Deep Cleaning (Scaling and Root Planing) Home Care Instructions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Instant Update- Getting up to Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 F
Instant Update- Getting Up To Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 Francis G. Serio, DMD, MS, MBA Diplomate, American Board of Periodontology Staff Dentist, Greene County Health Care, Inc. Course Synopsis Some things change and some things remain the same. The bedrocks of periodontal therapy are time-tested but new approaches to some of these therapies are providing better outcomes for patients. In addition, advances in the science of periodontics have led to both a better understanding of the disease processes and a new classification system for the periodontal diseases and conditions. In addition, as implant dentistry continues to solidify its position, complications are becoming more commonplace. This course will focus on four main areas: The changes in science that have led to the new classification of the periodontal diseases and conditions. Current understanding of the perio-systemic connection. The “semi-surgical” approach to periodontal therapy. Peri-implant mucositis and peri-implantitis and what to do about it. At the end of this presentation, each participant will be able to: Identify the differences between the 1999 and 2017 disease classification systems. Identify key factors and systemic diseases that have a strong association with the periodontal diseases. Develop a “semi-surgical” treatment plan for a patient with periodontitis. Understand the key factors that contribute to peri-implant disease and possible therapeutic approaches. Periodontitis is a disease of the non-mineralized and mineralized connective tissues- What causes and contributes to its breakdown? Bacterial infections vs. Inflammation 1 Statistical vs. Clinical Significance Clinical significance- Jacobson, et al. -
04-301E Scaling and Root Planing
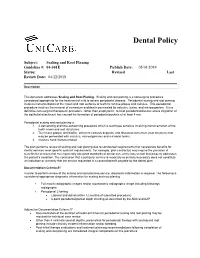
Dental Policy Subject: Scaling and Root Planing Guideline #: 04-301E Publish Date: 05/01/2019 Status: Revised Last Review Date: 04/22/2019 Description This document addresses Scaling and Root Planing. Scaling and root planing is a nonsurgical procedure considered appropriate for the treatment of mild to severe periodontal disease. Periodontal scaling and root planing involves instrumentation of the crown and root surfaces of teeth to remove plaque and calculus. This periodontal procedure involves the removal of cementum and dentin permeated by calculus, toxins, and microorganism. It is a definitive non-surgical therapeutic procedure, rather than prophylactic, to treat periodontal disease where migration of the epithelial attachment has caused the formation of periodontal pockets of at least 4 mm. Periodontal scaling and root planing is: 1. A demanding and time-consuming procedure which is technique sensitive involving instrumentation of the tooth crown and root structures. 2. To remove plaque and biofilm, adherent calculus deposits, and diseased cementum (root structure) that may be permeated with calculus, microorganisms and microbial toxins. 3. involves hand instrumentation The plan performs review of scaling and root planing due to contractual requirements that necessitate benefits for dental services meet specific contract requirements. For example, plan contract(s) may require the provision of benefits for services that meet generally accepted standards of dental care at the lowest cost that properly addresses the patient’s condition. The conclusion that a particular service is medically or dentally necessary does not constitute an indication or warranty that the service requested is a covered benefit payable by the dental plan. Documentation Criteria #1 In order to perform review of the scaling and root planning service, diagnostic information is required. -

