Periodontal Practice Patterns
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Chlorhexidine in Maintaining Periodontal Health
International Journal of Dentistry Research 2016; 1(1): 31-33 Review Article Importance of Chlorhexidine in Maintaining Periodontal IJDR 2016; 1(1): 31-33 December Health © 2016, All rights reserved www.dentistryscience.com Dr. Manpreet Kaur*1, Dr. Krishan Kumar1 1 Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak-124001, Haryana, India Abstract Plaque is responsible for periodontal diseases. In order to prevent occurrence and progression of periodontal disease, removal of plaque becomes important. Mechanical tooth cleaning aids such as toothbrushes, dental floss, interdental brushes are used for removal of plaque. However, in some cases, chemical agents are used as an adjunct to mechanical methods to facilitate plaque control and prevent gingivitis. Chlorhexidine (CHX) mouthwash is the most commonly used and is considered as gold standard chemical agent. In this review, mechanism of action and other properties of CHX are discussed. Keywords: Plaque, Chemical agents, Chlorhexidine (CHX). INTRODUCTION Dental plaque is primary etiologic factor responsible for gingivitis and periodontitis [1]. Mechanical plaque control using toothbrushes, interdental brushes, dental floss prevent occurrence of gingivitis. However, in majority of population, mechanical methods of plaque control are ineffective due to less time spent[2] for plaque removal and lack of consistency. These limitations necessitate use of chemical plaque control agents as an adjunct to mechanical plaque control. Among various chemical agents, chlorhexidine (CHX) is considered to be a gold standard chemical agent for plaque control. Its structural formula consists of two symmetric 4-chlorophenyl rings and two biguanide groups connected by a central hexamethylene chain. Mechanism of action for CHX CHX is bactericidal and is effective against gram-positive bacteria, gram-negative bacteria and yeast organisms. -
Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Cytokines and Their Genetic Polymorphisms Related to Periodontal Disease
Journal of Clinical Medicine Review Cytokines and Their Genetic Polymorphisms Related to Periodontal Disease Małgorzata Kozak 1, Ewa Dabrowska-Zamojcin 2, Małgorzata Mazurek-Mochol 3 and Andrzej Pawlik 4,* 1 Chair and Department of Dental Prosthetics, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 2 Department of Pharmacology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 3 Department of Periodontology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland; [email protected] 4 Department of Physiology, Pomeranian Medical University, Powsta´nców Wlkp 72, 70-111 Szczecin, Poland * Correspondence: [email protected] Received: 24 October 2020; Accepted: 10 December 2020; Published: 14 December 2020 Abstract: Periodontal disease (PD) is a chronic inflammatory disease caused by the accumulation of bacterial plaque biofilm on the teeth and the host immune responses. PD pathogenesis is complex and includes genetic, environmental, and autoimmune factors. Numerous studies have suggested that the connection of genetic and environmental factors induces the disease process leading to a response by both T cells and B cells and the increased synthesis of pro-inflammatory mediators such as cytokines. Many studies have shown that pro-inflammatory cytokines play a significant role in the pathogenesis of PD. The studies have also indicated that single nucleotide polymorphisms (SNPs) in cytokine genes may be associated with risk and severity of PD. In this narrative review, we discuss the role of selected cytokines and their gene polymorphisms in the pathogenesis of periodontal disease. Keywords: periodontal disease; cytokines; polymorphism 1. -

Vhi Dental Rules - Terms and Conditions
Vhi Dental Rules - Terms and Conditions Date of Issue: 1st January 2021 Introduction to Your Policy The purpose of this Policy is to provide an Insured Person with Dental Services as described below. Only the stated Treatments are covered. Maximum benefit limits and any applicable waiting periods are listed in Your Table of Benefits. In order to qualify for cover under this Policy all Treatments must be undertaken by a Dentist or a Dental Hygienist in a dental surgery, be clinically necessary, in line with usual, reasonable and customary charges for the area where the Treatment was undertaken, and must be received by the Insured Person during their Period of Cover. Definitions We have defined below words or phrases used throughout this Policy. To avoid repeating these definitions please note that where these words or phrases appear they have the precise meaning described below unless otherwise stated. Where words or phrases are not listed within this section, they will take on their usual meaning within the English language. Accident An unforeseen injury caused by direct impact outside of oral cavity to an Insured Person’s teeth and gums (this includes damage to dentures whilst being worn). Cancer A malignant tumour, tissues or cells, characterised by the uncontrolled growth and spread of malignant cells and invasion of tissue. Child/Children Your children, step-child/children, legally adopted child/children or child/children where you are their legal guardian provided that the child/children is under age 18 on the date they are first included under this Policy. Claims Administrator Vhi Dental Claims Department, Intana, IDA Business Park, Athlumney, Navan, Co. -

