CDR Pharmacoeconomic Review Report for Trelegy Ellipta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download Product Insert (PDF)
PRODUCT INFORMATION Piclamilast Item No. 29170 CAS Registry No.: 144035-83-6 Formal Name: 3-(cyclopentyloxy)-N-(3,5-dichloro- 4-pyridinyl)-4-methoxy-benzamide O Synonyms: RP 73401, RPR 73401 Cl H MF: C18H18Cl2N2O3 FW: 381.3 N O Purity: ≥98% O Supplied as: A solid N Storage: -20°C Cl Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Piclamilast is supplied as a solid. A stock solution may be made by dissolving the piclamilast in the solvent of choice, which should be purged with an inert gas. Piclamilast is soluble in organic solvents such as ethanol and DMSO. The solubility of piclamilast in ethanol is approximately 20 mM and approximately 100 mM in DMSO. Description 1 Piclamilast is a phosphodiesterase 4 (PDE4) inhibitor (IC50 = 0.31 nM). It is selective for PDE4 over PDE1, 2,3 PDE2, PDE3, PDE5, and PDE7A in cell-free assays (IC50s = >100, 40, >100, 14, and >10 μM, respectively). Piclamilast inhibits superoxide production by guinea pig eosinophils and histamine-induced contraction 1,4 in isolated guinea pig trachea (IC50s = 24 and 2 nM, respectively). It inhibits eosinophil, neutrophil, lymphocyte, and TNF-α accumulation in bronchoalveolar lavage fluid (BALF) from ovalbumin-sensitized 5 rats (ED50s = 23.8, 14.1, 19.5, and 14.4 μmol/kg, respectively). Piclamilast also inhibits ovalbumin-induced 2 bronchoconstriction in a guinea pig model of asthma (ED50 = 0.033 mg/kg). References 1. Ashton, M.J., Cook, D.C., Fenton, G., et al. Selective type IV phosphodiesterase inhibitors as antiasthmatic agents. -

A Comparison of Fluticasone Propionate, 1 Mg Daily, with Beclomethasone Dipropionate, 2 Mg Daily, in the Treatment of Severe Asthma
Copyright ©ERS Joumals Ltd 1993 Eur Respir J , 1993, 6, Sn-884 European Respiratory Joumal Printed in UK - all rights reserved ISSN 0903 - 1936 A comparison of fluticasone propionate, 1 mg daily, with beclomethasone dipropionate, 2 mg daily, in the treatment of severe asthma N.C. Bames*, G. Marone**, G.U. Di Maria***, S. Visser, I. Utama++, S.L. Payne+++, on behalf of an International Study Group A comparison of fluticasone propionate. 1 mg daily, with beclomethasone dipropionate, • The London Chest Hospital, London, 2 mg daily, in the treatment of severe asthma. N. C. Bames, G. Marone, G.U. Di Maria, UK. ** Servizio di Allergologia e S. Visser. l Utama, S.L Payne, on behalf of an International Study Group. @ERS Immunologia Clinica. I Clinica Medica Journals Ltd 1993. Universita, Napoli, Italy. *** lnstituto Malattie Respiratorie, Ospedale Tomaselli, ABSTRACT: We wanted w compare the efficacy and safety of fluticasone propi Catania, Sicily, Italy. onate, a new topically active inhaled corticosteroid, to that of high dose beclo + H.F. Verwoerd Hospital, Pretoria, South methasone dipropionate, in severe adult asthma. Africa. ++ St Laurentius Ziekenhius, 1 Patients currently receiving between 1.5-2.0 mg·day- of an inhaled corticoster CV Roermond, The Netherlands. +++ oid were treated for six weeks in a double-blind, randomized, parallel group study Glaxo Group Research Ltd, Greenford, with 1 mg·day-1 fluticasone propionate (n•82), or 2 mg·day·1 beclometbasone Middlesex, UK. dipropionate (n•72). Mean morning peak expirarory flow rates (PEFR) increased from 303 w 321 Correspondence: N.C. Bames l·min-1 with fluticasone propionate, and from 294 w 319 l·min·1 with beclometbasone The London Chest Hospital dipropionate. -

