Comparative Evaluation of Two Different One-Stage Full-Mouth
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Chlorhexidine in Maintaining Periodontal Health
International Journal of Dentistry Research 2016; 1(1): 31-33 Review Article Importance of Chlorhexidine in Maintaining Periodontal IJDR 2016; 1(1): 31-33 December Health © 2016, All rights reserved www.dentistryscience.com Dr. Manpreet Kaur*1, Dr. Krishan Kumar1 1 Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak-124001, Haryana, India Abstract Plaque is responsible for periodontal diseases. In order to prevent occurrence and progression of periodontal disease, removal of plaque becomes important. Mechanical tooth cleaning aids such as toothbrushes, dental floss, interdental brushes are used for removal of plaque. However, in some cases, chemical agents are used as an adjunct to mechanical methods to facilitate plaque control and prevent gingivitis. Chlorhexidine (CHX) mouthwash is the most commonly used and is considered as gold standard chemical agent. In this review, mechanism of action and other properties of CHX are discussed. Keywords: Plaque, Chemical agents, Chlorhexidine (CHX). INTRODUCTION Dental plaque is primary etiologic factor responsible for gingivitis and periodontitis [1]. Mechanical plaque control using toothbrushes, interdental brushes, dental floss prevent occurrence of gingivitis. However, in majority of population, mechanical methods of plaque control are ineffective due to less time spent[2] for plaque removal and lack of consistency. These limitations necessitate use of chemical plaque control agents as an adjunct to mechanical plaque control. Among various chemical agents, chlorhexidine (CHX) is considered to be a gold standard chemical agent for plaque control. Its structural formula consists of two symmetric 4-chlorophenyl rings and two biguanide groups connected by a central hexamethylene chain. Mechanism of action for CHX CHX is bactericidal and is effective against gram-positive bacteria, gram-negative bacteria and yeast organisms. -

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Periodontal Practice Patterns
PERIODONTAL PRACTICE PATTERNS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of the Ohio State University By Janel Kimberlay Yu, D.D.S. Graduate Program in Dentistry The Ohio State University 2010 Dissertation Committee: Dr. Angelo Mariotti, Advisor Dr. Jed Jacobson Dr. Eric Seiber Copyright by Janel Kimberlay Yu 2010 Abstract Background: Differences in the rates of dental services between geographic regions are important since major discrepancies in practice patterns may suggest an absence of evidence-based clinical information leading to numerous treatment plans for similar dental problems and the misallocation of limited resources. Variations in dental care to patients may result from characteristics of the periodontist. Insurance claims data in this study were compared to the characteristics of periodontal providers to determine if variations in practice patterns exist. Methods: Claims data, between 2000-2009 from Delta Dental of Ohio, Michigan, Indiana, New Mexico, and Tennessee, were examined to analyze the practice patterns of 351 periodontists. For each provider, the average number of select CDT periodontal codes (4000-4999), implants (6010), and extractions (7140) were calculated over two time periods in relation to provider variable, including state, urban versus rural area, gender, experience, location of training, and membership in organized dentistry. Descriptive statistics were performed to depict the data using measures of central tendency and measures of dispersion. ii Results: Differences in periodontal procedures were present across states. Although the most common surgical procedure in the study period was osseous surgery, greater increases over time were observed in regenerative procedures (bone grafts, biologics, GTR) when compared to osseous surgery. -

Instant Update- Getting up to Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 F
Instant Update- Getting Up To Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 Francis G. Serio, DMD, MS, MBA Diplomate, American Board of Periodontology Staff Dentist, Greene County Health Care, Inc. Course Synopsis Some things change and some things remain the same. The bedrocks of periodontal therapy are time-tested but new approaches to some of these therapies are providing better outcomes for patients. In addition, advances in the science of periodontics have led to both a better understanding of the disease processes and a new classification system for the periodontal diseases and conditions. In addition, as implant dentistry continues to solidify its position, complications are becoming more commonplace. This course will focus on four main areas: The changes in science that have led to the new classification of the periodontal diseases and conditions. Current understanding of the perio-systemic connection. The “semi-surgical” approach to periodontal therapy. Peri-implant mucositis and peri-implantitis and what to do about it. At the end of this presentation, each participant will be able to: Identify the differences between the 1999 and 2017 disease classification systems. Identify key factors and systemic diseases that have a strong association with the periodontal diseases. Develop a “semi-surgical” treatment plan for a patient with periodontitis. Understand the key factors that contribute to peri-implant disease and possible therapeutic approaches. Periodontitis is a disease of the non-mineralized and mineralized connective tissues- What causes and contributes to its breakdown? Bacterial infections vs. Inflammation 1 Statistical vs. Clinical Significance Clinical significance- Jacobson, et al. -