Comparative Evaluation of Two Different One-Stage Full-Mouth
ORIGINAL RESEARCH Comparative Evaluation of Two Different One-stage Full-mouth Disinfection Protocols using BANA Assay: A Randomized Clinical Study Arjumand Farooqui1, Vineet V Kini2, Ashvini M Padhye3 ABSTRACT Aim: The aim of this study was to evaluate and compare two different one-stage full-mouth disinfection protocols in the treatment of chronic periodontitis by assessing dental plaque and tongue coat using BANA assay. Materials and methods: The present study was a prospective randomized clinical parallel arm study design including 40 healthy subjects randomly allocated into two groups, i.e., group A (Quirynen’s protocol of one-stage full-mouth disinfection) and group B (Bollen’s protocol of one-stage full-mouth disinfection). Subjects were assessed at baseline and six weeks using plaque index, gingival index, and sulcus bleeding index. Probing depth and relative clinical attachment level were also recorded at six weeks. Winkel tongue coat index and BANA were recorded at 8 weeks using subgingival plaque and tongue coat sample. Results: Both group A and group B demonstrated statistically significant reduction in plaque index, gingival index, sulcus bleeding index, Winkel tongue coat index, reduction in probing depth, and gain in relative clinical attachment level on intragroup comparison. There was no significant difference in BANA assay score of subgingival plaque and tongue coat samples in between group A and group B. Conclusion: From the findings of this study, both Quirynen’s protocol and Bollen’s protocol of one-stage full-mouth disinfection are effective in plaque reduction and tongue coat reduction and achieve comparable clinical healing outcomes. Clinical significance: The difference in duration and mode of use of chlorhexidine as a chemical plaque control agent in the two treatment interventions of Quirynen’s and Bollen’s protocol of one-stage full-mouth disinfection did not demonstrate statistical significance in reducing sulcus bleeding index scores, reducing probing depths, and gain in relative clinical attachment levels. -

The Treatment of Peri-Implant Diseases: a New Approach Using HYBENX® As a Decontaminant for Implant Surface and Oral Tissues
antibiotics Article The Treatment of Peri-Implant Diseases: A New Approach Using HYBENX® as a Decontaminant for Implant Surface and Oral Tissues Michele Antonio Lopez 1,†, Pier Carmine Passarelli 2,†, Emmanuele Godino 2, Nicolò Lombardo 2 , Francesca Romana Altamura 3, Alessandro Speranza 2 , Andrea Lopez 4, Piero Papi 3,* , Giorgio Pompa 3 and Antonio D’Addona 2 1 Unit of Otolaryngology, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] 2 Division of Oral Surgery and Implantology, Institute of Clinical Dentistry, Department of Head and Neck, Catholic University of the Sacred Heart, Gemelli University Polyclinic Foundation, 00168 Rome, Italy; [email protected] (P.C.P.); [email protected] (E.G.); [email protected] (N.L.); [email protected] (A.S.); [email protected] (A.D.) 3 Department of Oral and Maxillo Facial Sciences, Policlinico Umberto I, “Sapienza” University of Rome, 00161 Rome, Italy; [email protected] (F.R.A.); [email protected] (G.P.) 4 Universidad Europea de Madrid, 28670 Madrid, Spain; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Background: Peri-implantitis is a pathological condition characterized by an inflammatory Citation: Lopez, M.A.; Passarelli, process involving soft and hard tissues surrounding dental implants. The management of peri- P.C.; Godino, E.; Lombardo, N.; implant disease has several protocols, among which is the chemical method HYBENX®. The aim Altamura, F.R.; Speranza, A.; Lopez, of this study is to demonstrate the efficacy of HYBENX® in the treatment of peri-implantitis and to A.; Papi, P.; Pompa, G.; D’Addona, A. -

One-Stage, Full-Mouth Disinfection: Fiction Or Reality?
FOCUS ARTICLE One-Stage, Full-Mouth Disinfection: Fiction or Reality? Marc Quirynen, Wim Teughels, Martine Pauwels, Daniel van Steenberghe Recent research indicated that periopathogens colonize, besides the pockets, also other niches within the oral cavity including: the soft tissues, the saliva, the tongue, and even the tonsils. Since the supragingival plaque and the bacteria in these niches have a major impact on the subgin- gival plaque colonisation but especially on the recolonation after debridement, it seems reason- able to expect that a one-stage, full-mouth disinfection protocol, involving the bacteria over the entire oro-pharyngeal area, has a significantly better outcome when compared to a more staged approach (e.g. with treatments per quadrant). Since several review papers recently discussed the benefits of a one-stage, full-mouth disinfection protocol, pointing to some shortcomings in the our research protocol or with an attempt to compare the data of the new approach with other studies (with unfortunately non comparable approaches), this review paper aims to clarify some of the confusion concerning the benefits of a one-stage, full-mouth disinfection approach. Key words: periodontal breakdown; periodontopathogens; mouth disinfection INTRODUCTION logy, 1996; Slots and Rams, 1991; Socransky and Haffajee, 1992; Wolff et al, 1994). The ef- Periodontal breakdown primarily develops when ficiency of the host defence is partially hereditary the microbial load within a periodontal pocket (Kinane and Hart, 2003) but environmental fac- overrules the local and systemic host defence tors such as bad oral hygiene, smoking, immuno- mechanisms. Such an imbalance occurs in differ- suppressive medication, stress and so on can fur- ent situations, including an aspecific increase in ther impair the immune defence mechanism. -

