(CHASP): Findings from Literature Review and Baseline Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Grouped by Cluster
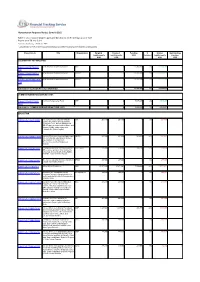
Humanitarian Response Plan(s): Somalia 2015 Table E: List of appeal projects (grouped by Cluster), with funding status of each Report as of 28-Sep-2021 http://fts.unocha.org (Table ref: R##) Compiled by OCHA on the basis of information provided by donors and recipient organizations. Project Code Title Organization Original Revised Funding % Unmet Outstanding requirements requirements USD Covered requirements pledges USD USD USD USD CLUSTER NOT YET SPECIFIED SOM-15/SNYS/78452/ to be allocated to specific projects WFP 0 0 15,200,048 0% -15,200,048 0 561 SOM-15/SNYS/78471/ to be allocated to specific projects UNHCR 0 0 22,776,204 0% -22,776,204 0 120 SOM-15/SNYS/78658/R/ to be allocated to specific projects UNICEF 0 0 13,712,399 0% -13,712,399 0 124 Sub total for CLUSTER NOT YET SPECIFIED 0 0 51,688,651 0% -51,688,651 0 COMMON HUMANITARIAN FUND (CHF) SOM-15/SNYS/77965/ Common Humanitarian Fund CHF 0 0 9,595,257 0% -9,595,257 0 7622 Sub total for COMMON HUMANITARIAN FUND (CHF) 0 0 9,595,257 0% -9,595,257 0 EDUCATION SOM-15/E/71574/8380 Increasing Access & Quality of Basic JCC 201,150 201,150 0 0% 201,150 0 Literacy for Children and Adults from Vulnerable, Poor, Women Headed and IDP / Returness Households in Bu'ale and Salagle (Middle Jubba region) and Celbarde-Ato (Bakool region) SOM-15/E/71608/14579 Improved Protective Learning Spaces and FENPS 451,400 451,400 289,999 64% 161,401 0 Access to Quality Education for School Age Children in Humanitarian Emergencies and Conflict Areas in Somalia SOM-15/E/71628/5660 Emergency education for crises-affected -

Highlights Map 1: January 2012 Monthly Rain Gauge Data (Mm) Map 2: January 2012 Monthly Rainfall Estimates
Food Security and Nutrition Analysis Unit - Somalia Monthly Rainfall and NDVI, January, 2012 Highlights Map 1: January 2012 Monthly Rain Gauge data (mm) Map 2: January 2012 Monthly Rainfall Estimates Sunny and dry weather conditions, DJIBOUTI Gulf of Aden AWDAL characterized by higher than BARI SANAG average daytime temperatures W. GALBEED and strong winds manifested the TOGDHEER SOOL presence of the Jilaal dry season. NUGAL Observed rainfall data from ETHIOPIA SWALIM monitored weather ETHIOPIA stations have recorded zero MUDUG Indian Ocean rainfall in all the stations during GALGADUD the month of January. BAKOOL HIRAN Millimeters Satellite derived Rainfall Estimates GEDO (RFE) confirmed the prevailing M.SHABELLE dry weather conditions in most BAY of the country in January (Map L.SHABELLE M. JUBA 2-5). FSNAU field reports indicate 40 hotter and drier than normal L.JUBA conditions in most parts of the country as expected during the season. The exception is the Source: SWALIM Source: NOAA Golis-Guban livelihood zone, which received small amounts of January 2012: Dekadal Rainfall Estimates (RFE) localized Hays rains. Map 3: 1st Dekad (1-10) Map 4: 2nd Dekad (11-20) Map 5: 3rd Dekad (21-30) DJIBOUTI Gulf of Aden DJIBOUTI Gulf of Aden DJIBOUTI Gulf of Aden Bari The Normalized Difference Awdal Awdal Sanag Bari Awdal Sanag Sanag Bari W. Galbeed W. Galbeed Vegetation Index (NDVI) W. Galbeed Nugal Togdheer indicates generally above average Togdheer Sool Togdheer Sool Sool Nugal Nugal Mudug vegetation in the South, with no ETHIOPIA ETHIOPIA ETHIOPIA change from the previous month Mudug Mudug Galgadud Galgadud Galgadud Indian in most areas of the country (Map Ocean Indian Indian Bakool Hiran Bakool Hiran Bakool Hiran 10). -

