Anytown Trauma Center Trauma Protocols
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Arizona Guidelines for Field Triage of Injured Patients (Regional Modifications Are Permissible)
Arizona Guidelines for Field Triage of Injured Patients (Regional modifications are permissible) FIELD TRIAGE DECISION SCHEME Measure vital signs and level of consciousness Glasgow Coma Scale ≤13 Systolic blood pressure (mmHg) <90 mmHg Step One Respiratory rate <10 or >29 breaths per minute (<20 in infant aged < 1 year1), or need for ventilator support YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess anatomy of injury. patients. These patients should be transported preferentially to the highest level of care within the trauma system. • All penetrating injuries to head, neck, torso, and extremities proximal to elbow or knee • Chest wall instability or deformity (e.g., flail chest) • Two or more proximal long-bone fractures • Crushed, de-gloved, mangled, or pulseless extremity Step Two3 • Amputation proximal to wrist or ankle • Pelvic fractures • Open or depressed skull fracture • Paralysis YES NO Transport to a Trauma Center2. Steps 1 and 2 attempt to identify the most seriously injured Assess mechanism of injury patients. These patients should be transported preferentially to the highest level of care within the and evidence of high-energy trauma system. impact. • Falls o Adults: >20 feet (one story is equal to 10 feet) 4 o Children : >10 feet or two or three times the height of the child • High-risk auto crash 5 Intrusion , including roof: >12 inches occupant site; >18 inches any site Step Three3 o o Ejection (partial or complete) from automobile o Death in same passenger compartment o Vehicle telemetry data consistent with high risk of injury 6 • Auto vs. -

Emergency Physician Recognition of Adverse Drug-Related Events in Elder Patients Presenting to an Emergency Department
ACAD EMERG MED d March 2005, Vol. 12, No. 3 d www.aemj.org 197 Emergency Physician Recognition of Adverse Drug-related Events in Elder Patients Presenting to an Emergency Department Corinne Miche` le Hohl, MD, CCFP, FRCPC, Caroline Robitaille, BPharm, MSc, Vicky Lord, BPharm, MSc, Jerrald Dankoff, MD, CSPQ, Antoinette Colacone, BSc, CCRA, Luc Pham, BSc, Anick Be´ rard, PhD, Jocelyne Pe´ pin,BPharm,MSc,MarcAfilalo,MD,FRCPC Abstract Objectives: The authors examined the ability of emergency ADREs that were not associated with the chief complaint physicians (EPs) to recognize adverse drug-related events (32.1%; 95% CI = 14.8% to 49%). EPs recognized six of seven (ADREs) in elder patients presenting to the emergency severe ADREs (85.7%), 13 of 23 moderate ADREs (56.5%; department (ED). Methods: This was a prospective obser- 95% CI = 36.8% to 77%), and none of the mild ADREs. vational study of patients at least 65 years of age who Recognition of ADREs varied with medication class. presented to the ED. ADREs were identified using a vali- Conclusions: EP performance was superior at identifying dated, standardized scoring system. EP recognition of severe ADREs relating to the patients’ chief complaints. ADREs was assessed through physician interview and However, EP performance was suboptimal with respect to subsequent chart review. Results: A total of 161 patients identifying ADREs of lower severity, having missed a signif- were enrolled in the study. Thirty-seven ADREs were icant number of ADREs of moderate severity as well as ones identified, which occurred in 26 patients (16.2%; 95% unrelated to the patients’ chief complaints. -
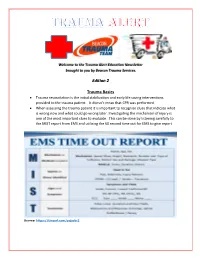
Edition 2 Trauma Basics
Welcome to the Trauma Alert Education Newsletter brought to you by Beacon Trauma Services. Edition 2 Trauma Basics Trauma resuscitation is the initial stabilization and early life saving interventions provided to the trauma patient. It doesn’t mean that CPR was performed. When assessing the trauma patient it is important to recognize clues that indicate what is wrong now and what could go wrong later. Investigating the mechanism of injury is one of the most important clues to evaluate. This can be done by listening carefully to the MIST report from EMS and utilizing the 60 second time out for EMS to give report Source: https://tinyurl.com/ycjssbr3 What is wrong with me? EMS MIST 43 year old male M= unrestrained driver, while texting drove off road at 40 mph into a tree, with impact to driver’s door, 20 minute extrication time I= Deformity to left femur, pain to left chest, skin pink and warm S= B/P- 110/72, HR- 128 normal sinus, RR- 28, Spo2- 94% GCS=14 (Eyes= 4 Verbal= 4 Motor= 6) T= rigid cervical collar, IV Normal Saline at controlled rate, splint left femur What are your concerns? (think about the mechanism and the EMS report), what would you prepare prior to the patient arriving? Ten minutes after arrival in the emergency department the patient starts to have shortness of breath with stridorous sound. He is now diaphoretic and pale. B/P- 80/40, HR- 140, RR- 36 labored. Absent breath sounds on the left. What is the patients’ underlying problem?- Answer later in the newsletter Excellence in Trauma Nursing Award Awarded in May for National Trauma Month This year the nominations were very close so we chose one overall winner and two honorable mentions. -
Advanced Trauma Management for Emergency Physicians: Updates
The Institute for Emergency Department Clinical Quality Improvement Advanced Trauma Management for Emergency Physicians: www.EDQualityInstitute.org Updates and Best Practices 14-15 December, 2020 Interactive CME Course – Live Streamed from Boston The Institute for Emergency Department Clinical Quality Improvement Promoting excellence in emergency department operations, clinical quality, and patient safety through a commitment to quality improvement, clinical education, international collaboration, and research Offered by BIDMC Department of Emergency Medicine, a Harvard Medical School teaching hospital Course Description Advanced Trauma Management for the Emergency Physician is a 2-day, 13-hour course that provides updates, best practices, and new pathways & protocols regarding the acute care of major trauma patients, from Emergency Department arrival through hospital admission/discharge. The course will focus on advanced, state-of- the-art clinical knowledge and skills, with an emphasis on teamwork, non-technical skills, and best practices in ED management. The goal of this advanced trauma management course is to prepare emergency clinicians, who already have a strong base in trauma care, to quickly and accurately assess and provide high-quality care for trauma patients. Emphasis will be on optimizing outcomes for patients presenting with high-risk traumatic injuries. Advanced Trauma Management for the Emergency Physician is delivered by the Department of Emergency Medicine at Harvard Medical Faculty Physicians at Beth Israel Deaconess Medical Center, a level 1 trauma center. This course is relevant for clinicians working in emergency medicine, critical care, and urgent care and can be applied in the trauma center, community hospital, or remote setting. Optimized for Remote Education The program is optimized for distance learning. -