Lasers in Minimally Invasive Periodontal and Peri-Implant Therapy
Periodontology 2000, Vol. 71, 2016, 185–212 © 2016 John Wiley & Sons A/S. Published by John Wiley & Sons Ltd Printed in Singapore. All rights reserved PERIODONTOLOGY 2000 Lasers in minimally invasive periodontal and peri-implant therapy KOJI MIZ UTANI, AKI RA AOKI , DONALD COLUZZI, RAYMOND YUKNA , CHEN-YING WANG, VERI CA PAV LIC & YUICHI IZUMI ‘Pain free’ and ‘simple procedure’ are two of the most occasionally demonstrated some effectiveness. attractive phrases to patients who are otherwise Recent evidence demonstrates that laser treatment reluctant to accept any dental treatment (138). Mini- has the potential to improve therapeutic outcomes mally invasive dental therapy (81) could satisfy the and therefore be a valuable addition to conventional demands of such patients. The procedures can be treatments (55). Currently, high-power-output lasers comfortable, although not necessarily without any are used adjunctively with scaling and root planing or pain; and be effective for disease control whilst pre- as minimally invasive surgery. Also, very-low-power- serving more healthy dental tissue. output lasers are employed for cellular stimulation Scaling and root planing is an example of a mini- and/or activation of antimicrobial agents following mally invasive procedure because it is a conservative, scaling and root planing. Both of these laser applica- cause-related therapy that attempts to eliminate etio- tions can be considered as minimally invasive logic factors from the root surface (26). Scaling and approaches to periodontal disease treatment. root planing can result in improved clinical outcomes The aim of the present review was to survey the rele- such as reduced bleeding on probing and decreased vant literature of the clinical application of lasers as periodontal pocket depth. -

ADA Guide to Reporting D4346
D4346 Guide – Version 4 – July 11, 2018 – Page 1 of 11 ADA Code of Ethics: Veracity This is the foundation for the ADA’s position – “Code for what you do, and do what you coded for.” Section 5 of the ADA Principles of Ethics and Code of Professional Conduct is particularly applicable when determining the treatment plan and procedure coding. SECTION 5 — Principle: Veracity ("truthfulness") The dentist has a duty to communicate truthfully. Code of Professional Conduct 5.A. Representation of Care. Dentists shall not represent the care ADA Guide to being rendered to their patients in a false or misleading manner. Reporting D4346 5.B. Representation of Fees. Dentists shall not represent the fees being charged for providing care in a false or misleading Developed by the ADA, this guide is manner. published to educate dentists and Advisory Opinions others in the dental community on this scaling procedure and its 5.B.5. Dental Procedures. A dentist who incorrectly describes on a third approved code, first published in party claim form a dental procedure in order to receive a greater CDT 2017 and effective Jan 1, 2017 payment or reimbursement or incorrectly makes a non-covered procedure appear to be a covered procedure on such a claim ©2018 American Dental Association (ADA). form is engaged in making an unethical, false or misleading All rights reserved. representation to such third party. 5.B.6. Unnecessary Services. A dentist who recommends and performs unnecessary dental services or procedures is engaged in unethical conduct. The dentist's ethical obligation in this matter applies regardless of the type of practice arrangement or contractual obligations in which he or she provides patient care. -

