The Roots of Periodontology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Chlorhexidine in Maintaining Periodontal Health
International Journal of Dentistry Research 2016; 1(1): 31-33 Review Article Importance of Chlorhexidine in Maintaining Periodontal IJDR 2016; 1(1): 31-33 December Health © 2016, All rights reserved www.dentistryscience.com Dr. Manpreet Kaur*1, Dr. Krishan Kumar1 1 Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak-124001, Haryana, India Abstract Plaque is responsible for periodontal diseases. In order to prevent occurrence and progression of periodontal disease, removal of plaque becomes important. Mechanical tooth cleaning aids such as toothbrushes, dental floss, interdental brushes are used for removal of plaque. However, in some cases, chemical agents are used as an adjunct to mechanical methods to facilitate plaque control and prevent gingivitis. Chlorhexidine (CHX) mouthwash is the most commonly used and is considered as gold standard chemical agent. In this review, mechanism of action and other properties of CHX are discussed. Keywords: Plaque, Chemical agents, Chlorhexidine (CHX). INTRODUCTION Dental plaque is primary etiologic factor responsible for gingivitis and periodontitis [1]. Mechanical plaque control using toothbrushes, interdental brushes, dental floss prevent occurrence of gingivitis. However, in majority of population, mechanical methods of plaque control are ineffective due to less time spent[2] for plaque removal and lack of consistency. These limitations necessitate use of chemical plaque control agents as an adjunct to mechanical plaque control. Among various chemical agents, chlorhexidine (CHX) is considered to be a gold standard chemical agent for plaque control. Its structural formula consists of two symmetric 4-chlorophenyl rings and two biguanide groups connected by a central hexamethylene chain. Mechanism of action for CHX CHX is bactericidal and is effective against gram-positive bacteria, gram-negative bacteria and yeast organisms. -
Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Periodontal Practice Patterns
PERIODONTAL PRACTICE PATTERNS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of the Ohio State University By Janel Kimberlay Yu, D.D.S. Graduate Program in Dentistry The Ohio State University 2010 Dissertation Committee: Dr. Angelo Mariotti, Advisor Dr. Jed Jacobson Dr. Eric Seiber Copyright by Janel Kimberlay Yu 2010 Abstract Background: Differences in the rates of dental services between geographic regions are important since major discrepancies in practice patterns may suggest an absence of evidence-based clinical information leading to numerous treatment plans for similar dental problems and the misallocation of limited resources. Variations in dental care to patients may result from characteristics of the periodontist. Insurance claims data in this study were compared to the characteristics of periodontal providers to determine if variations in practice patterns exist. Methods: Claims data, between 2000-2009 from Delta Dental of Ohio, Michigan, Indiana, New Mexico, and Tennessee, were examined to analyze the practice patterns of 351 periodontists. For each provider, the average number of select CDT periodontal codes (4000-4999), implants (6010), and extractions (7140) were calculated over two time periods in relation to provider variable, including state, urban versus rural area, gender, experience, location of training, and membership in organized dentistry. Descriptive statistics were performed to depict the data using measures of central tendency and measures of dispersion. ii Results: Differences in periodontal procedures were present across states. Although the most common surgical procedure in the study period was osseous surgery, greater increases over time were observed in regenerative procedures (bone grafts, biologics, GTR) when compared to osseous surgery. -

