History of EMS and Trauma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arizona Guidelines for Field Triage of Injured Patients (Regional Modifications Are Permissible)
Arizona Guidelines for Field Triage of Injured Patients (Regional modifications are permissible) FIELD TRIAGE DECISION SCHEME Measure vital signs and level of consciousness Glasgow Coma Scale ≤13 Systolic blood pressure (mmHg) <90 mmHg Step One Respiratory rate <10 or >29 breaths per minute (<20 in infant aged < 1 year1), or need for ventilator support YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess anatomy of injury. patients. These patients should be transported preferentially to the highest level of care within the trauma system. • All penetrating injuries to head, neck, torso, and extremities proximal to elbow or knee • Chest wall instability or deformity (e.g., flail chest) • Two or more proximal long-bone fractures • Crushed, de-gloved, mangled, or pulseless extremity Step Two3 • Amputation proximal to wrist or ankle • Pelvic fractures • Open or depressed skull fracture • Paralysis YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess mechanism of injury patients. These patients should be transported preferentially to the highest level of care within the and evidence of high-energy trauma system. impact. • Falls o Adults: >20 feet (one story is equal to 10 feet) 4 o Children : >10 feet or two or three times the height of the child • High-risk auto crash 5 Intrusion , including roof: >12 inches occupant site; >18 inches any site Step Three3 o o Ejection (partial or complete) from automobile o Death in same passenger compartment o Vehicle telemetry data consistent with high risk of injury 6 • Auto vs. -
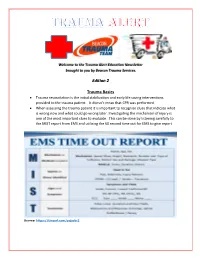
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -
Needs Assessment for New Trauma Center Development in the Commonwealth of Pennsylvania 2014
WHITE PAPER ON NEEDS ASSESSMENT FOR NEW TRAUMA CENTER DEVELOPMENT IN THE COMMONWEALTH OF PENNSYLVANIA 2014 Purpose Currently new trauma center development in Pennsylvania—with limited exception—is driven by competitive financial and hospital/healthcare system imperatives. The Pennsylvania Trauma Systems Foundation strongly recommends that going forward, new trauma center applications be based on a needs assessment process so as to optimize distribution of trauma centers in the trauma system and thereby provide optimal trauma care for the citizens of the Commonwealth of Pennsylvania. A guide for such a needs assessment is provided in this paper. Introduction Trauma systems have developed based on the sole precept that optimal recovery from traumatic injury is best achieved through the organization of prehospital and hospital preparedness and capability into a codified continuum of care. A codified continuum of care that is designated/accredited on a regular basis by qualified organizations such as the Pennsylvania Trauma Systems Foundation (PTSF). It is undisputed that trauma centers in states such as Pennsylvania have significantly improved the public health for citizens of the Commonwealth. Trauma is the fifth leading cause of death in Pennsylvania. A Pa. Department of Health study demonstrated a 30% reduced chance of death for severely injured patients treated in an accredited trauma center. In 2012, 95.6% of the 40,479 trauma qualifying patients treated at a trauma center survived. Currently, there are a total of 32 trauma centers in PA as noted below. 1 Figure 1 Source: http://www.rural.palegislature.us/demographics_rural_urban_counties.html As is readily appreciated, the majority of trauma centers are in the most populated counties (Philadelphia and Allegheny) with large areas of the state seemingly having little or no ready access to organized trauma care. -

The Trauma Center Providing Lifesaving Care for Critically Injured Patients
A community newsletter from Antelope Valley Hospital July/August 2017 The Trauma Center Providing Lifesaving Care for Critically Injured Patients Rapid Response Mental Health Services Team Ready to Expansion on Horizon Provide Early Intervention 24/7 In this issue Growing Excellence 2 CEO Message 3 Mental Health Services Right in Your Expansion on Horizon Own Backyard 4 Rapid Response Team Ready to Provide Early Intervention 24/7 5 Hyperbaric Oxygen erapy he previous issue of HealthConnect featured an article describing the Aids in Wound Healing upcoming reopening of our outpatient surgery center through a part - nership between AV Hospital and a local surgery center. In this issue AVH Trauma Center Provides T 6 we’re announcing the expansion of our mental health services. Combined, Lifesaving Care for Critically these two initiatives signify a renewal as well as a change for both our hospital Injured Patients and the overall healthcare in our community. 9 Amazing Person e renewal, of course, is our continued commitment to ensuring that local From Tragedy Comes Sense families don’t need to travel outside the Antelope Valley to receive exceptional of Community for AVH care. at has never been truer than it is today. AV Hospital is a state-of-the-art Employee and Family medical center offering services, technologies and staffing far beyond what would normally be found in a traditional local community hospital. is includes our Hospital Highlights 10 incredible trauma center, which is also featured in this issue. What’s more is Annual Summer Blood Drive that our 450-member medical staff includes primary care physicians, internists 12 and specialists who have been trained at some of the best medical schools and programs in the world. -