Periodontitis and Peri-Implantitis Biomarkers in Human Oral Fluids and the Null-Allele Mouse Model
Department of Cell Biology of Oral Diseases Institute of Dentistry, Biomedicum Helsinki, University of Helsinki, Helsinki, Finland Department of Oral and Maxillofacial Diseases Helsinki University Central Hospital (HUCH), University of Helsinki, Helsinki, Finland Department of Diagnostics and Oral Medicine Institute of Dentistry, University of Oulu, Oulu University Hospital, Oulu, Finland PERIODONTITIS AND PERI-IMPLANTITIS BIOMARKERS IN HUMAN ORAL FLUIDS AND THE NULL-ALLELE MOUSE MODEL Heidi Kuula Academic Dissertation To be presented with the permission of the Faculty of Medicine, University of Helsinki, for public discussion in the Lecture Hall 1 at Biomedicum Helsinki, Haartmaninkatu 8, Helsinki, on June 12th 2009, at 12 noon Helsinki 2009 Supervised by: Professor Timo Sorsa, DDS, PhD, Dipl Perio Department of Cell Biology of Oral Diseases, Institute of Dentistry, University of Helsinki, and Department of Oral and Maxillofacial Diseases, Helsinki University Central Hospital (HUCH) Helsinki, Finland Professor Tuula Salo, DDS, PhD Department of Diagnostics and Oral Medicine, Institute of Dentistry, University of Oulu, and Oulu University Hospital (OYS) Oulu, Finland Reviewed by: Assistant Professor Marja L. Laine, DDS, PhD Department of Oral Microbiology, Academic Centre for Dentistry Amsterdam Amsterdam, the Netherlands Professor Denis F. Kinane, BDS, PhD Associate Dean for Research and Enterprise Delta Endowed Professor Director, Oral Health and Systemic Disease Research Group University of Louisville Louisville, Kentucky, USA Opponent: Professor Anders Gustafsson, DDS, PhD Institute of Odontology Department of Periodontology Karolinska Institutet Huddinge, Sweden ISBN 978-952-92-5634-1 (paperback) ISBN 978-952-10-5603-1 (PDF) Helsinki 2009 Yliopistopaino 2 CONTENTS List of original publications Abbreviations Abstract 1. Introduction 2. -

Surgical Crown Lengthening in a Population with Human Immunodeficiency Virus: a Retrospective Analysis<Link Href="#Jper0
Volume 83 • Number 3 Case Series Surgical Crown Lengthening in a Population With Human Immunodeficiency Virus: A Retrospective Analysis Shilpa Kolhatkar,* Suzanne A. Mason,† Ana Janic,* Monish Bhola,* Shaziya Haque,‡ and James R. Winkler* Background: Individuals with human immunodeficiency virus (HIV) have an increased risk of developing health problems, including some that are life threatening. Today, dental treatment for the population with a positive HIV diagnosis (HIV+) is comprehensive. There are limited reports on the outcomes of intraoral sur- gical therapy in patients with HIV, such as crown lengthening surgery (CLS) with osseous recontouring. This report investigates the outcome of CLS procedures performed at an urban dental school in a population of individuals with HIV. Specifically, this retrospective clinical analysis evaluates the healing response after CLS. Methods: Paper and electronic records were examined from the year 2000 to the present. Twenty-one in- dividuals with HIV and immunosuppression, ranging from insignificant to severe, underwent CLS. Pertinent details, including laboratory values, medications, smoking history/status, and postoperative outcomes, were recorded. One such surgery is described in detail with radiographs, photographs, and a videoclip. Results: Of the 21 patients with HIV examined after CLS, none had postoperative complications, such as delayed healing, infection, or prolonged bleeding. Variations in viral load (<48 to 40,000 copies/mL), CD4 cell count (126 to 1,260 cells/mm3), smoking (6 of 21 patients), platelets (130,000 to 369,000 cells/mm3), and neutrophils (1.1 to 4.5 · 103 /mm3) did not impact surgical healing. In addition, variations in medication reg- imens (highly active anti-retroviral therapy [18]; on protease inhibitors [1]; no medications [2]) did not have an impact. -