Evaluation of Clinical Efficacy of 0.2% Chlorhexidine Irrigation, 1.5
Original Research Article Evaluation of clinical efficacy of 0.2% chlorhexidine irrigation, 1.5% chlorhexidine gel and 2.5mg biodegradable chlorhexidine chip as an adjunct to scaling and root planing in the management of Chronic Periodontitis Shubhra Vaish1,*, Vidya Dodwad2, Aakriti Mahajan3, Sonakshi Gupta4 1Professor, 2Professor & Head, 3,4Senior Resident, Dept. of Periodontology & Oral Implantology, ITS Centre for Dental Studies & Research, Muradnagar, Ghaziabad, Uttar Pradesh, India *Corresponding Author: Email: [email protected] Abstract Introduction: Various chemotherapeutic agents can be administered subgingivally to enhance the efficacy of non-surgical therapy mechanical treatment. Chlorhexidine (CHX) is an effective antimicrobial agent and has been used as a topical antiseptic for over 30 years. The aim of the study was to evaluate and compare the clinical efficacy of various forms of local delivery of Chlorhexidine (CHX) i.e. 0.2% CHX irrigation, 1.5% CHX gel and 2.5mg biodegradable CHX chip as an adjunct to scaling and root planning in the management of Chronic Periodontitis. Materials and Method: Forty sites from patients with Chronic Periodontitis and probing depth 5 to 7 mm were randomly divided into 4 groups. Group I (10 Sites): scaling and root planing (SRP) + subgingival irrigation with 0.2% Chlorhexidine; Group II (10 Sites): SRP + subgingival application of 1.5% Chlorhexidine gel (Chlo-Site); Group III (10 Sites): SRP + intrapocket administration of Chlorhexidine chip (Periocol-CG); Group IV (10 Sites): scaling and root planing only (control group). Improvement in periodontal health was assessed by the gingival index of Loe and Silness and plaque was assessed using the Turesky et al. -

Prenatal Dental Care Prescription
Prenatal Dental Care Prescription Patient Name: (Last) ______________ (First) _________________ DOB: Gestational Age today: __________ Due Date: ____________________ Allergies: ______________________________________________________ Medications: Precautions: NONE SPECIFY (If any): Please provide routine dental evaluation and care, which may include the following: ■ Dental x-ray with proper abdominal and neck lead shield (after 14 weeks gestation) ■ Oral Health Examination ■ Dental prophylaxis ■ Scaling and root planing ■ Root canal ■ Extraction ■ Restorations (amalgam or composite) filling cavities ■ Local anesthesia (without vasopressors, e.g. epinephrine) ■ Antibiotics (except Tetracycline/Sulfa/Quinolones) The use of the following are considered generally safe during pregnancy, if no drug allergy exists. Patient may have: (Check all that apply) Acetaminophen with codeine for pain control (Note: no NSAID’s, e.g., ibuprofen, naproxen) Alternative pain control medication: (Specify) ____________________________ Penicillin/Amoxicillin Clindamycin Cephalosporins Erythromycin (Not estolate form) Please note that routine cleaning and plaque control can performed in ANY trimester and that the preferred time to treat active caries is between 13 to 30 weeks of gestation. Prenatal Care Provider: _______________________________ Phone: __________________ Signature: __________________________________________ Date: ___________________ DO NOT HESITATE TO CALL FOR QUESTIONS ************************************************************************************* -

Post Op Scaling and Root Planing Instructions
POST OPERATIVE INSTRUCTIONS FOLLOWING SCALING AND ROOT PLANING PLEASE READ THESE INSTRUCTIONS COMPLETELY AND CAREFULLY Scaling and root planing is a non-surgical treatment of periodontal disease. The purpose of the treatment is to remove bacterial plaque and tartar from around teeth and under the gum line, which is causing bone loss. The goal is to produce clean, healthy teeth and roots, which will !promote healing of the inflammation and infection that causes gum disease. You may take an over-the-counter pain reliever for any tenderness or discomfort. Take ibuprofen !(Advil/Motrin) or acetaminophen (Tylenol) unless you have medical conditions or allergies. After scaling and root planing, avoid eating anything on the area being treated for two hours or until the anesthetic has worn off completely. It is easy to bite or burn your cheek, tongue or lip while numb. Avoid any hard foods such as tortilla chips, potato chips, popcorn, or seeds for the !next several days. To help soothe the area, rinse your mouth 2-3 times a day with warm salt water rinses. If you are !prescribed Peridex/Chlorhexidine, use as directed. Resume your home care regimen of brushing twice a day with a soft bristled toothbrush and daily flossing immediately, but be gentle with the area recently treated. Your gum health must be maintained with proper home care, as instructed, and regular dental visits. You may use a !WaterPik if recommended. It is not unusual for the teeth to be more sensitive to hot or cold temperatures, and/or sweets. This is normal. This occurs as the gum tissue heals and shrinks in size and should gradually resolve in a few weeks with proper home care. -