Classification and Diagnosis of Aggressive Periodontitis
Received: 3 November 2016 Revised: 11 October 2017 Accepted: 21 October 2017 DOI: 10.1002/JPER.16-0712 2017 WORLD WORKSHOP Classification and diagnosis of aggressive periodontitis Daniel H. Fine1 Amey G. Patil1 Bruno G. Loos2 1 Department of Oral Biology, Rutgers School Abstract of Dental Medicine, Rutgers University - Newark, NJ, USA Objective: Since the initial description of aggressive periodontitis (AgP) in the early 2Department of Periodontology, Academic 1900s, classification of this disease has been in flux. The goal of this manuscript is to Center of Dentistry Amsterdam (ACTA), review the existing literature and to revisit definitions and diagnostic criteria for AgP. University of Amsterdam and Vrije Universiteit, Amsterdam, The Netherlands Study analysis: An extensive literature search was performed that included databases Correspondence from PubMed, Medline, Cochrane, Scopus and Web of Science. Of 4930 articles Dr. Daniel H. Fine, Department of Oral reviewed, 4737 were eliminated. Criteria for elimination included; age > 30 years old, Biology, Rutgers School of Dental Medicine, Rutgers University - Newark, NJ. abstracts, review articles, absence of controls, fewer than; a) 200 subjects for genetic Email: fi[email protected] studies, and b) 20 subjects for other studies. Studies satisfying the entrance criteria The proceedings of the workshop were were included in tables developed for AgP (localized and generalized), in areas related jointly and simultaneously published in the Journal of Periodontology and Journal of to epidemiology, microbial, host and genetic analyses. The highest rank was given to Clinical Periodontology. studies that were; a) case controlled or cohort, b) assessed at more than one time-point, c) assessed for more than one factor (microbial or host), and at multiple sites. -
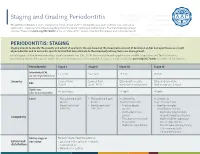
Staging and Grading Periodontitis
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

Tobacco and Your Oral Health
Oral Wellness Series Tobacco and Your Oral Health We all know smoking is bad for us, but did you know that chewing tobacco is just as harmful to your oral health as cigarettes? Tobacco causes bad breath, which nobody likes, but it has far more serious risks to your oral health, including: • Mouth sores • Slow healing after oral surgery • Difficulties correcting cosmetic dental problems • Stained teeth and tongue • Dulled sense of taste and smell The Biggest Risk? Did you know tobacco Cancer. The Centers for Disease Control have linked smoking and use is a huge risk factor tobacco use to oral cancer. Oral cancer is the eighth most common cancer in the U.S., and it’s very difficult to detect. As a result, two- for gum disease? thirds of all cases are diagnosed in late stages, making treatment and survival difficult.1 Tobacco and Gum Disease Tobacco use is also a huge risk factor for gum disease, a leading cause of tooth loss. More than 41% of daily smokers over the age of 65 are toothless because of gum disease, compared to only 20% of non-smokers.2 Maintain good oral health by avoiding tobacco. It keeps your whole body healthier. The Effects of Smoking on Your Gums Smoking reduces blood flow to your gums, cutting Is Smokeless Tobacco Safer? off vital nutrients and preventing bones from healing. Smokeless tobacco—chew, dip and snuff—is not This lets bacteria from tartar infect surrounding tissue, regulated by the FDA so it’s hard to know what’s in it. 3 forming deep pockets between teeth and gums. -

American Academy of Periodontology Task Force Report on the Update to the 1999 Classification of Periodontal Diseases and Conditions*
J Periodontol • July 2015 American Academy of Periodontology Task Force Report on the Update to the 1999 Classification of Periodontal Diseases and Conditions* The American Academy of Periodontology (AAP) peri- 4 mm CAL, and Severe =‡5 mm CAL.’’ Numerous odically publishes reports, statements, and guidelines important studies since 1999 have used similar pa- on a variety of topics relevant to periodontics. These rameters to define periodontitis. For example, the papers are developed by an appointed committee of recent epidemiologic studies outlining the prevalence experts, and the documents are reviewed and ap- of periodontitis in the United States used attachment proved by the AAP Board of Trustees. loss parameters to define various severities of peri- odontitis.2,3 It is recognized that CAL is of importance for the scientific advancement of the knowledge of n 2014, the American Academy of Periodontology periodontitis. However, in clinical practice, measure- Board of Trustees charged a Task Force to develop ment of CAL has proven to be challenging, and is time Ia clinical interpretation of the 1999 Classification consuming. Measuring the location of the cemento- of Periodontal Diseases and Conditions to address enamel junction (CEJ) when the gingival margin is concerns expressed by the education community, the located coronal to the CEJ is difficult and may involve American Board of Periodontology, and the practic- some guesswork when the CEJ is not readily evident ing community that the current Classification pres- via tactile sensation. These issues can result in ex- ents challenges for the education of dental students aminations being performed in which, rather than and implementation in clinical practice. -

