New Zealand Data Sheet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Effect of Indacaterol, a Novel Long-Acting Beta 2
ERJ Express. Published on November 29, 2006 as doi: 10.1183/09031936.00032806 EFFECT OF INDACATEROL, A NOVEL LONG-ACTING BETA 2-AGONIST, ON HUMAN ISOLATED BRONCHI Emmanuel Naline (1), Alexandre Trifilieff (2), Robin A. Fairhurst (2), Charles Advenier (1), Mathieu Molimard (3) (1) Research Unit EA220, Université de Versailles, Faculté de Médecine, Pharmacology, Hôpital Foch, 40 rue Worth, 92150 Suresnes, France (2) Novartis Institute for BioMedical Research, Horsham, England (3) Département de Pharmacologie, Université Victor Segalen Bordeaux 2; CHU Pellegrin; INSERM U657, Bordeaux, France Correspondence: Mathieu Molimard Département de Pharmacologie CHU de Bordeaux - Université Victor Segalen-INSERM U657 33076 Bordeaux cedex, France Phone: 33 (0)5 57 57 15 60 Fax: 33 (0)5 57 57 46 71 E-mail: [email protected] Short title: Indacaterol effect on isolated human bronchi 1 Copyright 2006 by the European Respiratory Society. Abstract Indacaterol is a novel β2-adrenoceptor agonist in development for the once-daily treatment of asthma and COPD. This study evaluated the relaxant effect of indacaterol on isolated human bronchi obtained from lungs of patients undergoing surgery for lung carcinoma. Potency (-logEC50), intrinsic efficacy (Emax) and onset of action were determined at resting tone. Duration of action was determined against cholinergic neural contraction induced by electrical field stimulation (EFS). At resting tone, -logEC50 and Emax values were, respectively, 8.82±0.41 and 77±5% for indacaterol, 9.84±0.22 and 94±1% for formoterol, 8.36±0.16 and 74±4% for salmeterol, and 8.43±0.22 and 84±4% for salbutamol. In contrast to salmeterol, indacaterol did not antagonize the isoprenaline response. -

Trimbow, INN-Beclometasone / Formoterol / Glycopyrronium Bromide
23 May 2017 EMA/CHMP/290028/2017 – Rev 1 Committee for Medicinal Products for Human Use (CHMP) Summary of opinion1 (initial authorisation) Trimbow beclometasone / formoterol / glycopyrronium bromide On 18 May 2017, the Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Trimbow, intended for the maintenance treatment of moderate to severe chronic obstructive pulmonary disease (COPD). The applicant for this medicinal product is Chiesi Farmaceutici S.p.A., Italy. Trimbow is a triple combination of an inhaled glucocorticoid (beclometasone dipropionate), a long-acting beta2 receptor agonist (formoterol fumarate dihydrate) and a long-acting muscarinic antagonist (glycopyrronium bromide). It will be available as a pressurised metered dose inhaler delivering a solution with a nominal dose per actuation of 87 micrograms / 5 micrograms / 9 micrograms of the active substances respectively. Beclometasone reduces inflammation in the lungs, whereas formoterol and glycopyrronium produce relaxation of bronchial smooth muscle helping to dilate the airways and make breathing easier (ATC code: R03AL09). The benefits with Trimbow are its ability to relieve and prevent symptoms such as shortness of breath, wheezing and cough and to reduce exacerbations of COPD symptoms. The most common side effects of Trimbow are oral candidiasis, muscle spasm and dry mouth. The full indication is: “Maintenance treatment in adult patients with moderate to severe -