Read Onlinepdf 18.98 MB
ResidentOfficial Publication of the Emergency Medicine Residents’ Association December 2018/January 2019 VOL 45 / ISSUE 6 Exertional Rhabdomyolysis EmBassador Travel Team Seeking the Best and Brightest EM Physicians Enjoy the flexibility to live where you want and practice where you are needed. EmBassador TRAVEL TEAM PHYSICIANS RECEIVE: Paid travel and Practice variety accommodations Concierge support Travel convenience package Regional engagements, Paid medical staff dues, equitable scheduling and licenses, certifications and no mandatory long-term applications employment commitment Exceptional Fast track to future compensation package leadership opportunities For More Information: Mansoor Khan, MD National Director, EmBassador Program 917.656.6958 | [email protected] ENVISION PHYSICIAN SERVICES OFFERS ... programs that align physicians to become leaders MANSOOR KHAN, MD, MHA, FAAEM EMERGENCY MEDICINE Why EM Residents choose Envision Physician Services ■ Professional Development and Career Advancement ■ Employment Flexibility: Full-Time, Part-Time, moonlighting and travel team. Employed and Independent Contractor options ■ Practice Variety: Coast-to-coast opportunities at well-recognized hospitals and health systems ■ Unparalleled practice support ■ Earn While You Learn Program: Provides senior residents with $2,500/month while you complete your residency For more information, contact: 877.226.6059 [email protected] TABLE OF CONTENTS EDITORIAL STAFF Categories EDITOR-IN-CHIEF Tommy Eales, DO Indiana University COVER STORY DEPUTY -

Anytown Trauma Center Trauma Protocols
ANYTOWN TRAUMA CENTER TRAUMA PROTOCOLS TITLE: TRAUMA TEAM ACTIVATION PROTOCOL PURPOSE: The purpose of the protocol is to establish guidelines for trauma team activation and define the members of the responding trauma team to facilitate the resuscitation and management of critical or seriously injured patients who require rapid, organized resuscitation, evaluation and stabilization to promote optimal outcomes. It also serves to provide triage guidelines for adult and pediatric patients. PROCESS: 1. TRAUMA TEAM ACTIVATION PROTCOL A. The criteria for activation of the trauma team is clearly defined and posted at the Emergency Department triage desk, by the EMS communication station and in the resuscitation rooms. B. The trauma team may be activated prior to arrival based on the EMS communication and their assessment. C. The trauma surgeon, emergency medicine physician, emergency department charge nurse/ house supervisor, emergency department nurses and the Trauma Program Manager may activate the trauma team. D. The person calling the trauma activation will initiate the trauma page to group page the trauma team and will specify the MOI, BP, HR, ETA and level of activation required and age if available. E. If the trauma team members are present in the emergency department and alert is still communicated to ensure everyone is notified. F. Trauma team member notification and arrival times will be documented on the trauma flow sheet (paper or electronic). G. Trauma team members will sign-in when they arrive. H. Trauma team members will be activated for all patients who meet the following criteria: 1. Level 1 trauma activation (major): life threatening injuries and/or unstable vital signs, limb-threating or disability threatening injury 2. -

Committee on Trauma: History and Future Direction
Committee on Trauma: History and Future Direction Ronald M. Stewart, MD October 12, 2015 National Association of State EMS Officials The Problem • 180,000 lives lost each year • 1 million disabled • 10 million lives worldwide • One of the two most expensive health care problems in the US • Leading cause of death world wide 2020 35% reduction 6,720 lives United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS), Office of Analysis, Epidemiology, and Health Promotion (OAEHP), Compressed Mortality File (CMF) compiled from CMF 1968-1988, Series 20, No. 2A 2000, CMF 1989-1998, Series 20, No. 2E 2003 and CMF 1999-2001, Series 20, No. 2G 2004 on CDC WONDER On-line Database. !"##$%&'()*+',#-.%/-)0)1)*2' •! 3"45&4'-2-*#&'$#6#1%.&#/*')-'-%&#(+4*' 5/)75#')/'*+#'8%/*#&.%"4"2'9:' •! ;6)$#/8#$'04-#$'-#1<=>%6#"/4/8#' –!!"##$%&'4/$',#-.%/-)0)1)*2' –!?%$#1'<%"')&."%6)/>'%"'-%16)/>'&%-*'%<'%5"' &4@%"'."%01#&-' "Freedom, however, is not the last word. Freedom is only part of the story and half of the truth!In fact, freedom is in danger of deteriorating!unless it is lived in terms of responsibleness.” Viktor Frankl, MD A6#"6)#(' •! BC:'?%$#1'<%"'D#41*+'C4"#'E&."%6#&#/*' •! 3+#'B&#")84/'C%11#>#'%<':5">#%/-'C%&&)F##' %/'3"45&4' –! G+%' –! G+4*'' –! G+#/' –! G+#"#' –! G+2' –! D%(' •! !5*5"#':*"4*#>)8'H)"#8I%/'4/$'J#('K"%>"4&-' The ACS Model for Health Care Quality • Set appropriate standards • Insure the right infrastructure • Use the right data • Verify Pioneered and Developed by COT “One may long, as I do, for a gentler flame, a respite, a pause for musing. -