Assessment Report 2011
ASSESSMENT REPORT 2011 PHASE 1 - PEACE AND RECONCILIATION JOIN- TOGETHER ACTION For Galmudug, Himan and Heb, Galgaduud and Hiiraan Regions, Somalia Yme/NorSom/GSA By OMAR SALAD BSc (HONS.) DIPSOCPOL, DIPGOV&POL Consultant, in collaboration with HØLJE HAUGSJÅ (program Manager Yme) and MOHAMED ELMI SABRIE JAMALLE (Director NorSom). 1 Table of Contents Pages Summary of Findings, Analysis and Assessment 5-11 1. Introduction 5 2. Common Geography and History Background of the Central Regions 5 3. Political, Administrative Governing Structures and Roles of Central Regions 6 4. Urban Society and Clan Dynamics 6 5. Impact of Piracy on the Economic, Social and Security Issues 6 6. Identification of Possibility of Peace Seeking Stakeholders in Central Regions 7 7. Identification of Stakeholders and Best Practices of Peace-building 9 8. How Conflicts resolved and peace Built between People Living Together According 9 to Stakeholders 9. What Causes Conflicts Both locally and regional/Central? 9 10. Best Practices of Ensuring Women participation in the process 9 11. Best Practices of organising a Peace Conference 10 12. Relations Between Central Regions and Between them TFG 10 13. Table 1: Organisation, Ownership and Legal Structure of the 10 14. Peace Conference 10 15. Conclusion 11 16. Recap 11 16.1 Main Background Points 16.2 Recommendations 16.3 Expected Outcomes of a Peace Conference Main and Detailed Report Page 1. Common geography and History Background of Central Regions 13 1.1 Overview geographical and Environmental Situation 13 1.2 Common History and interdependence 14 1.3 Chronic Neglect of Central Regions 15 1.4 Correlation Between neglect and conflict 15 2. -
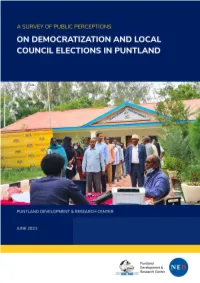
Survey of Public Perceptions on Local Elections in Puntland
A SURVEY OF PUBLIC PERCEPTIONS ON DEMOCRATIZATION AND LOCAL COUNCIL ELECTIONS IN PUNTLAND JULY 2021 Puntland Development & Research Center www.pdrcsomalia.org Copyright © 2021 Puntland Development & Research Center. All rights reserved. ACKNOWLEDGEMENT Puntland Development Research Center (PDRC) would like to thank the Ministry of Interior, Federal Affairs and Democratization for their collaboration during this survey. In addition, I would like to extend my sincere gratitude and appreciation to Nugal University, Somali National University (Badhan), and East Africa University for their role in identifying a team of students who ably supported the data collection for this survey. Critical to the success of this survey include the National Endowment for Democracy (NED) who provided technical and financial support to the survey. Finally, I would like to express my utmost gratitude to PDRC research team (Abdinasir Mohamed Yusuf, Muctar Hirsi Mohamed, and Fardows Ahmed Gambol) for their tireless efforts in bringing the survey work to completion. Ali Farah Ali Executive Director Puntland Development Research Center Garowe, Puntland State of Somalia ii TABLE OF CONTENTS Executive Summary .......................................................................................................................................... 1 1. Background and Objectives .................................................................................................................. 4 1.1 Methodology .......................................................................................................................................... -

