Nursing Unit Descriptions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arizona Guidelines for Field Triage of Injured Patients (Regional Modifications Are Permissible)
Arizona Guidelines for Field Triage of Injured Patients (Regional modifications are permissible) FIELD TRIAGE DECISION SCHEME Measure vital signs and level of consciousness Glasgow Coma Scale ≤13 Systolic blood pressure (mmHg) <90 mmHg Step One Respiratory rate <10 or >29 breaths per minute (<20 in infant aged < 1 year1), or need for ventilator support YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess anatomy of injury. patients. These patients should be transported preferentially to the highest level of care within the trauma system. • All penetrating injuries to head, neck, torso, and extremities proximal to elbow or knee • Chest wall instability or deformity (e.g., flail chest) • Two or more proximal long-bone fractures • Crushed, de-gloved, mangled, or pulseless extremity Step Two3 • Amputation proximal to wrist or ankle • Pelvic fractures • Open or depressed skull fracture • Paralysis YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess mechanism of injury patients. These patients should be transported preferentially to the highest level of care within the and evidence of high-energy trauma system. impact. • Falls o Adults: >20 feet (one story is equal to 10 feet) 4 o Children : >10 feet or two or three times the height of the child • High-risk auto crash 5 Intrusion , including roof: >12 inches occupant site; >18 inches any site Step Three3 o o Ejection (partial or complete) from automobile o Death in same passenger compartment o Vehicle telemetry data consistent with high risk of injury 6 • Auto vs. -

Medical Policy
bmchp.org | 888-566-0008 wellsense.org | 877-957-1300 Medical Policy Ambulatory Cardiac Monitors (Excluding Holter Monitors) Policy Number: OCA 3.35 Version Number: 24 Version Effective Date: 03/01/21 + Product Applicability All Plan Products Well Sense Health Plan Boston Medical Center HealthNet Plan Well Sense Health Plan MassHealth Qualified Health Plans/ConnectorCare/Employer Choice Direct Senior Care Options ◊ Notes: + Disclaimer and audit information is located at the end of this document. ◊ The guidelines included in this Plan policy are applicable to members enrolled in Senior Care Options only if there are no criteria established for the specified service in a Centers for Medicare & Medicaid Services (CMS) national coverage determination (NCD) or local coverage determination (LCD) on the date of the prior authorization request. Review the member’s product-specific benefit documents at www.SeniorsGetMore.org to determine coverage guidelines for Senior Care Options. Policy Summary The Plan considers the use of ambulatory cardiac monitors in the outpatient setting to be medically necessary if the type of ambulatory cardiac monitor is covered for the Plan member and ALL applicable Plan criteria are met, as specified in the Medial Policy Statement and Limitations sections of this policy. Plan prior authorization is required. When the device is covered for the member, medically necessary ambulatory cardiac monitors utilized in the outpatient setting may include ambulatory cardiac event monitors, mobile cardiac outpatient telemetry, and/or single-use external ambulatory electrocardiographic monitoring patches available by prescription. Ambulatory Cardiac Monitors (Excluding Holter Monitors) + Plan refers to Boston Medical Center Health Plan, Inc. and its affiliates and subsidiaries offering health coverage plans to enrolled members. -
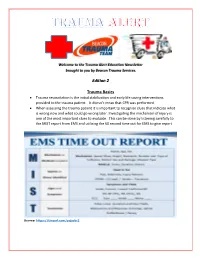
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