A Historical Perspective of the Level II Trauma Center at Lancaster
A HISTORICAL PERSPECTIVE OF THE LEVEL II TRAUMA CENTER AT LANCASTER GENERAL HOSPITAL Frederick B. Rogers, MD, MS, FACS Frederick Beyer, MD, FACS Brian Gross, BS INTRODUCTION The Level II trauma center at Lancaster General Hospital (LGH) was one of the first to be verified by the newly established state trauma foundation (Pennsylvania Trauma Systems Foundation- PTSF) in 1987. For nearly 30 years, the trauma center at LGH has been caring for the seriously- injured patients of Lancaster County and its environs, admitting over 2,000 critically injured patients per year—a volume that rivals many Level I programs. While we now consider our Level II trauma center to be a mainstay of the LGH healthcare system, few people are aware of the extraordinary time, fortitude, and perseverance that went into its birth and development. Through the years, there were times of incredible pride, times of despondency and reflection, and even times of humor. Throughout all these times, however, there was never any question of our commitment to having a Level II trauma center that would serve the needs of the community. The purpose of this review is to examine the history of our trauma center, while acknowledging some of its important figures and their individual contributions. As many of these individuals still work at LGH in different capacities, it is the purpose of this review to recognize the time and resources they brought to the success of the trauma program and are continuing to bring to this organization. We also wish to acknowledge other significant contributors who deserve recognition but are not individually mentioned. -

Trauma Center Transfer of Elderly Patients with Mild Traumatic Brain Injury Improves Outcomes
The American Journal of Surgery xxx (xxxx) xxx Contents lists available at ScienceDirect The American Journal of Surgery journal homepage: www.americanjournalofsurgery.com Trauma center transfer of elderly patients with mild Traumatic Brain Injury improves outcomes * Ana M. Velez a, , Spiros G. Frangos b, Charles J. DiMaggio b, c, Cherisse D. Berry b, Jacob B. Avraham a, Marko Bukur b a New York University School of Medicine, Department of Surgery, 462 First Avenue, NBV 15 N1, 10016, New York, NY, USA b New York University School of Medicine, Department of Surgery, Division of Trauma and Acute Care Surgery, 462 First Avenue, NBV 15 N1, 10016, New York, NY, USA c New York University School of Medicine, Department of Population Health, New York, NY, USA article info abstract Article history: Background: Elderly patients with Traumatic Brain Injury (TBI) are frequently transferred to designated Received 29 October 2018 Trauma Centers (TC). We hypothesized that TC transfer is associated with improved outcomes. Received in revised form Methods: Retrospective study utilizing the National Trauma Databank. Demographics, injury and out- 4 June 2019 comes data were abstracted. Patients were dichotomized by transfer to a designated level I/II TC vs. not. Accepted 10 June 2019 Multivariate regression was used to derive the adjusted primary outcome, mortality, and secondary outcomes, complications and discharge disposition. Keywords: Results: 19,664 patients were included, with a mean age of 78.1 years. 70% were transferred to a level I/II Elderly < fi Mortality TC. Transferred patients had a higher ISS (12 vs. 10, p 0.001). Mortality was signi cantly lower in pa- ¼ Outcomes tients transferred to level I/II TCs (5.6% vs. -

