to week or 2 mg every two months following three monthly Zyprexa® Zydis® 12. -

Profile of Aclidinium Bromide in the Treatment of Chronic Obstructive Pulmonary Disease
International Journal of COPD Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Profile of aclidinium bromide in the treatment of chronic obstructive pulmonary disease Michael W Sims Abstract: Bronchodilators provide the mainstay of pharmacologic therapy for chronic Reynold A Panettieri, Jr. obstructive pulmonary disease (COPD), and anticholinergic bronchodilators, in particular, appear to be the most effective. There are currently two anticholinergic agents available in the US for Pulmonary, Allergy, and Critical Care Division, Airways Biology Initiative, the treatment of COPD (ipratropium bromide and tiotropium bromide), but several others are Department of Medicine, University in various stages of development. Aclidinium bromide, a novel, long-acting, anticholinergic of Pennsylvania School of Medicine, Philadelphia, PA, USA bronchodilator, is currently in Phase III trials for the management of COPD. Available evidence suggests that aclidinium is a safe and well tolerated drug with a relatively rapid onset and a sufficient duration of action to provide once-daily dosing. This article will provide a pharma- cologic profile of aclidinium bromide and review the preclinical and clinical studies evaluating its safety and efficacy in the treatment of COPD. Keywords: aclidinium bromide, bronchodilators, pulmonary disease, chronic obstructive, muscarinic antagonists, pharmacokinetics, pharmacology Introduction Chronic obstructive pulmonary disease (COPD) is characterized, in part, by chronic airflow -

2021 Formulary List of Covered Prescription Drugs
2021 Formulary List of covered prescription drugs This drug list applies to all Individual HMO products and the following Small Group HMO products: Sharp Platinum 90 Performance HMO, Sharp Platinum 90 Performance HMO AI-AN, Sharp Platinum 90 Premier HMO, Sharp Platinum 90 Premier HMO AI-AN, Sharp Gold 80 Performance HMO, Sharp Gold 80 Performance HMO AI-AN, Sharp Gold 80 Premier HMO, Sharp Gold 80 Premier HMO AI-AN, Sharp Silver 70 Performance HMO, Sharp Silver 70 Performance HMO AI-AN, Sharp Silver 70 Premier HMO, Sharp Silver 70 Premier HMO AI-AN, Sharp Silver 73 Performance HMO, Sharp Silver 73 Premier HMO, Sharp Silver 87 Performance HMO, Sharp Silver 87 Premier HMO, Sharp Silver 94 Performance HMO, Sharp Silver 94 Premier HMO, Sharp Bronze 60 Performance HMO, Sharp Bronze 60 Performance HMO AI-AN, Sharp Bronze 60 Premier HDHP HMO, Sharp Bronze 60 Premier HDHP HMO AI-AN, Sharp Minimum Coverage Performance HMO, Sharp $0 Cost Share Performance HMO AI-AN, Sharp $0 Cost Share Premier HMO AI-AN, Sharp Silver 70 Off Exchange Performance HMO, Sharp Silver 70 Off Exchange Premier HMO, Sharp Performance Platinum 90 HMO 0/15 + Child Dental, Sharp Premier Platinum 90 HMO 0/20 + Child Dental, Sharp Performance Gold 80 HMO 350 /25 + Child Dental, Sharp Premier Gold 80 HMO 250/35 + Child Dental, Sharp Performance Silver 70 HMO 2250/50 + Child Dental, Sharp Premier Silver 70 HMO 2250/55 + Child Dental, Sharp Premier Silver 70 HDHP HMO 2500/20% + Child Dental, Sharp Performance Bronze 60 HMO 6300/65 + Child Dental, Sharp Premier Bronze 60 HDHP HMO -

PRAC Draft Agenda of Meeting 11-14 May 2020
11 May 2020 EMA/PRAC/257460/2020 Human Division Pharmacovigilance Risk Assessment Committee (PRAC) Draft agenda for the meeting on 11-14 May 2020 Chair: Sabine Straus – Vice-Chair: Martin Huber 11 May 2020, 10:30 – 19:30, via teleconference 12 May 2020, 08:30 – 19:30, via teleconference 13 May 2020, 08:30 – 19:30, via teleconference 14 May 2020, 08:30 – 16:00, via teleconference Organisational, regulatory and methodological matters (ORGAM) 28 May 2020, 09:00-12:00, via teleconference Disclaimers Some of the information contained in this agenda is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also change during the course of the review. Additional details on some of these procedures will be published in the PRAC meeting highlights once the procedures are finalised. Of note, this agenda is a working document primarily designed for PRAC members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the agenda cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on-going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006, Rev. 1). Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

IEHP Dualchoice Cal Mediconnect Formulary Maintenance Drug List
IEHP DualChoice Cal MediConnect (Medicare-Medicaid Plan) Formulary Maintenance Drug List The following formulary medications may be approvable up to a three-month supply. Certain medications on this list may require prior approval from the plan based on existing criteria before being covered. For coverage information please see our formulary located on our website. BRAND GENERIC STREGTH DOSAGE FORM ABACAVIR ABACAVIR SULFATE 300 MG TABLET ABACAVIR ABACAVIR SULFATE 20 MG/ML SOLUTION TRIUMEQ ABACAVIR SULFATE/DOLUTEGRAVIR 600-50-300 TABLET SODIUM/LAMIVUDINE ABACAVIR-LAMIVUDINE ABACAVIR SULFATE/LAMIVUDINE 600-300MG TABLET ABACAVIR-LAMIVUDINE- ABACAVIR SULFATE/LAMIVUDINE/ZIDOVUDINE 150-300 MG TABLET ZIDOVUDINE TYMLOS ABALOPARATIDE 80MCG/DOSE PEN INJCTR ORENCIA ABATACEPT 125 MG/ML SYRINGE ORENCIA CLICKJECT ABATACEPT 125 MG/ML AUTO INJCT ORENCIA ABATACEPT 50MG/0.4ML SYRINGE ORENCIA ABATACEPT 87.5MG/0.7 SYRINGE VERZENIO ABEMACICLIB 50 MG TABLET VERZENIO ABEMACICLIB 100 MG TABLET VERZENIO ABEMACICLIB 150 MG TABLET VERZENIO ABEMACICLIB 200 MG TABLET ABIRATERONE ACETATE ABIRATERONE ACETATE 500 MG TABLET ABIRATERONE ACETATE ABIRATERONE ACETATE 250 MG TABLET YONSA ABIRATERONE ACETATE, SUBMICRONIZED 125 MG TABLET CALQUENCE ACALABRUTINIB 100 MG CAPSULE ACAMPROSATE CALCIUM ACAMPROSATE CALCIUM 333 MG TABLET DR ACARBOSE ACARBOSE 25 MG TABLET ACARBOSE ACARBOSE 50 MG TABLET ACARBOSE ACARBOSE 100 MG TABLET ACEBUTOLOL HCL ACEBUTOLOL HCL 200 MG CAPSULE ACEBUTOLOL HCL ACEBUTOLOL HCL 400 MG CAPSULE ACETAZOLAMIDE ER ACETAZOLAMIDE 500 MG CAPSULE ER ACETAZOLAMIDE