Somali Fisheries
www.securefisheries.org SECURING SOMALI FISHERIES Sarah M. Glaser Paige M. Roberts Robert H. Mazurek Kaija J. Hurlburt Liza Kane-Hartnett Securing Somali Fisheries | i SECURING SOMALI FISHERIES Sarah M. Glaser Paige M. Roberts Robert H. Mazurek Kaija J. Hurlburt Liza Kane-Hartnett Contributors: Ashley Wilson, Timothy Davies, and Robert Arthur (MRAG, London) Graphics: Timothy Schommer and Andrea Jovanovic Please send comments and questions to: Sarah M. Glaser, PhD Research Associate, Secure Fisheries One Earth Future Foundation +1 720 214 4425 [email protected] Please cite this document as: Glaser SM, Roberts PM, Mazurek RH, Hurlburt KJ, and Kane-Hartnett L (2015) Securing Somali Fisheries. Denver, CO: One Earth Future Foundation. DOI: 10.18289/OEF.2015.001 Secure Fisheries is a program of the One Earth Future Foundation Cover Photo: Shakila Sadik Hashim at Alla Aamin fishing company in Berbera, Jean-Pierre Larroque. ii | Securing Somali Fisheries TABLE OF CONTENTS LIST OF FIGURES, TABLES, BOXES ............................................................................................. iii FOUNDER’S LETTER .................................................................................................................... v ACKNOWLEDGEMENTS ............................................................................................................. vi DEDICATION ............................................................................................................................ vii EXECUTIVE SUMMARY (Somali) ............................................................................................ -

Highlights Map 1: November 2015 Monthly Rain Gauge Data Map 2: November 2015 TAMSAT Monthly Rainfall Estimates
Food Security and Nutrition Analysis Unit - Somalia November 2015 Monthly Rainfall and NDVI (Issued December 15, 2015) Highlights Map 1: November 2015 Monthly Rain Gauge Data Map 2: November 2015 TAMSAT Monthly Rainfall Estimates Gulf of Aden The month of November 2015 has Gulf of Aden DJIBOUTI AWDAL been marked by heavy rains in most BARI SANAG parts of the country with many stations W. GALBEED recording above average rains. The TOGDHEER southern regions were the wettest SOOL during the month with various stations NUGAL recording above average rains in most ETHIOPIA ETHIOPIA of te regions. Some of the stations that MUDUG recorded significant rainfall in the North Indian Ocean Indian Ocean include: Eyl (226mm), Alula (194mm), GALGADUD Elafweyn (138mm) while in the South Hudur, Elbarde, Dinsor, Beletweyn, HIRAN Balad and Jamame stations recorded BAKOOL 226mm, 119mm, 176mm, 130mm, GEDO M.SHABELLE 104mm and 120mm respectively (Table BAY 1 and Map 1). In the second dekad of November 2015, tropical cyclone L.SHABELLE (Chapala) hit Tooxin and Bareedo M. JUBA villages of Alula district in Bari region L.JUBA causing damage of houses and loss of boats to some fishermen. Source: TAMSAT and JRC Satellite-derived (TAMSAT) Rainfall Source: SWALIM Estimates (RFE) confirms the continuation of Deyr rains through late November. November 2015: TAMSAT Dekadal RFE The satellite imegery indicate enhanced rains in the Jubas, Shabelles, Bay and Map 3: 1st Dekad (1-10) Map 4: 2nd Dekad (11-20) Map 5: 3rd Dekad (21-30) parts of Hiran (Maps 2-5 and 9). The DJIBOUTI Gulf of Aden DJIBOUTI Gulf of Aden DJIBOUTI Gulf of Aden Bari Awdal Normalized Difference Vegetation Index Sanag Bari Awdal Sanag Awdal Sanag Bari W. -

Emergency Appeal Operations Update Somalia: Tropical Cyclone
Emergency appeal operations update Somalia: Tropical cyclone Emergency appeal n° MDRSO002 GLIDE n° TC – 2013-000140-SOM Operations update n° 2 Timeframe covered by this update: 10 January 2014 – 5 February 2014 Emergency Appeal operation start date: 20 Timeframe: 9 months and end date September 2014 December 2013 Appeal budget: CHF Appeal coverage: Total estimated Red Cross and Red Crescent 2,406,038 18 % response to date: CHF 426,817 Disaster Relief Emergency Fund (DREF) allocated: 67,841 N° of people being assisted: 23,100 (3,300 households) Host National Society presence (n° of volunteers, staff, branches): 50 volunteers, 40 staff and 2 SRCS Branches (Garowe and Bosaso) Red Cross Red Crescent Movement partners actively involved in the operation: Somali Red Crescent Society (SRCS), IFRC, ICRC Other partner organizations actively involved in the operation: WFP,UNICEF,UNHCR,FAO,UNFPA, World Vision, CARE, NRC, DRC, IOM, FINAID, ADESO Summary: On Sunday 10 November 2013, the State of Puntland was hit by a tropical cyclone, followed by very heavy rains and flash floods. The cyclone caused loss of human lives and the destruction of assets including livestock and fishing boats, destroyed numerous settlements, service centers, roads, schools, communication and electrical installations. The most affected areas included, Dangorayo, Bandar Beyla, Garowe and Eyl districts. Other areas affected include the coastal villages in Bari region including Hafun, Iskushuban, Bargal, Qandala and Allula districts. With the support of IFRC and the start-up loan provided through the DREF operation, the Somali Red Crescent Society (SRCS) undertook a detailed assessment in the affected areas in Nugaal and Bari regions. -