Sepsis: a Guide for Patients & Relatives
SEPSIS: A GUIDE FOR PATIENTS & RELATIVES CONTENTS ABOUT SEPSIS ABOUT SEPSIS: INTRODUCTION P3 What is sepsis? In the UK, at least 150,000* people each year suffer from serious P4 Why does sepsis happen? sepsis. Worldwide it is thought that 3 in a 1000 people get sepsis P4 Different types of sepsis P4 Who is at risk of getting sepsis? each year, which means that 18 million people are affected. P5 What sepsis does to your body Sepsis can move from a mild illness to a serious one very quickly, TREATMENT OF SEPSIS which is very frightening for patients and their relatives. P7 Why did I need to go to the Critical Care Unit? This booklet is for patients and relatives and it explains sepsis P8 What treatment might I have had? and its causes, the treatment needed and what might help after P9 What other help might I have received in the Critical Care Unit? having sepsis. It has been written by the UK Sepsis Trust, a charity P10 How might I have felt in the Critical Care Unit? which supports people who have had sepsis and campaigns to P11 How long might I stay in the Critical Care Unit and hospital? raise awareness of the illness, in collaboration with ICU steps. P11 Moving to a general ward and The Outreach Team/Patient at Risk Team If a patient cannot read this booklet for him or herself, it may be helpful for AFTER SEPSIS relatives to read it. This will help them to understand what the patient is going through and they will be more able to support them as they recover. -

Emergency Department Resuscitation of the Critically Ill Review by Stephen C
BOOK AND MEDIA REVIEW Emergency Department Resuscitation of the Critically Ill Review by Stephen C. Morris, MD, MPH 0196-0644/$-see front matter Copyright © 2018 by the American College of Emergency Physicians. Emergency Department Resuscitation of the crashing morbidly obese patient reviews some of the nuanced Critically Ill management we should be striving for as more of our patients become obese, such as specific airway and ventilation Winters ME, Bond MC, Marcolini EG, et al management and use of ideal versus total body weight American College of Emergency Physicians calculations for critical-care-specific medications. Consider It was with great pleasure that I agreed to review the another example from the chapter on left ventricular assist second edition of Emergency Department Resuscitation of the devices. Although these patients have long been the domain Critically Ill, by Michael E. Winters. I had read and relied of specialty centers, with complex physiology and on the first edition posttraining. Like most who work in complications, the longevity now offered by the devices will emergency medicine, I practice a great deal of critical care; ultimately make them the domain of the community however, I have not completed a fellowship in critical care, emergency department. Additionally, at the cutting edge of nor do I review critical care literature with the level of our practice, the text contains a chapter on extracorporeal scrutiny that I would like. For those of us who want to membrane oxygenation, with a discussion of the practical ensure that we are up to date to guarantee clinical and clinical aspects of implementation. -

A BRI H IEF HISTO Howard R. C ORY of TH the Champion, K HE
A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris The Eastern Association for the Surgery of Trauma (EAST) was founded by a group of surgeons each of whom had somewhat established themselves in the field of trauma and surgical critical care by the early 1980s and were in the process of developing these disciplines and mentoring young surgeons. EAST has widely exceeded the original aspirations of that group of then-young surgeons. To understand why EAST was created and why it succeeded, it is necessary to glance back to the mid 1980s. The notion of EAST occurred in 1985 within a context of a growing demand for organized trauma care but no appropriate opportunities for young aspiring trauma surgeons to exchange knowledge, discuss advances in patient care, or develop their careers in this field within the discipline of surgery. No vehicle adequately nurtured young surgeons into the field of trauma. Today, EAST is an established and respected surgical organization reaching its 25-year mark with membership (Figure 1) of 1363 now exceeding that of the premier global trauma organization, the American Association for the Surgery of Trauma (AAST) (1227 members). Then The world of the young trauma surgeon in the early to mid 1980s was a very different place than it is more than 25 years later. -
Needs Assessment for New Trauma Center Development in the Commonwealth of Pennsylvania 2014
WHITE PAPER ON NEEDS ASSESSMENT FOR NEW TRAUMA CENTER DEVELOPMENT IN THE COMMONWEALTH OF PENNSYLVANIA 2014 Purpose Currently new trauma center development in Pennsylvania—with limited exception—is driven by competitive financial and hospital/healthcare system imperatives. The Pennsylvania Trauma Systems Foundation strongly recommends that going forward, new trauma center applications be based on a needs assessment process so as to optimize distribution of trauma centers in the trauma system and thereby provide optimal trauma care for the citizens of the Commonwealth of Pennsylvania. A guide for such a needs assessment is provided in this paper. Introduction Trauma systems have developed based on the sole precept that optimal recovery from traumatic injury is best achieved through the organization of prehospital and hospital preparedness and capability into a codified continuum of care. A codified continuum of care that is designated/accredited on a regular basis by qualified organizations such as the Pennsylvania Trauma Systems Foundation (PTSF). It is undisputed that trauma centers in states such as Pennsylvania have significantly improved the public health for citizens of the Commonwealth. Trauma is the fifth leading cause of death in Pennsylvania. A Pa. Department of Health study demonstrated a 30% reduced chance of death for severely injured patients treated in an accredited trauma center. In 2012, 95.6% of the 40,479 trauma qualifying patients treated at a trauma center survived. Currently, there are a total of 32 trauma centers in PA as noted below. 1 Figure 1 Source: http://www.rural.palegislature.us/demographics_rural_urban_counties.html As is readily appreciated, the majority of trauma centers are in the most populated counties (Philadelphia and Allegheny) with large areas of the state seemingly having little or no ready access to organized trauma care. -