Title: ED Trauma: Trauma Nurse Clinical Resuscitation
Title: ED Trauma: Trauma Nurse Clinical Resuscitation Document Category: Clinical Document Type: Policy Department/Committee Owner: Practice Council Original Date: Approved By (last review): Director of Emergency Services, Approval Date: 07/28/2014 Trauma Medical Director, Medical Director Emergency (Complete history at end of document.) Services POLICY: To provide immediate, effective and efficient patient care to the trauma patient, designated nursing staff will respond to the trauma room when a trauma page is received. TRAUMA CONTROL NURSE: 1) Role: a) The trauma control nurse (TCN) is a registered nurse (RN) with specialized training in the care of the traumatized patient, and who will function as the trauma team’s lead nurse. b) The TCN shall have successfully completed the Trauma Nurse Core Course (TNCC), Advanced Cardiac Life Support (ACLS), Emergency Nurse Pediatric Course (ENPC) or Pediatric Advanced Life Support (PALS), and role orientation with trauma services. c) Full-time employee or regularly scheduled part-time Emergency Department (ED) nurse. d) RN must have 6 months of LMH ED experience. 2) Trauma Control Duties: a) Inspects and stocks trauma room at beginning of each shift and after each trauma patient is discharged from the ED. b) Attempts to maintain trauma room temperature at 80-82 degrees Fahrenheit. c) Communicates with pre-hospital personnel to obtain patient information and prior field treatment and response. d) Makes determination that a patient meets Type I or Type II criteria and immediately notifies LMH’s Call System to initiate the Trauma Activation System. e) Assists physician with orders as directed. f) Acts as liaison with patient’s family/law enforcement/emergency medical services (EMS)/flight crews. -