1 Effect of Indacaterol, a Novel Long-Acting Beta 2
ERJ Express. Published on November 29, 2006 as doi: 10.1183/09031936.00032806 EFFECT OF INDACATEROL, A NOVEL LONG-ACTING BETA 2-AGONIST, ON HUMAN ISOLATED BRONCHI Emmanuel Naline (1), Alexandre Trifilieff (2), Robin A. Fairhurst (2), Charles Advenier (1), Mathieu Molimard (3) (1) Research Unit EA220, Université de Versailles, Faculté de Médecine, Pharmacology, Hôpital Foch, 40 rue Worth, 92150 Suresnes, France (2) Novartis Institute for BioMedical Research, Horsham, England (3) Département de Pharmacologie, Université Victor Segalen Bordeaux 2; CHU Pellegrin; INSERM U657, Bordeaux, France Correspondence: Mathieu Molimard Département de Pharmacologie CHU de Bordeaux - Université Victor Segalen-INSERM U657 33076 Bordeaux cedex, France Phone: 33 (0)5 57 57 15 60 Fax: 33 (0)5 57 57 46 71 E-mail: [email protected] Short title: Indacaterol effect on isolated human bronchi 1 Copyright 2006 by the European Respiratory Society. Abstract Indacaterol is a novel β2-adrenoceptor agonist in development for the once-daily treatment of asthma and COPD. This study evaluated the relaxant effect of indacaterol on isolated human bronchi obtained from lungs of patients undergoing surgery for lung carcinoma. Potency (-logEC50), intrinsic efficacy (Emax) and onset of action were determined at resting tone. Duration of action was determined against cholinergic neural contraction induced by electrical field stimulation (EFS). At resting tone, -logEC50 and Emax values were, respectively, 8.82±0.41 and 77±5% for indacaterol, 9.84±0.22 and 94±1% for formoterol, 8.36±0.16 and 74±4% for salmeterol, and 8.43±0.22 and 84±4% for salbutamol. In contrast to salmeterol, indacaterol did not antagonize the isoprenaline response. -

Trimbow, INN-Beclometasone / Formoterol / Glycopyrronium Bromide
23 May 2017 EMA/CHMP/290028/2017 – Rev 1 Committee for Medicinal Products for Human Use (CHMP) Summary of opinion1 (initial authorisation) Trimbow beclometasone / formoterol / glycopyrronium bromide On 18 May 2017, the Committee for Medicinal Products for Human Use (CHMP) adopted a positive opinion, recommending the granting of a marketing authorisation for the medicinal product Trimbow, intended for the maintenance treatment of moderate to severe chronic obstructive pulmonary disease (COPD). The applicant for this medicinal product is Chiesi Farmaceutici S.p.A., Italy. Trimbow is a triple combination of an inhaled glucocorticoid (beclometasone dipropionate), a long-acting beta2 receptor agonist (formoterol fumarate dihydrate) and a long-acting muscarinic antagonist (glycopyrronium bromide). It will be available as a pressurised metered dose inhaler delivering a solution with a nominal dose per actuation of 87 micrograms / 5 micrograms / 9 micrograms of the active substances respectively. Beclometasone reduces inflammation in the lungs, whereas formoterol and glycopyrronium produce relaxation of bronchial smooth muscle helping to dilate the airways and make breathing easier (ATC code: R03AL09). The benefits with Trimbow are its ability to relieve and prevent symptoms such as shortness of breath, wheezing and cough and to reduce exacerbations of COPD symptoms. The most common side effects of Trimbow are oral candidiasis, muscle spasm and dry mouth. The full indication is: “Maintenance treatment in adult patients with moderate to severe -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