History of Cardiac Trauma Surgery
History of cardiac trauma surgery A J Nicol, MB ChB, FCS (SA), PhD; P H Navsaria, MB ChB, FCS (SA), MMed (Surg); D Kahn, MB ChB, FCS (SA), ChM Department of Surgery, Groote Schuur Hospital, Cape Town, South Africa Corresponding author: A Nicol ([email protected]) The ancient Egyptians, although realising the diaphragm, of the small intestine, of the coronary artery and that blood in the the anatomical importance of the heart, stomach and of the liver is deadly.’[8,9] Aristotle pericardial sac could compress the heart and were largely responsible for the aura of (384 - 322 BC) wrote that ‘The heart again restrict its movement.[17] mysticism and superstition that enveloped is the only one of the viscera, and indeed the heart for centuries. The Egyptian Book the only part of the body, that is unable to The nihilism surrounding cardiac injuries of the Dead (c. 1567 BC) describes how, on tolerate any serious affection. This is but what continued and in 1804 John Bell published entry to the underworld, the jackal-headed might reasonably be expected. For, if the his Discourses of Nature and Care of Wounds, Anubis weighed the heart of the deceased primary or dominant part be diseased, there declaring that ‘there is so little to be done … against a statue of the goddess of truth and is nothing from which the other parts which and the signs and consequences are so clear, justice.[1,2] If the heart weighed the same, the depend upon it can derive sucour’.[10,11] Celsus that it is a waste of time to speak longer of dead person was admitted ‘to the company (1st century AD) recognised the clinical wounds of the heart’.[5,18] of Osiris and the blessed; if not, if his heart features of shock associated with a cardiac was heavy and laden with sin, it was cast to injury when he wrote in De Medicina that, There is dispute over who should be named the devouring beast Ammit’.[3] ‘When the heart is wounded much blood as the first modern cardiac surgeon. -

Trauma, Surgical Critical Care and Acute Care Surgery Services
Trauma, Surgical Critical Care and Acute Care Surgery Services Region’s most experienced nationally verified Level I trauma center The University of Kansas Hospital is the largest regional resource for trauma and acute care surgery. Our multidisciplinary team provides expert care from the time of injury or illness through the patient’s post-hospitalization rehabilitation. The University of Kansas Hospital focuses this specialty practice on the 3 facets of acute care surgery: emergency surgery, trauma surgery and surgical critical care. Our trauma and acute care specialists are in the hospital 24 hours a day, 7 days a week, providing expert surgical care. We specialize in high-acuity surgical and trauma patients with multisystem injuries and complex surgical conditions. • Because we see a large volume of patients, we excel at providing care to surgical and trauma patients. • Our comprehensive approach to care involves a multidisciplinary team that specifically specializes in caring for acute surgical and trauma patients. • As part of an academic medical center, we are active in surgical research, forging new techniques that lead to improved care and recovery. • We are continually focused on quality improvement for optimal outcomes. PB200320120 Specialized care team Level I trauma care Trauma, critical and acute care Concussion management Trauma and acute care surgery patients The Level I Trauma Center at The University of Our surgeons are board-certified in general Timely and effective concussion treatment receive comprehensive treatment from a Kansas Hospital serves the highest volume of surgery and surgical critical care. They provide is important for recovery. Our concussion multidisciplinary team of professionals, each trauma patients in the region. -