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

Emergency Department Resuscitation of the Critically Ill Review by Stephen C
BOOK AND MEDIA REVIEW Emergency Department Resuscitation of the Critically Ill Review by Stephen C. Morris, MD, MPH 0196-0644/$-see front matter Copyright © 2018 by the American College of Emergency Physicians. Emergency Department Resuscitation of the crashing morbidly obese patient reviews some of the nuanced Critically Ill management we should be striving for as more of our patients become obese, such as specific airway and ventilation Winters ME, Bond MC, Marcolini EG, et al management and use of ideal versus total body weight American College of Emergency Physicians calculations for critical-care-specific medications. Consider It was with great pleasure that I agreed to review the another example from the chapter on left ventricular assist second edition of Emergency Department Resuscitation of the devices. Although these patients have long been the domain Critically Ill, by Michael E. Winters. I had read and relied of specialty centers, with complex physiology and on the first edition posttraining. Like most who work in complications, the longevity now offered by the devices will emergency medicine, I practice a great deal of critical care; ultimately make them the domain of the community however, I have not completed a fellowship in critical care, emergency department. Additionally, at the cutting edge of nor do I review critical care literature with the level of our practice, the text contains a chapter on extracorporeal scrutiny that I would like. For those of us who want to membrane oxygenation, with a discussion of the practical ensure that we are up to date to guarantee clinical and clinical aspects of implementation. -

Implementing Public-Access Programs for Automated External Defibrillation
Correspondance that approving new drugs more rapidly Therapeutic Products Program internal constitute only 4.6% of drugs ap- does not compromise safety, we are processes was 188 days (range 74–376 proved in the United States at least 1 better off putting our limited resources days).2 Approval times are much longer year before approval in Canada in the into other areas such as improving for 2 reasons: considerable downtime 7-year period. Canada’s woefully inadequate postmar- occurs between the receipt of the appli- Finally, I endorse the recommen- keting evaluation system. cation and the start of the scientific re- dation that Canada’s inadequate post- view, and the separate assessment of marketing surveillance system should Joel Lexchin manufacturing and stability data is often be improved and have proposed new Emergency physician not coordinated with the safety and effi- approaches that could be adopted in University Health Network cacy evaluation. Canada.5–7 However, the unnecessary Toronto, Ont. An evaluation of the importance of a delays in Canada’s review and ap- Barbara Mintzes new drug’s therapeutic potential should proval system should also be elimi- Department of Health Care be based not simply on the lack of a nated and Canada’s performance stan- & Epidemiology current treatment, which is the practice dard of 355 days for all new drug University of British Columbia of the Patented Medicine Prices Re- applications achieved. In that way, Vancouver, BC view Board, but rather it should be Canadians will no longer have to ex- based on several factors. The US Food perience delayed access to potentially References 1. -
Needs Assessment for New Trauma Center Development in the Commonwealth of Pennsylvania 2014
WHITE PAPER ON NEEDS ASSESSMENT FOR NEW TRAUMA CENTER DEVELOPMENT IN THE COMMONWEALTH OF PENNSYLVANIA 2014 Purpose Currently new trauma center development in Pennsylvania—with limited exception—is driven by competitive financial and hospital/healthcare system imperatives. The Pennsylvania Trauma Systems Foundation strongly recommends that going forward, new trauma center applications be based on a needs assessment process so as to optimize distribution of trauma centers in the trauma system and thereby provide optimal trauma care for the citizens of the Commonwealth of Pennsylvania. A guide for such a needs assessment is provided in this paper. Introduction Trauma systems have developed based on the sole precept that optimal recovery from traumatic injury is best achieved through the organization of prehospital and hospital preparedness and capability into a codified continuum of care. A codified continuum of care that is designated/accredited on a regular basis by qualified organizations such as the Pennsylvania Trauma Systems Foundation (PTSF). It is undisputed that trauma centers in states such as Pennsylvania have significantly improved the public health for citizens of the Commonwealth. Trauma is the fifth leading cause of death in Pennsylvania. A Pa. Department of Health study demonstrated a 30% reduced chance of death for severely injured patients treated in an accredited trauma center. In 2012, 95.6% of the 40,479 trauma qualifying patients treated at a trauma center survived. Currently, there are a total of 32 trauma centers in PA as noted below. 1 Figure 1 Source: http://www.rural.palegislature.us/demographics_rural_urban_counties.html As is readily appreciated, the majority of trauma centers are in the most populated counties (Philadelphia and Allegheny) with large areas of the state seemingly having little or no ready access to organized trauma care. -