Intranasal Rhinitis Agents
Intranasal Rhinitis Agents Therapeutic Class Review (TCR) February 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. -

Doxofylline, a Novofylline Inhibits Lung Inflammation Induced By
Pulmonary Pharmacology & Therapeutics 27 (2014) 170e178 Contents lists available at ScienceDirect Pulmonary Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/ypupt Doxofylline, a novofylline inhibits lung inflammation induced by lipopolysacharide in the mouse Yanira Riffo-Vasquez*, Francis Man, Clive P. Page Sackler Institute of Pulmonary Pharmacology, Institute of Pharmaceutical Science, King’s College London, UK article info abstract Article history: Rational: Doxofylline is a xanthine drug that has been used as a treatment for respiratory diseases for Received 20 December 2013 more than 30 years. In addition to doxofylline being a bronchodilator, some studies have indicated that Received in revised form doxofylline also has anti-inflammatory properties, although little is known about the effect of this drug 30 December 2013 on lung inflammation. Accepted 2 January 2014 Objectives: We have investigated the actions of doxofylline against the effects of Escherichia coli LPS in the lungs of BALB/c mice. Keywords: Methods: Animals have been treated with doxofylline (0.1, 0.3 and 1 mg/kg i.p.) 24, -and 1 h before, and Doxofylline m Neutrophils 6 h after intra-nasal instillation of LPS (10 g/mouse). Readouts were performed 24 h later. fi LPS Results: Doxofylline at 1 and 0.3, but not at 0.1 mg/kg, signi cantly inhibit neutrophil recruitment to the Lung lung induced by LPS (LPS: 208.4 Æ 14.5 versus doxofylline: 1 mg/kg: 106.2 Æ 4.8; 0.3 mg/kg: 4 Inflammation 105.3 Æ 10.7 Â 10 cells/ml). Doxofylline significantly inhibited IL-6 and TNF-a release into BAL fluid in Mice comparison to LPS-treated animals (LPS: 1255.6 Æ 143.9 versus doxofylline 1 mg/kg: 527.7 Æ 182.9; 0.3 mg/kg: 823.2 Æ 102.3 pg/ml). -

Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5
ANTICHOLINERGICS: Reference List of Drugs with Potential Anticholinergic Effects 1, 2, 3, 4, 5 J Bareham BSP © www.RxFiles.ca Aug 2021 WHENEVER POSSIBLE, AVOID DRUGS WITH MODERATE TO HIGH ANTICHOLINERGIC ACTIVITY IN OLDER ADULTS (>65 YEARS OF AGE) Low Anticholinergic Activity; Moderate/High Anticholinergic Activity -B in combo Beers Antibiotics Antiparkinsonian Cardiovascular Agents Immunosuppressants ampicillin *ALL AVAILABLE AS amantadine SYMMETREL atenolol TENORMIN azaTHIOprine IMURAN cefOXitin GENERIC benztropine mesylate COGENTIN captopril CAPOTEN cyclosporine NEORAL clindamycin bromocriptine PARLODEL chlorthalidone GENERIC ONLY hydrocortisone CORTEF gentamicin (Oint & Sol’n NIHB covered) carbidopa/levodopa SINEMET digoxin LANOXIN, TOLOXIN methylprednisolone MEDROL piperacillin entacapone COMTAN dilTIAZem CARDIZEM, TIAZAC prednisone WINPRED dipyridamole PERSANTINE, ethopropazine PARSITAN vancomycin phenelzine NARDIL AGGRENOX disopyramide RYTHMODAN Muscle Relaxants pramipexole MIRAPEX Antidepressants baclofen LIORESAL ( on intrathecal only) procyclidine KEMADRIN furosemide LASIX amitriptyline ELAVIL cyclobenzaprine FLEXERIL selegiline ELDEPRYL hydrALAZINE APRESOLINE clomiPRAMINE ANAFRANIL isosorbide ISORDIL methocarbamol ROBAXIN OTC trihexyphenidyl ARTANE desipramine NORPRAMIN metoprolol LOPRESOR orphenadrine NORFLEX OTC doxepin >6mg SINEQUAN Antipsychotics NIFEdipine ADALAT tiZANidine ZANAFLEX A imipramine TOFRANIL quiNIDine GENERIC ONLY C ARIPiprazole ABILIFY & MAINTENA -