Phenytoin-Induced Gingival Overgrowth Management
Brazilian Dental Journal (2015) 26(1): 39-43 ISSN 0103-6440 http://dx.doi.org/10.1590/0103-6440201300029 Department of Dentistry, UFRN - Phenytoin-Induced Gingival Federal University of Rio Grande Overgrowth Management do Norte, Natal, RN, Brazil Correspondence: Dr. Bruno César with Periodontal Treatment de Vasconcelos Gurgel, Avenida Senador Salgado Filho, 1787, Lagoa Nova, 59056-000 Natal, RN, Brasil. Tel.: +55-84-3215-4103. e-mail: [email protected] Bruno César de Vasconcelos Gurgel, Carlos Roberto Batista de Morais, Pedro Carlos da Rocha-Neto, Euler Maciel Dantas, Leão Pereira Pinto, Antonio de Lisboa Lopes Costa Phenytoin-induced gingival overgrowth (PIGO) is a common complication of the continuous use of medications. This paper presents a case of PIGO hindering oral function and compromising oral hygiene and aesthetics, which was treated with a combination of nonsurgical and surgical periodontal therapies. A 39-year-old male patient was referred for dental treatment with several complaints, especially upper and lower gingival overgrowth that hindered speech and swallowing. Generalized deep probing pockets and bone loss were detected. Diagnosis of gingival overgrowth associated with phenytoin and chronic periodontitis was established. The treatment plan consisted of conservative therapy with education on oral health, motivation and meticulous oral hygiene instruction in combination with scaling and root planing. During the revaluation period, a marked reduction in the clinical parameters was noted, particularly probing pocket depth reduction. Surgical therapy for removal of gingival overgrowth was also performed to achieve pocket reduction. Supportive periodontal therapy was proposed Key words: phenytoin, gingival and the patient is currently under follow-up for 4 years. -

Classification and Diagnosis of Aggressive Periodontitis
Received: 3 November 2016 Revised: 11 October 2017 Accepted: 21 October 2017 DOI: 10.1002/JPER.16-0712 2017 WORLD WORKSHOP Classification and diagnosis of aggressive periodontitis Daniel H. Fine1 Amey G. Patil1 Bruno G. Loos2 1 Department of Oral Biology, Rutgers School Abstract of Dental Medicine, Rutgers University - Newark, NJ, USA Objective: Since the initial description of aggressive periodontitis (AgP) in the early 2Department of Periodontology, Academic 1900s, classification of this disease has been in flux. The goal of this manuscript is to Center of Dentistry Amsterdam (ACTA), review the existing literature and to revisit definitions and diagnostic criteria for AgP. University of Amsterdam and Vrije Universiteit, Amsterdam, The Netherlands Study analysis: An extensive literature search was performed that included databases Correspondence from PubMed, Medline, Cochrane, Scopus and Web of Science. Of 4930 articles Dr. Daniel H. Fine, Department of Oral reviewed, 4737 were eliminated. Criteria for elimination included; age > 30 years old, Biology, Rutgers School of Dental Medicine, Rutgers University - Newark, NJ. abstracts, review articles, absence of controls, fewer than; a) 200 subjects for genetic Email: fi[email protected] studies, and b) 20 subjects for other studies. Studies satisfying the entrance criteria The proceedings of the workshop were were included in tables developed for AgP (localized and generalized), in areas related jointly and simultaneously published in the Journal of Periodontology and Journal of to epidemiology, microbial, host and genetic analyses. The highest rank was given to Clinical Periodontology. studies that were; a) case controlled or cohort, b) assessed at more than one time-point, c) assessed for more than one factor (microbial or host), and at multiple sites. -

Deep Cleaning (Scaling and Root Planing) Home Care Instructions
Deep Cleaning (Scaling and Root Planing) Home Care Instructions Following the completion of your deep cleaning appointment please follow these home care instructions : - Days 1-3: Warm saltwater rinses 2-3 times daily. A soft food diet is recommended in these initial few days. Days 4-14: Rinse with 1 cap full of Chlorhexidine twice daily after brushing and flossing. Please refrain from eating or drinking for 30 minutes after. Resume twice daily brushing and flossing. Consistent daily oral hygiene is essential to allow proper healing of your gum tissues. - In some cases, local antibiotics may have been placed. If so, please follow the specific instructions that were given to you at your appointment. Others points to Consider: The local anesthesia administered will likely cause your lips, tongue, and cheeks to remain numb for several hours. During this time, please be very careful to not chew, burn, or otherwise injure your lips, tongue, or cheeks. If you must eat while still numb, it is advisable to do so on the opposite side. It is normal to have some mild discomfort after your cleaning. The discomfort is from cleaning plaque and calculus off of the teeth around already inflamed tissue. The multiple injections also will contribute towards your soreness. Motrin may be taken for pain relief, but do not exceed 800mg in 8 hours. After scaling and root planing, you can expect that your gum tissue will be less swollen or prone to bleeding. You may also notice that your teeth feel smoother and your breath smells better. You may experience some thermal sensitivity (especially cold) after your cleaning. -
Staging and Grading Periodontitis
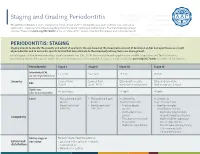
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