The Nebraska Office of Emergency Health Systems Trauma Program Is Pleased That You Wish to Participate in the Statewide Trauma System
Revised July 2019 INSTRUCTIONS FOR FILLING OUT PRE-REVIEW QUESTIONNAIRE (PRQ) The Nebraska Office of Emergency Health Systems Trauma Program is pleased that you wish to participate in the statewide trauma system. The Nebraska Statewide Trauma System is comprised of hospitals and clinics striving to improve trauma patient care. Through this system all facilities offering trauma care may become centers of excellence. Thank you for participating in this process. In order to prepare for your on-site review, please complete this questionnaire. All answers should directly follow the questions. The entire questionnaire is available on the web in a downloadable format @ http://dhhs.ne.gov/Pages/EHS-Statewide-Trauma-System-of-Care.aspx. The PRQ should be completed electronically if possible otherwise, you may submit a hard copy. Note: If a hard copy is printed a color printer should be used so that information and questions printed in blue appear on the page to the applicant. Return the completed questionnaire to: Sherri Wren EHS Trauma Program Manager Office of Emergency Health Systems P.O. Box 95026 Lincoln, NE 68509-5026 Phone: (402) 471-0539 E-mail: [email protected] If you have questions or concerns while filling out the PRQ, please contact: State of Nebraska Trauma Nurse Specialist OR your Regional Trauma Program Manager (please reference website list of Designated Trauma Centers on the website cited above for names and contact information). I. PURPOSE: A. The purpose of this questionnaire for Consultation Visits is: 1. To provide your institution with an outline of what site visitors will be discussing with you. -

Bed-Based Ballistocardiography: Dataset and Ability to Track Cardiovascular Parameters
sensors Article Bed-Based Ballistocardiography: Dataset and Ability to Track Cardiovascular Parameters Charles Carlson 1,* , Vanessa-Rose Turpin 2, Ahmad Suliman 1 , Carl Ade 2, Steve Warren 1 and David E. Thompson 1 1 Mike Wiegers Department of Electrical and Computer Engineering, Kansas State University, Manhattan, KS 66506, USA; [email protected] (A.S.); [email protected] (S.W.); [email protected] (D.E.T.) 2 Department of Kinesiology, Kansas State University, Manhattan, KS 66506, USA; [email protected] (V.-R.T.); [email protected] (C.A.) * Correspondence: [email protected] Abstract: Background: The goal of this work was to create a sharable dataset of heart-driven signals, including ballistocardiograms (BCGs) and time-aligned electrocardiograms (ECGs), photoplethysmo- grams (PPGs), and blood pressure waveforms. Methods: A custom, bed-based ballistocardiographic system is described in detail. Affiliated cardiopulmonary signals are acquired using a GE Datex CardioCap 5 patient monitor (which collects ECG and PPG data) and a Finapres Medical Systems Finometer PRO (which provides continuous reconstructed brachial artery pressure waveforms and derived cardiovascular parameters). Results: Data were collected from 40 participants, 4 of whom had been or were currently diagnosed with a heart condition at the time they enrolled in the study. An investigation revealed that features extracted from a BCG could be used to track changes in systolic blood pressure (Pearson correlation coefficient of 0.54 +/− 0.15), dP/dtmax (Pearson correlation coefficient of 0.51 +/− 0.18), and stroke volume (Pearson correlation coefficient of 0.54 +/− 0.17). Conclusion: A collection of synchronized, heart-driven signals, including BCGs, ECGs, PPGs, and blood pressure waveforms, was acquired and made publicly available.