A Dental Hygienist's Perspective • Periodontal Disease Diagnosis
Treating, Reporting and Managing Periodontal Diseases: A Dental Hygienist’s Perspective Presenter: Kathy S. Forbes, RDH, BS June 23, 2018 12:30-3:30 • Periodontal Disease Diagnosis Case Types I-V and AAP Classifications I-VIII • Chart Documentation Risk Management Issues • Dental “Insurance” Not really insurance . Really! 1 • Treatment Planning for *Non-surgical Dental Hygiene Procedures/Procedure Code Selection *Evaluations *Adult/Child Prophylaxis *Scaling and Root Planing *”Gingivitis” Procedure *Periodontal Maintenance Concerns? There are dental hygienists who provide periodontal procedures (SRP, PM) but document preventive procedures (AP). There are business staff who bill for adult prophylaxis when the hygienist has provided periodontal procedures. 2 Concerns? Both scenarios cause the practice to lose money. Both scenarios would be considered risk management issues. Classification/Case Types of Periodontal Diseases (Based on 1989 World Workshop in Periodontics) Formerly AAP Classification System Case Type I – Early/Chronic Gingivitis Case Type II – Established Gingivitis/Early Periodontitis Case Type III – Moderate/Chronic Periodontitis Case Type IV – Advanced Periodontitis Case Type V – Refractory Periodontitis 3 General Guidelines Extent Severity Localized = 30% or less Slight = of sites are involved LOA/CAL 1-2 mm Generalized = more than Moderate = 30% of sites are involved LOA/CAL 3-4 mm Severe = LOA/CAL 5+ mm LOA = Loss of Attachment CAL = Clinical Attachment Loss Case Types I-V (recognized by most “Insurance” Companies) Case -

Efficacy of Oral Probiotics As an Adjunct to Scaling and Root
IJEDS Ameet Mani et al 10.5005/jp-journals-10029-1145 ORIGINAL RESEARCH Efficacy of Oral Probiotics as an Adjunct to Scaling and Root Planing in Nonsurgical Treatment Outcome of Generalized Chronic Periodontitis Patients: A Clinico-Microbiological Study 1Ameet Mani, 2Rajiv Saini, 3Sugandha R Saini ABSTRACT INTRODUCTION Aim: This study aims to find out the effects of Probiotics, Mouth acts as a window to a lot of systemic diseases and delivered with a lozenge for its effect on clinical and serves as a port of entry of the various infections that microbiological parameters in subjects with chronic periodontitis can alter and affect the immune status of the person. after scaling and root planing (SRP). The oral cavity has the potential to harbor at least 600 Materials and methods: A total of 40 generalized mild to different bacterial species, and in any given patient, moderate chronic periodontitis subjects were finally enrolled in more than 150 species may be present, surfaces of tooth a double-blind, placebo-controlled, randomized clinical study. Selected subjects after SRP were randomly divided into two can have as many as billion bacteria in its attached bac- groups: Group I (test group) with 20 subjects receiving probiotic terial plaque and good oral hygiene is the fundamental tablet once daily and group II (control group) receiving placebo for oral integrity as it greatly affects the quality of life.1 tablets once daily. Clinical parameters and bacterial count for Periodontitis is a destructive inflammatory disease of the Aggregatibacter actinomycetemcomitans, Porphyromonas supporting tissues of the teeth and is caused by specific gingivalis, Prevotella intermedia, Fusobacterium nucleatum were evaluated at baseline, 2, and 4 months after the microorganisms or group of specific microorganisms medication.