22518Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 22518Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) 7 CLINICAL PHARMACOLOGY REVIEW NDA: 22-518 Brand Name: Dulera Generic Name: Mometosone furoate / formoterol fumarate Indication: Asthma (b) (4) in adults and children 12 years of age and older Dosage Form: Inhalation aerosol Strengths: (b) (4) 100/5, 200/5 mcg Route of Administration: Oral Inhalation Dosing regimen: Two inhalations twice daily (morning and evening) Applicant: Schering-Plough and Novartis OCP Division: DCP2 Clinical Division: DPAP (OND-570) Submission Date: May 21, 2009 Reviewers: Ying Fan, Ph.D., Liang Zhao, Ph.D. Team Leader (Acting): Partha Roy, Ph. D. TABLE OF CONTENTS 1 EXECUTIVE SUMMARY.................................................................................................... 3 1.1 Recommendations ........................................................................................................................3 1.2 Phase IV commitments.................................................................................................................3 1.3 Summary of Clinical Pharmacology and Biopharmaceutics findings.....................................3 2 QUESTION BASED REVIEW............................................................................................. 9 2.1 General Attributes/Background..................................................................................................9 2.1.1 What is the pertinent regulatory background of DULERA? ..................................... -
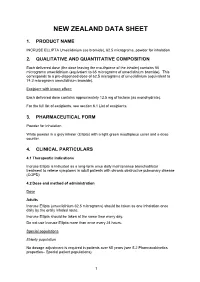
New Zealand Data Sheet
NEW ZEALAND DATA SHEET 1. PRODUCT NAME INCRUSE ELLIPTA Umeclidinium (as bromide), 62.5 micrograms, powder for inhalation 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each delivered dose (the dose leaving the mouthpiece of the inhaler) contains 55 micrograms umeclidinium (equivalent to 65 micrograms of umeclidinium bromide). This corresponds to a pre-dispensed dose of 62.5 micrograms of umeclidinium (equivalent to 74.2 micrograms umeclidinium bromide). Excipient with known effect: Each delivered dose contains approximately 12.5 mg of lactose (as monohydrate). For the full list of excipients, see section 6.1 List of excipients. 3. PHARMACEUTICAL FORM Powder for Inhalation White powder in a grey inhaler (Ellipta) with a light green mouthpiece cover and a dose counter. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Incruse Ellipta is indicated as a long-term once daily maintenance bronchodilator treatment to relieve symptoms in adult patients with chronic obstructive pulmonary disease (COPD). 4.2 Dose and method of administration Dose Adults Incruse Ellipta (umeclidinium 62.5 micrograms) should be taken as one inhalation once daily by the orally inhaled route. Incruse Ellipta should be taken at the same time every day. Do not use Incruse Ellipta more than once every 24 hours. Special populations Elderly population No dosage adjustment is required in patients over 65 years (see 5.2 Pharmacokinetics properties– Special patient populations). 1 Renal impairment No dosage adjustment is required in patients with renal impairment (see 5.2 Pharmacokinetics properties – Special patient populations). Hepatic impairment No dosage adjustment is required in patients with mild or moderate hepatic impairment. Incruse Ellipta has not been studied in patients with severe hepatic impairment (see 5.2 Pharmacokinetics properties– Special patient populations). -

Chronic Obstructive Lung Disease
Chronic Obstructive Lung Disease Amita Vasoya, DO FACOI FCCP FAASM Christiana Care Pulmonary Associates Clinical Assistant Professor of Medicine Sidney Kimmel Medical College of Thomas Jefferson University Rowan University School of Osteopathic Medicine ACOI Board Review 2019 Disclosures No Disclosures Obstructive Lung Diseases COPD Chronic ◦ Chronic Bronchitis Bronchitis Emphysema ◦ Emphysema Asthma Other ◦ Bronchiectasis Asthma ◦ Bronchiolitis ◦ Cystic Fibrosis ◦ Alpha 1 anti-trypsin deficiency Inter-relationship: Inflammation and Bronchial Hyperreactivity ATS GOLD CHEST 2002; 121: 121S-126S COPD THIRD leading cause of death worldwide It is the only leading cause of death whose prevalence is increasing! http://www.who.int/mediacentre/factsheets COPD Risk Factors Cigarette smoking Occupational exposures ◦ Silica, formaldehyde, toluene, nickel, cadmium, cotton, dust, etc Air pollution Biomass fuel Hyperresponsive airway Asthma Genetic factors Pathogenesis of COPD ATS Pulmonary Board Review 2015 Inflammatory Mediators: COPD ATS Pulmonary Board Review 2015 INFLAMMATION Small Airway Disease Parenchyma destruction Airway inflammation Loss of alveolar attachments Airway remodeling Decreased elastic recoil AIRFLOW LIMITATION ATS Pulmonary Board Review 2015 COPD Phenotypes Non-exacerbator Exacerbator with emphysema Exacerbator with chronic bronchitis Frequent exacerbator Alpha 1 Antitrypsin deficiency ACOS BCOS www.eclipse-copd.com, Lange P. Int J COPD 2016. 11: 3-12 Hurst JR. NEJM 2010. 363: 1128-38 Morphologic Types of -