Management of Acute Liver Failure In
Management of Acute Liver Failure in ICU Philip Berry MRCP, Clinical Research Fellow, Institute of Liver Studies, Kings College Hospital, London, UK Email: [email protected] Self assessment questions Scenario: A twenty-year-old female is brought into the Emergency Department having been found unconscious in her bedsit. There is no other recent history. She did not respond to a bolus of 50% dextrose in the ambulance, despite having an unrecordable blood glucose when tested by the paramedics. While she is being intubated on account of reduced level of consciousness, an arterial blood gas sample reveals profound lactic acidosis (pH 7.05, pCO2 2.5 kPa, base deficit – 10, lactate 13 mg/L). Blood pressure is 95/50 mmHg. 1. What are the possible explanations for her presentation? Laboratory tests demonstrate hepatocellular necrosis (AST 21,000 U/L) and coagulopathy (INR 9.1) with thrombocytopenia (platelet count 26 x 109/L). Acute liver failure appears the most likely diagnosis. 2. What are the most likely causes of acute liver failure (ALF) in this previously well patient? Her mean arterial blood pressure remains low (50mmHg) after 3 litres of colloid and crystalloid. The casualty nurse, who is doing half-hourly neurological observations, reports reduced pupillary response to light. 3. What severe complications of ALF may result in death within hours, and what are the immediate management priorities for this patient? Introduction Successful management of this rare but potentially devastating disorder relies on early recognition. The hallmark of acute liver failure (ALF) is encephalopathy (ranging from a subtle alterations in consciousness level to coma) in the context of an acute, severe liver injury. -

Emergency Medicine Profile
Emergency Medicine Profile Updated December 2019 1 Table of Contents Slide . General Information 3-6 . Total number & number/100,000 population by province, 2019 7 . Number/100,000 population, 1995-2019 8 . Number by gender & year, 1995-2019 9 . Percentage by gender & age, 2019 10 . Number by gender & age, 2019 11 . Percentage by main work setting, 2019 12 . Percentage by practice organization, 2017 13 . Hours worked per week (excluding on-call), 2019 14 . On-call duty hours per month, 2019 15 . Percentage by remuneration method 16 . Professional & work-life balance satisfaction, 2019 17 . Number of retirees during the three year period of 2016-2018 18 . Employment situation, 2017 19 . Links to additional resources 20 2 General information Emergency medicine focuses on the recognition, evaluation and care of patients who are acutely ill or injured. It is a high-pressure, fast-paced specialty that, because of its diversity, requires a broad base of medical knowledge and a variety of well-honed clinical and technical skills. Emergency physicians (emergentologists) must be prepared to treat patients of all ages and a nearly infinite variety of conditions and degrees of illness – often before a definite diagnosis is made and within time-restricted circumstances. The approach to treatment in an emergency department can vary dramatically from case to case, even for the same medical condition, depending on whether it’s a pediatric patient versus a geriatric patient. Emergency physicians need a number of personal strengths, including physical and emotional toughness, confidence, composure, ability to multi task and strong interpersonal skills. They must also be willing and able to do shift work. -

The Nebraska Office of Emergency Health Systems Trauma Program Is Pleased That You Wish to Participate in the Statewide Trauma System
Revised July 2019 INSTRUCTIONS FOR FILLING OUT PRE-REVIEW QUESTIONNAIRE (PRQ) The Nebraska Office of Emergency Health Systems Trauma Program is pleased that you wish to participate in the statewide trauma system. The Nebraska Statewide Trauma System is comprised of hospitals and clinics striving to improve trauma patient care. Through this system all facilities offering trauma care may become centers of excellence. Thank you for participating in this process. In order to prepare for your on-site review, please complete this questionnaire. All answers should directly follow the questions. The entire questionnaire is available on the web in a downloadable format @ http://dhhs.ne.gov/Pages/EHS-Statewide-Trauma-System-of-Care.aspx. The PRQ should be completed electronically if possible otherwise, you may submit a hard copy. Note: If a hard copy is printed a color printer should be used so that information and questions printed in blue appear on the page to the applicant. Return the completed questionnaire to: Sherri Wren EHS Trauma Program Manager Office of Emergency Health Systems P.O. Box 95026 Lincoln, NE 68509-5026 Phone: (402) 471-0539 E-mail: [email protected] If you have questions or concerns while filling out the PRQ, please contact: State of Nebraska Trauma Nurse Specialist OR your Regional Trauma Program Manager (please reference website list of Designated Trauma Centers on the website cited above for names and contact information). I. PURPOSE: A. The purpose of this questionnaire for Consultation Visits is: 1. To provide your institution with an outline of what site visitors will be discussing with you.