The NIH Clinical Center MICU (6 Months) Washington Hospital
NIH Clinical Center Critical Care Medicine Department Sample Clinical Training Rotation The NIH Clinical Center MICU (6 months) The Clinical Center of the National Institutes of Health is the world's largest hospital facility devoted exclusively to patient oriented biomedical research. The CCMD has sole responsibility for the medical/pediatric/coronary intensive care unit, which provides critical care for all patients with general medical and cardiac problems, as well as manages all critically ill pediatric patients and some subspecialty surgery patients. The medical intensive care unit has full responsibility for the patients, and CCMD fellows write all of the orders. The fellow serves a consultative role in the general surgery/neurosurgery and marrow transplant units and frequently is called upon to assume the primary management of complicated preoperative and postoperative patients. Multidisciplinary teaching rounds are held twice daily. First-year critical care fellows spend six months at the Clinical Center. They are charged with responsibility for all aspects of patient care, under the supervision of CCMD senior staff physicians. Critical care fellows also receive experience in respiratory therapy and anesthesiology. Clinical Center respiratory therapy and cardiopulmonary monitoring services are provided by the CCMD. First-year critical care fellows are required to spend time in the Clinical Center operating rooms to master airway management skills. Washington Hospital Center SICU (2 months) Director, Surgical Critical Care Services: Arthur St. Andre, M.D. The Washington Hospital Center is the largest trauma center in the DC Metropolitan area and also one of the highest volume cardiac surgery centers in the area. At Washington Hospital Center Surgical Critical Care Services, the CCMD fellow, aided by a team of interns and residents, has principal responsibility for supervising one of the three 12-bed surgical intensive care units, under the guidance of an attending physician. -

Nursing Unit Descriptions – Uchealth Northern Colorado
Nursing Unit Descriptions – UCHealth northern Colorado CARDIOVASCULAR SERVICE LINE Cardiac Unit (PVH & MCR) The cardiac units at PVH and MCR have a total of 39 beds. Patients admitted to these units have diagnoses such as acute myocardial infarction (AMI), chronic heart failure (CHF), coronary artery disease (CAD), and post percutaneous coronary intervention (PCI). MCR cardiac unit also has patients who are post-cardiac or vascular surgery or cardiothoracic surgery. PVH cardiac also cares for patients needing non-invasive ventilation. Both units utilize a team concept that consists of many disciplines working together for each and every patient. CRITICAL CARE SERVICES Surgical Intensive Care Unit / SICU (MCR) – This is a 12-bed unit specializing in acutely ill adults with medical, surgical, neurological and neurosurgical illnesses and patients who have sustained traumatic injuries. Surgical Progressive Care Unit (MCR) – This is a 12-bed unit specializing in intermediate or moderately stable care of the acutely ill adult patient with medical, surgical, neurological, and neurosurgical illnesses and patients who have sustained traumatic injuries. Cardiac Intensive Care Unit / CICU (MCR) – This is a 12-bed unit specializing in acutely ill adults with medical and cardiovascular illnesses and patients who have undergone interventional radiology, vascular and cardiothoracic surgeries. Cardiac Progressive Care Unit (MCR) – This is a 12-bed unit that specializes in the intermediate or moderately stable care of the adult cardiac/telemetry patient population such as heart failure, cardiomyopathy, R/O myocardial infarction (MI), and 24-hour post open hearts. Intensive Care Unit / ICU (PVH) – This is a 12-bed unit specializing in acutely ill adults with medical and surgical conditions. -

Trauma Center Designation
Trauma Center Designation The District of Columbia is fortunate to have several major medical centers and healthcare facilities with world-class faculty and healthcare providers. Only the Director of DC Health has the authority to designate Trauma Centers in the District of Columbia according to District of Columbia Municipal Regulation (DCMR) Chapter 29-559: https://www.dcregs.dc.gov/Common/DCMR/SectionList.aspx?SectionNumber=29-559 The designation of both Trauma and Specialty Centers must be consistent with the National Guidelines or National Standards as mandated in the Emergency Medical Services Act of 2008. There are three criteria that must be met before the Director designates a Trauma Level in a healthcare facility: 1. Verification by the American College of Surgeons Committee on Trauma that the facility meets the requirements for one of the four levels of service consistent with the criteria and resource capacity for Optimal Care of the Injured Patient by the American College of Surgeons Committee on Trauma (https://www.facs.org/-/media/files/quality- programs/trauma/vrc-resources/resources-for-optimal-care.ashx). Information on the Verification, Review and Consultation Program can be found at https://www.facs.org/quality-programs/trauma/tqp/center-programs/vrc/about and https://www.facs.org/quality-programs/trauma/tqp/center-programs/vrc/process 2. Participation in the District of Columbia Trauma Plan which coordinated all of the healthcare resources within the District and helps to protect and provide for the citizens and visitors. 3. Designated Trauma Centers must share the medical data collected by the Trauma service for Continuous Quality Improvement.