Dentine Hypersensitivity: Analysis of Self-Care Products§
Periodontics Periodontics Dentine hypersensitivity: analysis of self-care products§ Cassiano Kuchenbecker Rösing(a) Abstract: Dentine hypersensitivity is a condition that is often present in (b) Tiago Fiorini individuals, leading them to seek dental treatment. It has been described Diego Nique Liberman(b) Juliano Cavagni(b) as an acute, provoked pain that is not attributable to other dental prob- lems. Its actual prevalence is unknown, but it is interpreted as very un- pleasant by individuals. Several therapeutic alternatives are available to (a) Professor of Periodontology; (b)Graduate Student, Graduate Program in Dentistry manage dentine hypersensitivity, involving both in-office treatment and – School of Dentistry, Federal University of home-use products. The aim of this literature review was to evaluate self- Rio Grande do Sul, Porto Alegre, RS, Brazil. care products for managing dentine hypersensitivity. Among the prod- ucts available, dentifrices and fluorides are the most studied self-care products, with positive effects. However, a high percentage of individu- als is affected by the placebo effect. Among dentifrices, those containing potassium salts seem to be the most promising. Dental professionals need to understand the advantages and limitations of these therapies and use this knowledge in a positive approach that might help in decreasing den- tine hypersensitivity among patients. Descriptors: Dentin hypersensitivity; Review; Dental devices, home-care. § Paper presented at the “Oral Health Self-Care Products: Realities and -

Comparative Evaluation of Two Different One-Stage Full-Mouth
ORIGINAL RESEARCH Comparative Evaluation of Two Different One-stage Full-mouth Disinfection Protocols using BANA Assay: A Randomized Clinical Study Arjumand Farooqui1, Vineet V Kini2, Ashvini M Padhye3 ABSTRACT Aim: The aim of this study was to evaluate and compare two different one-stage full-mouth disinfection protocols in the treatment of chronic periodontitis by assessing dental plaque and tongue coat using BANA assay. Materials and methods: The present study was a prospective randomized clinical parallel arm study design including 40 healthy subjects randomly allocated into two groups, i.e., group A (Quirynen’s protocol of one-stage full-mouth disinfection) and group B (Bollen’s protocol of one-stage full-mouth disinfection). Subjects were assessed at baseline and six weeks using plaque index, gingival index, and sulcus bleeding index. Probing depth and relative clinical attachment level were also recorded at six weeks. Winkel tongue coat index and BANA were recorded at 8 weeks using subgingival plaque and tongue coat sample. Results: Both group A and group B demonstrated statistically significant reduction in plaque index, gingival index, sulcus bleeding index, Winkel tongue coat index, reduction in probing depth, and gain in relative clinical attachment level on intragroup comparison. There was no significant difference in BANA assay score of subgingival plaque and tongue coat samples in between group A and group B. Conclusion: From the findings of this study, both Quirynen’s protocol and Bollen’s protocol of one-stage full-mouth disinfection are effective in plaque reduction and tongue coat reduction and achieve comparable clinical healing outcomes. Clinical significance: The difference in duration and mode of use of chlorhexidine as a chemical plaque control agent in the two treatment interventions of Quirynen’s and Bollen’s protocol of one-stage full-mouth disinfection did not demonstrate statistical significance in reducing sulcus bleeding index scores, reducing probing depths, and gain in relative clinical attachment levels. -

Periodontal Health and Gingival Diseases
Received: 9 December 2017 Revised: 11 March 2018 Accepted: 12 March 2018 DOI: 10.1002/JPER.17-0719 2017 WORLD WORKSHOP Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions Iain L.C. Chapple1 Brian L. Mealey2 Thomas E. Van Dyke3 P. Mark Bartold4 Henrik Dommisch5 Peter Eickholz6 Maria L. Geisinger7 Robert J. Genco8 Michael Glogauer9 Moshe Goldstein10 Terrence J. Griffin11 Palle Holmstrup12 Georgia K. Johnson13 Yvonne Kapila14 Niklaus P. Lang15 Joerg Meyle16 Shinya Murakami17 Jacqueline Plemons18 Giuseppe A. Romito19 Lior Shapira10 Dimitris N. Tatakis20 Wim Teughels21 Leonardo Trombelli22 Clemens Walter23 Gernot Wimmer24 Pinelopi Xenoudi25 Hiromasa Yoshie26 1Periodontal Research Group, Institute of Clinical Sciences, College of Medical & Dental Sciences, University of Birmingham, UK 2University of Texas Health Science Center at San Antonio, USA 3The Forsyth Institute, Cambridge, MA, USA 4School of Dentistry, University of Adelaide, Australia 5Department of Periodontology and Synoptic Dentistry, Charité - Universitätsmedizin Berlin, Germany 6Department of Periodontology, Center for Oral Medicine, Johann Wolfgang Goethe-University Frankfurt, Germany 7Department of Periodontology, University of Alabama at Birmingham, USA 8Department of Oral Biology, SUNY at Buffalo, NY, USA 9Faculty of Dentistry, University of Toronto, Canada 10Department of Periodontology, Faculty of -