Classification and Diagnosis of Aggressive Periodontitis
Received: 3 November 2016 Revised: 11 October 2017 Accepted: 21 October 2017 DOI: 10.1002/JPER.16-0712 2017 WORLD WORKSHOP Classification and diagnosis of aggressive periodontitis Daniel H. Fine1 Amey G. Patil1 Bruno G. Loos2 1 Department of Oral Biology, Rutgers School Abstract of Dental Medicine, Rutgers University - Newark, NJ, USA Objective: Since the initial description of aggressive periodontitis (AgP) in the early 2Department of Periodontology, Academic 1900s, classification of this disease has been in flux. The goal of this manuscript is to Center of Dentistry Amsterdam (ACTA), review the existing literature and to revisit definitions and diagnostic criteria for AgP. University of Amsterdam and Vrije Universiteit, Amsterdam, The Netherlands Study analysis: An extensive literature search was performed that included databases Correspondence from PubMed, Medline, Cochrane, Scopus and Web of Science. Of 4930 articles Dr. Daniel H. Fine, Department of Oral reviewed, 4737 were eliminated. Criteria for elimination included; age > 30 years old, Biology, Rutgers School of Dental Medicine, Rutgers University - Newark, NJ. abstracts, review articles, absence of controls, fewer than; a) 200 subjects for genetic Email: fi[email protected] studies, and b) 20 subjects for other studies. Studies satisfying the entrance criteria The proceedings of the workshop were were included in tables developed for AgP (localized and generalized), in areas related jointly and simultaneously published in the Journal of Periodontology and Journal of to epidemiology, microbial, host and genetic analyses. The highest rank was given to Clinical Periodontology. studies that were; a) case controlled or cohort, b) assessed at more than one time-point, c) assessed for more than one factor (microbial or host), and at multiple sites. -

Application of Vibroacoustic Diagnosis in Assessing Bridges Connecting Teeth and Implants to Treat Tooth Absence in Sea Vessel Crews
POLISH MARITIME RESEARCH 1 (105) 2020 Vol. 27; pp. 188-194 10.2478/pomr-2020-0020 APPLICATION OF VIBROACOUSTIC DIAGNOSIS IN ASSESSING BRIDGES CONNECTING TEETH AND IMPLANTS TO TREAT TOOTH ABSENCE IN SEA VESSEL CREWS Artur Rasinski Military Institute of Medicine, Clinics of Otorhinolaryngology and Laryngological Oncology with the Clinical Ward of Oral and Maxillo-facial Surgery , Poland Grzegorz Klekot Warsaw University of Technology, Faculty of Automotive and Construction Machinery Engineering, Poland Piotr Skopiński Department of Histology and Embryology, Centre for Biostructure Research, Medical University of Warsaw, Poland ABSTRACT Implant treatment is a proven method in dentistry for partial and complete missing teeth reconstruction. In some clinical situations it is advisable to limit the number of implants, which can be obtained by making a bridge connecting the patient’s own tooth with the implant. So far, the possibility of using safe and permanent connections of natural teeth with implants has been examined to a small extent due to the dangers resulting from the different mobility of dental implants and teeth. An attempt was made to use vibro-acoustic techniques to evaluate various combinations of teeth and implants. Pilot studies were carried out on cadavers-pig mandibles with implants. There were recorded sounds in the immediate vicinity of the mandible formed in response to impulse excitations carried out with a point hit against a tooth or implant before and after their joining with a bridge. The comparison of spectra allows to see features indicating a high probability of being able to distinguish between the examined configurations. The results of the research should contribute to a better understanding of the mutual relations between the dental implant and the tooth, which are included in bridge. -
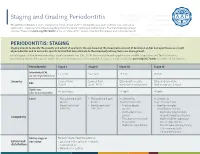
Staging and Grading Periodontitis
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