Antiviral Effect of Budesonide Against SARS-Cov-2
viruses Communication Antiviral Effect of Budesonide against SARS-CoV-2 Natalie Heinen 1 , Toni Luise Meister 1 , Mara Klöhn 1 , Eike Steinmann 1, Daniel Todt 1,2 and Stephanie Pfaender 1,* 1 Department of Molecular and Medical Virology, Ruhr-University Bochum, 44801 Bochum, Germany; [email protected] (N.H.); [email protected] (T.L.M.); [email protected] (M.K.); [email protected] (E.S.); [email protected] (D.T.) 2 European Virus Bioinformatics Center (EVBC), 07743 Jena, Germany * Correspondence: [email protected]; Tel.: +49-234-32-23189 Abstract: Treatment options for COVID-19, a disease caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, are currently severely limited. Therefore, antiviral drugs that efficiently reduce SARS-CoV-2 replication or alleviate COVID-19 symptoms are urgently needed. Inhaled glucocorticoids are currently being discussed in the context of treatment for COVID-19, partly based on a previous study that reported reduced recovery times in cases of mild COVID-19 after inhalative administration of the glucocorticoid budesonide. Given various reports that describe the potential antiviral activity of glucocorticoids against respiratory viruses, we aimed to analyze a potential antiviral activity of budesonide against SARS-CoV-2 and circulating variants of concern (VOC) B.1.1.7 (alpha) and B.1.351 (beta). We demonstrate a dose-dependent inhibition of SARS-CoV-2 that was comparable between all viral variants tested while cell viability remains unaffected. Our results are encouraging as they could indicate a multimodal mode of action of budesonide against SARS-CoV-2 and COVID-19, which could contribute to an improved clinical performance. -

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Flonase Sensimist Allergy Relief (Fluticasone Furoate)
Flonase® Sensimist™ Allergy Relief (fluticasone furoate) – Rx-to-OTC Approval • On February 8, 2017, GlaxoSmithKline Consumer Healthcare announced the launch of Flonase Sensimist Allergy Relief (fluticasone furoate) nasal spray, as an over the counter (OTC) treatment to temporarily relieve symptoms of hay fever or other upper respiratory allergies: nasal congestion; runny nose; sneezing; itchy nose; and itchy, watery eyes (in ages 12 years and older). — Flonase Sensimist Allergy Relief contains 27.5 mcg/spray of fluticasone furoate. — Flonase Sensimist Allergy Relief should not be used in children less than 2 years of age. • Previously, fluticasone furoate was only available by prescription as Veramyst®. Veramyst is no longer commercially available. • Fluticasone is also available OTC as brand (Flonase® Allergy Relief, Children’s Flonase® Allergy Relief) and generic products containing 50 mcg/spray of fluticasone propionate. — These products share the same indications as Flonase Sensimist Allergy Relief, but are not intended for children under 4 years of age. • Prescription fluticasone propionate nasal spray (50 mcg/spray) is available generically and indicated for the management of the nasal symptoms of perennial non-allergic rhinitis in adult and pediatric patients aged 4 years and older. • Warnings for Flonase Sensimist Allergy Relief state the following: — Do not use: in children under 2 years of age, to treat asthma, if there is an injury or surgery to the nose that is not fully healed, or if an allergic reaction to Flonase Sensimist Allergy Relief or any of its ingredients has occurred. — Ask a doctor prior to use if the patient has or had glaucoma or cataracts. -

Beclometasone / Formoterol / Glycopyrronium Bromide Pressurised Metered Dose Inhaler (Trimbow®) for the Treatment of COPD
Beclometasone / formoterol / glycopyrronium bromide pressurised metered dose inhaler (Trimbow®) for the treatment of COPD Commissioning Statement Fylde and Wyre Clinical Commissioning Group has agreed to fund the prescribing of Beclometasone / formoterol / glycopyrronium bromide pressurised metered dose inhaler (Trimbow®) for the treatment of COPD Restriction: Triple therapy should be reserved for patients who have failed to achieve or maintain an adequate response to an appropriate course of dual therapy This medicine is classified as GREEN (Restricted) for this indication Summary of supporting evidence TRILOGY shows that in patients with COPD who have severe or very severe airflow limitation,symptoms, and an exacerbation history, triple therapy with BDP/FF/GB (beclomethasone dipropionate / formoterol fumarate / glycopyrronium bromide) had a greater effect on pre-dose and 2-h post-dose FEV1 than BDP/FF. For the co-primary endpoint measuring breathlessness (Transition Dyspnea Index, TDI), superiority of BDP/FF/GB over BDP/FF was not shown. The rate of moderate-to-severe COPD exacerbations was 23% lower with BDP/FF/GB compared with BDP/FF, with the time to first exacerbation significantly longer with triple therapy. Thus, the greater improvement in lung function with BDP/FF/GB compared with BDP/FF was more clearly accompanied by a reduction in exacerbations than an improvement in breathlessness in this group of patients. Furthermore, BDP/FF/GB had a greater effect on health related quality of life than BDP/FF. TRINITY met the primary and both key secondary endpoints. Extrafine fixed triple (i.e. extra fine inhaled particle fraction, ICS/LABA/LAMA in one inhaler) resulted in a 20% (95% CI 8– 31) reduction in the rate of moderate-to-severe COPD exacerbations compared with tiotropium, together with a 0·061L mean improvement in pre-dose FEV1. -