SOMALIA Food Security Outlook October 2018 to May 2019
SOMALIA Food Security Outlook October 2018 to May 2019 Deyr rainfall expected to sustain current outcomes, except in some pastoral areas KEY MESSAGES Current food security outcomes, October 2018 • Food security has continued to improve throughout Somalia since the 2018 Gu. Most northern and central livelihood zones are Stressed (IPC Phase 2), while southern livelihood zones are Minimal (IPC Phase 1) or Stressed (IPC Phase 2). In October, humanitarian assistance continued to prevent worse outcomes in Guban Pastoral and northwestern Northern Inland Pastoral (NIP) livelihood zones, where Crisis! (IPC Phase 3!) and Stressed! (IPC Phase 2!) outcomes persist, respectively. Northwest Agropastoral and most IDP settlements are also in Crisis (IPC Phase 3). • Contrary to earlier forecasts, Deyr seasonal rainfall is now expected to be below-average despite the development of a weak El Niño. Overall, favorable soil moisture is anticipated to prevent large declines in Deyr crop production and rangeland resources, and current outcomes are likely to be sustained in most livelihood zones through May 2019. In Addun Pastoral, Coastal Deeh Pastoral and Fishing, and northeastern NIP livelihood zones, however, deterioration in pasture and water resources is likely to lead to Crisis (IPC Phase 3) outcomes during Source: FEWS NET and FSNAU FEWS NET and FSNAU classification is IPC-compatible. IPC- the 2019 pastoral lean season. compatible analysis follows key IPC protocols but does not necessarily reflect a consensus of national food security partners. • In the absence of food assistance, deterioration to Emergency (IPC Phase 4) in Guban Pastoral livelihood zone and to Crisis (IPC Phase 3) in northwestern NIP livelihood zone is likely. -
Peace in Puntland: Mapping the Progress Democratization, Decentralization, and Security and Rule of Law
Peace in Puntland: Mapping the Progress Democratization, Decentralization, and Security and Rule of Law Pillars of Peace Somali Programme Garowe, November 2015 Acknowledgment This Report was prepared by the Puntland Development Re- search Center (PDRC) and the Interpeace Regional Office for Eastern and Central Africa. Lead Researchers Research Coordinator: Ali Farah Ali Security and Rule of Law Pillar: Ahmed Osman Adan Democratization Pillar: Mohamoud Ali Said, Hassan Aden Mo- hamed Decentralization Pillar: Amina Mohamed Abdulkadir Audio and Video Unit: Muctar Mohamed Hersi Research Advisor Abdirahman Osman Raghe Editorial Support Peter W. Mackenzie, Peter Nordstrom, Jessamy Garver- Affeldt, Jesse Kariuki and Claire Elder Design and Layout David Müller Printer Kul Graphics Ltd Front cover photo: Swearing-in of Galkayo Local Council. Back cover photo: Mother of slain victim reaffirms her com- mittment to peace and rejection of revenge killings at MAVU film forum in Herojalle. ISBN: 978-9966-1665-7-9 Copyright: Puntland Development Research Center (PDRC) Published: November 2015 This report was produced by the Puntland Development Re- search Center (PDRC) with the support of Interpeace and represents exclusively their own views. These views have not been adopted or in any way approved by the contribut- ing donors and should not be relied upon as a statement of the contributing donors or their services. The contributing donors do not guarantee the accuracy of the data included in this report, nor do they accept responsibility for any use -