Stable Pressurised Aerosol Solution Composition of Glycopyrronium Bromide and Formoterol Combination
(19) TZZ¥¥_T (11) EP 3 384 898 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 10.10.2018 Bulletin 2018/41 A61K 9/00 (2006.01) A61M 15/00 (2006.01) A61K 31/167 (2006.01) A61K 31/40 (2006.01) (2006.01) (2006.01) (21) Application number: 18171127.6 B65D 83/54 A61K 31/573 A61K 31/54 (2006.01) A61K 45/06 (2006.01) (2006.01) (2006.01) (22) Date of filing: 23.12.2014 A61K 9/12 A61K 31/58 A61M 39/22 (2006.01) (84) Designated Contracting States: • COPELLI, Diego AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 43100 PARMA (IT) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • DAGLI ALBERI, Massimiliano PL PT RO RS SE SI SK SM TR 43100 PARMA (IT) Designated Extension States: • USBERTI, Francesca BA ME 43100 PARMA (IT) • ZAMBELLI, Enrico (30) Priority: 30.12.2013 EP 13199784 43100 PARMA (IT) (62) Document number(s) of the earlier application(s) in (74) Representative: Bianchetti Bracco Minoja S.r.l. accordance with Art. 76 EPC: Via Plinio, 63 14825154.9 / 3 089 735 20129 Milano (IT) (71) Applicant: Chiesi Farmaceutici S.p.A. Remarks: 43100 Parma (IT) This application was filed on 08-05-2018 as a divisional application to the application mentioned (72) Inventors: under INID code 62. • BONELLI, Sauro 43100 PARMA (IT) (54) STABLE PRESSURISED AEROSOL SOLUTION COMPOSITION OF GLYCOPYRRONIUM BROMIDE AND FORMOTEROL COMBINATION (57) The invention concerns an aerosol solution lower than the limit of quantification, when stored in ac- composition intended for use with a pressurised metered celerated conditions at 25°C and 60% relative humidity dose inhaler, comprising glycopyrronium bromide and (RH) for 6 months in a can internally coated by a resin formoterol, or a salt thereof or a solvate of said salt, op- comprising a fluorinated ethylene propylene (FEP) poly- tionally in combination with one or more additional active mer. -
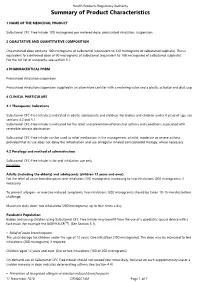
Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE MEDICINAL PRODUCT Salbutamol CFC-Free Inhaler 100 micrograms per metered dose, pressurised inhalation, suspension 2 QUALITATIVE AND QUANTITATIVE COMPOSITION One metered dose contains 100 micrograms of salbutamol (equivalent to 120 micrograms of salbutamol sulphate). This is equivalent to a delivered dose of 90 micrograms of salbutamol (equivalent to 108 micrograms of salbutamol sulphate). For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Pressurised inhalation suspension Pressurised inhalation suspension supplied in an aluminium canister with a metering valve and a plastic actuator and dust cap. 4 CLINICAL PARTICULARS 4.1 Therapeutic Indications Salbutamol CFC-Free Inhaler is indicated in adults, adolescents and children. For babies and children under 4 years of age, see sections 4.2 and 5.1. Salbutamol CFC-Free Inhaler is indicated for the relief and prevention of bronchial asthma and conditions associated with reversible airways obstruction. Salbutamol CFC-Free Inhaler can be used as relief medication in the management of mild, moderate or severe asthma, provided that its use does not delay the introduction and use of regular inhaled corticosteroid therapy, where necessary. 4.2 Posology and method of administration Salbutamol CFC-Free Inhaler is for oral inhalation use only. Posology Adults (including the elderly) and adolescents (children 12 years and over): For the relief of acute bronchospasm, one inhalation (100 micrograms) increasing to two inhalations (200 micrograms), if necessary. To prevent allergen- or exercise-induced symptoms, two inhalations (200 micrograms) should be taken 10-15 minutes before challenge. Maximum daily dose: two inhalations (200 micrograms) up to four times a day. -