One-Stage, Full-Mouth Disinfection: Fiction Or Reality?
FOCUS ARTICLE One-Stage, Full-Mouth Disinfection: Fiction or Reality? Marc Quirynen, Wim Teughels, Martine Pauwels, Daniel van Steenberghe Recent research indicated that periopathogens colonize, besides the pockets, also other niches within the oral cavity including: the soft tissues, the saliva, the tongue, and even the tonsils. Since the supragingival plaque and the bacteria in these niches have a major impact on the subgin- gival plaque colonisation but especially on the recolonation after debridement, it seems reason- able to expect that a one-stage, full-mouth disinfection protocol, involving the bacteria over the entire oro-pharyngeal area, has a significantly better outcome when compared to a more staged approach (e.g. with treatments per quadrant). Since several review papers recently discussed the benefits of a one-stage, full-mouth disinfection protocol, pointing to some shortcomings in the our research protocol or with an attempt to compare the data of the new approach with other studies (with unfortunately non comparable approaches), this review paper aims to clarify some of the confusion concerning the benefits of a one-stage, full-mouth disinfection approach. Key words: periodontal breakdown; periodontopathogens; mouth disinfection INTRODUCTION logy, 1996; Slots and Rams, 1991; Socransky and Haffajee, 1992; Wolff et al, 1994). The ef- Periodontal breakdown primarily develops when ficiency of the host defence is partially hereditary the microbial load within a periodontal pocket (Kinane and Hart, 2003) but environmental fac- overrules the local and systemic host defence tors such as bad oral hygiene, smoking, immuno- mechanisms. Such an imbalance occurs in differ- suppressive medication, stress and so on can fur- ent situations, including an aspecific increase in ther impair the immune defence mechanism. -
Periodontitis Have Struggled to Decide If There Are Different Diseases Or Variations of a Single Disease
• Attempts to classify periodontitis have struggled to decide if there are different diseases or variations of a single disease. • There is no evidence to support differentiating “chronic” and “aggressive” periodontitis. • Three forms of periodontitis have been identified: (1) periodontitis, (2) necrotising periodontitis, (3) periodontitis as a direct manifestation of systemic diseases. • A classification system must include complexity and risk factors as well as disease severity. • Individual cases of periodontitis should be characterised according to the stage and grade of the disease. Authors Mariano Sanz and Maurizio Tonetti Published March 2019 European Federation of © European Federation of Periodontology Periodontology Introduction: classifying periodontitis Previous attempts to classify periodontitis have revolved around the question of whether phenotypically different case presentations represent different diseases or variations of a single disease. The internationally accepted classification of periodontitis, published in 1999, provided a workable framework that has been used extensively in both clinical practice and scientific investigation. But this system suffers from significant shortcomings, including substantial overlap, the lack of a clear pathobiology- based distinctions between categories, diagnostic imprecision, and difficulties in implementation. The New Classification from the 2017 World Workshop on Periodontal and Peri- implant Disease and Conditions (“the World Workshop”) reviewed the scientific evidence and reached four main conclusions: 1. There is no evidence of a specific pathophysiology that enables the differentiation of cases as “aggressive” or “chronic” periodontitis or provides guidance for different kinds of intervention. 2. There is little consistent evidence that aggressive and chronic periodontitis are different diseases. But there is evidence that multiple factors, and the interactions between them, influence clinically observable disease outcomes (phenotypes) at the individual level.