6.5.HOA Outbreak Response Assessment 8-12 June 15 – Somalia
4th HOA Outbreak Response Assessment Somalia 8th to 12th June 2015 “Carve your name on hearts, not tombstones. A legacy is etched into the minds of others and the stories they share about you.” - Alder In fond memory of Brenda & Payenda Objectives • Determine as accurately as possible whether or not polio transmission has been stopped • Determine the level of support the country requires in order to achieve or maintain levels of surveillance sensitivity and population immunity sufficient enough to reliably maintain a polio-free status • Provide recommendations for strengthening AFP surveillance and to ensure that a comprehensive and adequate outbreak preparedness plan is in place. Methodology • Overview presentations on country and zones by WHO and UNICEF • Small group discussions with zonal teams of Government, UNICEF, and WHO • Document review and analysis – no field assessment due to security reasons • Provide feedback to the Government authorities and partner teams Subject areas of assessment • Implementation of recommendation from previous assessment • Quality of outbreak response • AFP surveillance sensitivity – Risk of undetected transmission – Ability to detect any new transmission at earliest • Population Immunity: Quality of SIAs, RI and assessment of need for additional SIAs • Communication strategy • Plans to strengthen / maintain population immunity with special focus on known high risk areas and populations • Outbreak preparedness and response plan Subject areas of assessment • Implementation of recommendation from previous -

Enhanced Enrolment of Pastoralists in the Implementation and Evaluation of the UNICEF-FAO-WFP Resilience Strategy in Somalia
Enhanced enrolment of pastoralists in the implementation and evaluation of the UNICEF-FAO-WFP Resilience Strategy in Somalia Prepared for UNICEF Eastern and Southern Africa Regional Office (ESARO) by Esther Schelling, Swiss Tropical and Public Health Institute UNICEF ESARO JUNE 2013 Enhanced enrolment of pastoralists in the implementation and evaluation of UNICEF-FAO-WFP Resilience Strategy in Somalia © United Nations Children's Fund (UNICEF), Nairobi, 2013 UNICEF Eastern and Southern Africa Regional Office (ESARO) PO Box 44145-00100 GPO Nairobi June 2013 The report was prepared for UNICEF Eastern and Southern Africa Regional Office (ESARO) by Esther Schelling, Swiss Tropical and Public Health Institute. The contents of this report do not necessarily reflect the policies or the views of UNICEF. The text has not been edited to official publication standards and UNICEF accepts no responsibility for errors. The designations in this publication do not imply an opinion on legal status of any country or territory, or of its authorities, or the delimitation of frontiers. For further information, please contact: Esther Schelling, Swiss Tropical and Public Health Institute, University of Basel: [email protected] Eugenie Reidy, UNICEF ESARO: [email protected] Dorothee Klaus, UNICEF ESARO: [email protected] Cover photograph © UNICEF/NYHQ2009-2301/Kate Holt 2 Table of Contents Foreword ........................................................................................................................................................................... -

Remittances and Livelihoods Support in Puntland and Somaliland Issued June 5, 2013 Acknowledgement
Family Ties: Executive Summary Remittances I and Livelihoods Support in Puntland and Somaliland June 5, 2013 Food Security and Nutrition Analysis Unit - Somalia Information for Better Livelihood Funding Agencies Family Ties: Remittances and Livelihoods Support in Puntland and Somaliland Swiss Agency for Development Issued June 5, 2013 and Cooperation SDC II DISCLAIMER This study was commissioned by the Food Security and Nutrition Analysis Unit (FSNAU) for Somalia, a project managed by the Food and Agriculture Organization of the United Nations (FAO). It was made possible through financial support from a number of donors listed whose logos appear on the front cover of this study report. The contents of this report are the sole responsibility of the authors and do not necessarily reflect the views and policies of FSNAU/FAO. Geographic names and administrative divisions, and presentation of material in the maps, used for the purpose of statistical analysis in this report, do not imply endorsement by the United Nations or any other agencies involved in the production of the report. Specifically, the designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of FAO concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Family Ties: Remittances and Livelihoods Support in Puntland and Somaliland Issued June 5, 2013 Acknowledgement III ACKNOWLEDGEMENT This study on remittances was commissioned by the Food Security and Nutrition Analysis Unit for Somalia (FSNAU), a project managed by the United Nations Food and Agriculture Organization (FAO).