The Roots of Periodontology
THE ROOTS OF PERIODONTOLOGY NMDHA 24th Annual Scientific Session Dennis Miller DMD, MS Diplomate, American Board of Periodontology Oct 19, 2012 A word about the value of history…… Those who don’t know history are destined to repeat it. Edmond Burke (1729-1797) Those of you who don’t remember the past are condemned to repeat it. • George Santayama, 1890 The History of Dentistry • Barbers and blacksmiths were the first dentists in America • 1840 – opening of the first dental school, University of Baltimore • 1859 – ADA was founded, oldest and largest national Dental Society in the world • 1890 – Dr. John Riggs describes periodontal disease • Calls it Riggs disease or pyorrhea • Marketed Anti-Riggs mouthwash (156 proof) • 1896 – Dr. G.V. Black who is known as the father of modern dentistry, describes cavity preparations • 1906 – Dr. C. Edmund Kells exposes first dental radiograph; also the first to use female dental assistants and surgical aspirators • 1929 – Orthodontics recognized as first dental specialty History of Periodontics • 1914 – Dr. Grace Rodgers Spalding and Dr. Gillette Hayden (both physicians) formed the American Academy of Oral Prophylaxis and Periodontology • 1919 – became the American Academy of Periodontology • Circa 1941 - Periodontics recognized as a dental specialty History of Hygiene • 1867 – Lucy Hobbs Taylor graduated from Ohio College of Dental Surgery as a hygienist • 1884 – paper presented at the NY 1st District Dental Society meeting advocating teeth cleaning for prevention, done by “staff” • 1923 – formation of ADHA Historical names of periodontitis • Loculosis • Blennorrhea gingivae • Periostitis • Alveolodental periostitis • Infectious arthrodental gingivitis • Phagedenic pericementitis • Expulsive gingivitis • Symptomatic alveolar arthritis • Smutz pyorrhea • Riggs disease • Periodontoclasia • Pyorrhea alveolaris The roots of Periodontology • The roots of the dental profession including periodontics and dental hygiene were not concocted by some entrepreneur. -

A Better View of Implants
dentistry uncensored highlights partner content A Better View of Implants Dr. Howard Farran and Dr. Ernest Orphanos discuss periodontics, implants and the importance of magnification at work r. Ernest Orphanos began Ernest Orphanos: It’s inaccurate. other dynamic with respect to what practicing as a periodontist in There is a plethora of reasons why we can do to save teeth. But we also D1994 in Florida, where today he but, by virtue of understanding have to be aware of the longitudinal focuses his services on dental implants the literature, we know that the studies. We can’t base the treatment and procedures related to dental longitudinal studies of All-on-4— we provide on our feelings or our implants, including All-on-4. compared to All-on-6, immediate-load opinions. It really should be based on Orphanos, who is the visiting and delayed-loading—have the same the peer-reviewed literature. lecturer for the postgraduate 10-year success rate. HF: How can new dentists department of periodontics at Tufts That’s No. 1. No. 2 is, if you do have determine whether they should use University, lectures nationally and a failed implant, you can replace the old-school periodontal surgery or internationally on this procedure, implant and weld to the titanium bar titanium? which allows four implants, as well as within the prosthesis. No. 3 is because EO: One has to defer to experts to teeth, to be placed on the same day. you’re reducing the bone, and you’re really make the best clinical judgment He teaches other surgeons All-on-4 at reducing this alveolar ridge, you’re for the patient, but a variety of factors his educational center in Boca Raton, getting down into the better basal come into play. -

Tobacco and Your Oral Health
Oral Wellness Series Tobacco and Your Oral Health We all know smoking is bad for us, but did you know that chewing tobacco is just as harmful to your oral health as cigarettes? Tobacco causes bad breath, which nobody likes, but it has far more serious risks to your oral health, including: • Mouth sores • Slow healing after oral surgery • Difficulties correcting cosmetic dental problems • Stained teeth and tongue • Dulled sense of taste and smell The Biggest Risk? Did you know tobacco Cancer. The Centers for Disease Control have linked smoking and use is a huge risk factor tobacco use to oral cancer. Oral cancer is the eighth most common cancer in the U.S., and it’s very difficult to detect. As a result, two- for gum disease? thirds of all cases are diagnosed in late stages, making treatment and survival difficult.1 Tobacco and Gum Disease Tobacco use is also a huge risk factor for gum disease, a leading cause of tooth loss. More than 41% of daily smokers over the age of 65 are toothless because of gum disease, compared to only 20% of non-smokers.2 Maintain good oral health by avoiding tobacco. It keeps your whole body healthier. The Effects of Smoking on Your Gums Smoking reduces blood flow to your gums, cutting Is Smokeless Tobacco Safer? off vital nutrients and preventing bones from healing. Smokeless tobacco—chew, dip and snuff—is not This lets bacteria from tartar infect surrounding tissue, regulated by the FDA so it’s hard to know what’s in it. 3 forming deep pockets between teeth and gums.