2019 Year in Review: Aerosol Therapy
2019 Year in Review: Aerosol Therapy Ariel Berlinski Introduction COPD Newly Approved Drugs Asthma New Devices As-Needed Inhaled Corticosteroid/Long-Acting Bronchodilator Therapy Asthma Medication Report in Adolescents and Caregivers Cystic Fibrosis Hypertonic Saline in Cystic Fibrosis Infectivity of Cough Aerosols in Cystic Fibrosis Liposomal Amikacin for MAC Lung Disease Electronic Nicotine Delivery Systems E-Cigarette or Vaping Associated Lung Injury Secondhand Exposure Summary Relevant publications related to medicinal and toxic aerosols are discussed in this review. Treatment of COPD includes a combination of long-acting bronchodilators and long-acting muscarinic antagonists. A combination of aclidinium bromide and formoterol fumarate was approved in the United States. The combination was superior to its components alone, as well as tiotropium and a salmeterol-fluticasone combination. Increased risk of an asthma exacerba- tion was reported in children exposed to electronic nicotine delivery systems. A smart inhaler capable of recording inspiratory flow was approved in the United States. The use of as-needed budesonide-formoterol was reported to be superior to scheduled budesonide and as-needed ter- butaline for the treatment of adults with mild-to-moderate asthma. A survey among teens with asthma and their caregivers revealed a disagreement in the number of inhaled controller medi- cations the teen was taking. Treatment with inhaled hypertonic saline resulted in a decreased lung clearance index in infants and preschool children with cystic fibrosis. Surgical masks were well tolerated and significantly decreased the burden of aerosolized bacteria generated by coughing in adults with cystic fibrosis. Inhaled liposomal amikacin in addition to guideline- based therapy was reported to be superior to guideline-based therapy alone in achieving nega- tive sputum cultures in adult subjects with Mycobacterium avium complex pulmonary disease. -

Hypersalivation in Children and Adults
Pharmacological Management of Hypersalivation in Children and Adults Scope: Adult patients with Parkinson’s disease, children with neurodisability, cerebral palsy, long-term ventilation with drooling, and drug-induced hypersalivation. ASSESSMENT OF SEVERITY/RESPONSE TO TREATMENT: Severity of drooling can be assessed subjectively via discussion with patients and their carers/parents and by observation. Amount of drooling can be quantified by measuring the number of bibs required per day and this can also be graded using the Thomas-Stonell and Greenberg scale: • 1 = Dry (no drooling) • 2 = Mild (moist lips) • 3 = Moderate (wet lips and chin) • 4 = Severe (damp clothing) CONSIDERATIONS FOR PRESCRIBING/TITRATION No evidence to support the use of one particular treatment over another. Drug choice is to be determined by individual patient factors. When prescribing/titrating antimuscarinic drugs to treat hypersalivation always take account of: • Coexisting conditions (for example, history of urinary retention, constipation, glaucoma, dental issues, reflux etc.) • Use of other existing medication affecting the total antimuscarinic burden • Risk of adverse effects Titrate dose upward until the desired level of dryness, side effects or maximum dose reached. Take into account the preferences of the patients and their carers/ parents, and the age range and indication covered by the marketing authorisations (see individual summaries of product characteristics, BNF or BNFc for full prescribing information). FIRST LINE DRUG TREATMENT OPTIONS FOR ADULTS