BREO • Do Not Use in Combination with an Additional Medicine Containing a ELLIPTA Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION treat acute symptoms. (5.2) These highlights do not include all the information needed to use BREO • Do not use in combination with an additional medicine containing a ELLIPTA safely and effectively. See full prescribing information for LABA because of risk of overdose. (5.3) BREO ELLIPTA. • Candida albicans infection of the mouth and pharynx may occur. Monitor patients periodically. Advise the patient to rinse his/her mouth with water BREO ELLIPTA 100/25 (fluticasone furoate 100 mcg and vilanterol without swallowing after inhalation to help reduce the risk. (5.4) 25 mcg inhalation powder), for oral inhalation • Increased risk of pneumonia in patients with COPD. Monitor patients for BREO ELLIPTA 200/25 (fluticasone furoate 200 mcg and vilanterol signs and symptoms of pneumonia. (5.5) 25 mcg inhalation powder), for oral inhalation • Potential worsening of infections (e.g., existing tuberculosis; fungal, Initial U.S. Approval: 2013 bacterial, viral, or parasitic infections; ocular herpes simplex). Use with caution in patients with these infections. More serious or even fatal course WARNING: ASTHMA-RELATED DEATH of chickenpox or measles can occur in susceptible patients. (5.6) See full prescribing information for complete boxed warning. • Risk of impaired adrenal function when transferring from systemic • Long-acting beta2-adrenergic agonists (LABA), such as vilanterol, corticosteroids. Taper patients slowly from systemic corticosteroids if increase the risk of asthma-related death. A placebo-controlled trial transferring to BREO ELLIPTA. (5.7) with another LABA (salmeterol) showed an increase in • Hypercorticism and adrenal suppression may occur with very high asthma-related deaths. This finding with salmeterol is considered a dosages or at the regular dosage in susceptible individuals. -

Fluticasone Furoate/Vilanterol 92/22 Μg Once-A-Day Vs Beclomethasone Dipropionate/Formoterol 100/6 Μg B.I.D
Open Access Journal of Pulmonology and Respiratory Research Research Article Fluticasone furoate/Vilanterol 92/22 μg once-a-day vs Beclomethasone dipropionate/Formoterol 100/6 μg b.i.d. in asthma patients: a 12-week pilot study Claudio Terzano* and Francesca Oriolo Respiratory Diseases Unit and School of Specialization in Respiratory Diseases Policlinico Umberto I, “Sapienza” University of Rome, Italy *Address for Correspondence: Dr Claudio Abstract Terzano, Respiratory Diseases Unit and School of Specialization in Respiratory Two of the most recent LABA/ICS combinations for treatment of persistent asthma are Fluticasone furoate/ Diseases Policlinico Umberto I, “Sapienza” Vilanterol 92/22 μg (Ellipta) and Beclomethasone dipropionate/Formoterol 100/6 μg (Nexthaler). University of Rome, Italy, Tel: 0649979051; Fax: 06499790675; Email: Objective: To compare once-daily Fluticasone/ Vilanterol combination with twice daily Beclomethasone/ [email protected] Formoterol association in moderate asthma, in terms of quality of life and lung function. Submitted: 08 September 2017 Methods: Fourty patients with moderate asthma treated with Beclomethasone/Formoterol 100/6 μg or Approved: 26 September 2017 Fluticasone/Vilanterol 92/22 μg. We revalued patients in terms of lung function and Asthma Control Test, at 4, 8 Published: 27 September 2017 and 12 weeks to assess any differences between the two groups. After 4 weeks, thirty-one of the fourty patients were evaluated in terms of respiratory function at predetermined time intervals. Copyright: 2017 Terzano C, et al. This is an open access article distributed under the Result: In patients treated with beclomethasone/formoterol FEV1 presented a mean value of 78% at the Creative Commons Attribution License, which third visit and of 79.1% during the fi nal check, compared with 74.5% and to 75.8% in patients in treatment permits unrestricted use, distribution, and with fl uticasone/vilanterol (p 0.01). -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020