The Roots of Periodontology
THE ROOTS OF PERIODONTOLOGY NMDHA 24th Annual Scientific Session Dennis Miller DMD, MS Diplomate, American Board of Periodontology Oct 19, 2012 A word about the value of history…… Those who don’t know history are destined to repeat it. Edmond Burke (1729-1797) Those of you who don’t remember the past are condemned to repeat it. • George Santayama, 1890 The History of Dentistry • Barbers and blacksmiths were the first dentists in America • 1840 – opening of the first dental school, University of Baltimore • 1859 – ADA was founded, oldest and largest national Dental Society in the world • 1890 – Dr. John Riggs describes periodontal disease • Calls it Riggs disease or pyorrhea • Marketed Anti-Riggs mouthwash (156 proof) • 1896 – Dr. G.V. Black who is known as the father of modern dentistry, describes cavity preparations • 1906 – Dr. C. Edmund Kells exposes first dental radiograph; also the first to use female dental assistants and surgical aspirators • 1929 – Orthodontics recognized as first dental specialty History of Periodontics • 1914 – Dr. Grace Rodgers Spalding and Dr. Gillette Hayden (both physicians) formed the American Academy of Oral Prophylaxis and Periodontology • 1919 – became the American Academy of Periodontology • Circa 1941 - Periodontics recognized as a dental specialty History of Hygiene • 1867 – Lucy Hobbs Taylor graduated from Ohio College of Dental Surgery as a hygienist • 1884 – paper presented at the NY 1st District Dental Society meeting advocating teeth cleaning for prevention, done by “staff” • 1923 – formation of ADHA Historical names of periodontitis • Loculosis • Blennorrhea gingivae • Periostitis • Alveolodental periostitis • Infectious arthrodental gingivitis • Phagedenic pericementitis • Expulsive gingivitis • Symptomatic alveolar arthritis • Smutz pyorrhea • Riggs disease • Periodontoclasia • Pyorrhea alveolaris The roots of Periodontology • The roots of the dental profession including periodontics and dental hygiene were not concocted by some entrepreneur. -

Retrospective Analysis of the Risk Factors of Peri-Implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5
ORIGINAL RESEARCH Retrospective Analysis of the Risk Factors of Peri-implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5 ABSTRACT Aim and objective: Peri-implantitis is a key concern for dental implants and the main common reason for implant failure. This investigation evaluated the risk factors and their implications on peri-implantitis. Materials and methods: A retrospective search of the patients’ clinical notes was performed to identify the documented cases of peri-implantitis. The inclusion criteria encompassed patients who were 18 years and older and were seen at the School of Dental Medicine, University of Nevada, Las Vegas, from January 2014 through September 2018. The search revealed that the number of peri-implantitis cases was 28, with an overall 45 implants. Data were collected and analyzed using the Chi-square test. Results: Total 28 patients presented with peri-implantitis. The distribution of males to females with peri-implantitis was 60.7 and 39.3%, respectively. The highest number of patients (21.4%) presenting with peri-implantitis fell within the age range of 65–69 years; 53.3% of peri- implantitis cases were in the maxillary arch. The predilection area for peri-implantitis was the mandibular first molar (24.4%). Periodontitis was the most significant cause (60.7%); respiratory diseases (42.9%) followed by hypertension (28.6%) were the most prevalent medical conditions in the studied population. Peri-implantitis occurred most frequently among Caucasians (62.7%), followed by Hispanics (29%). Conclusion: Within the limitations of the current evaluation, findings support previous claims that periodontitis remains the strongest predictor of peri-implantitis. -

Controlling the Intraoral Environment Before and After Implant Therapy a Peer-Reviewed Publication Written by Richard Nejat, DDS; Daniel Nejat, DDS; and Fiona M
Earn 4 CE credits This course was written for dentists, dental hygienists, and assistants. Controlling the Intraoral Environment Before and After Implant Therapy A Peer-Reviewed Publication Written by Richard Nejat, DDS; Daniel Nejat, DDS; and Fiona M. Collins, BDS, MBA, MA PennWell is an ADA CERP Recognized Provider Go Green, Go Online to take your course This course has been made possible through an unrestricted educational grant. The cost of this CE course is $59.00 for 4 CE credits. Cancellation/Refund Policy: Any participant who is not 100% satisfied with this course can request a full refund by contacting PennWell in writing. Educational Objectives smoking and drinking. The association between systemic Upon completion of this course, the clinician will be able to disease and periodontal health is well established, and the do the following: relationship between periodontal health and peri-implant 1. Understand the process of patient selection and the health is well established. For short- and long-term success systemic considerations that affect candidacy for of implants, patients must be willing and able to perform implant treatment effective oral hygiene measures to control the intraoral 2. List the adverse implant outcomes due to biological/ microbial environment. microbiological factors and mechanical factors 3. Control the intraoral environment during all three Patient Selection phases of implant treatment—presurgical, postsurgical, Patient selection during implant treatment planning involves and maintenance many considerations. In addition to the intraoral environ- 4. Understand the precautions to be taken when using ment, the patient’s general health status and smoking habits instruments around implants and the potential damage are highly relevant.