Reimbursement Policy Periodontal Codes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Assessment of a Panel of Risk Indicators in Severe Periodontitis Patients
Assessment of a panel of risk indicators in severe periodontitis patients Ciobanu L.¹, Miricescu D. ², Didilescu A.³, Țărmure V.4 ¹PhD Student in Dental Medicine, Division of Microbiology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ²Senior Lecturer, Division of Biochemistry, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania ³Professor, Division of Embryology, Faculty of Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania 4Associate Professor, Department of Orthodontics, Faculty of Dental Medicine, Iuliu Hațieganu University of Medicine and Pharmacy, Cluj-Napoca, Romania Correspondence to: Name: Ciobanu Lidia Address: Blvd. Camil Ressu 49, Bl. H26, Sc. D, Ap.61, Bucharest, Romania Phone: +40 724962500 E-mail address: [email protected] Abstract Aim and objectives The purpose of this study was to analyse a panel of risk indicators in a group of twenty-two patients with severe periodontitis. We also aimed to test possible associations between these indicators and the severity of periodontitis assessed by clinical attachment loss (CAL) mean values. Material and methods Periodontal status was assessed based on the CDC/AAP periodontitis case definition for population-based studies. Risk indicators, including age, gender, weight and height, level of education, and smoking habits, were recorded. Salivary cortisol level, as a marker of chronic stress, was also measured. Results The mean age of the patients was 44.86 (SD 12.81; range 24 to 72). Ten females (45.5%) were enrolled. Testing possible associations between risk indicators and CAL mean values showed no statistical significant correlations, although trends of positive correlations were found between males, BMI, and CAL, respectively Conclusions The present results suggest that a high BMI, as well as masculine gender, could have been important risk factors for severe periodontitis in this study group. -

Instant Update- Getting up to Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 F
Instant Update- Getting Up To Speed in Periodontics for 2019 Pennsylvania Dental Association Gettysburg Meeting April 6, 2019 Francis G. Serio, DMD, MS, MBA Diplomate, American Board of Periodontology Staff Dentist, Greene County Health Care, Inc. Course Synopsis Some things change and some things remain the same. The bedrocks of periodontal therapy are time-tested but new approaches to some of these therapies are providing better outcomes for patients. In addition, advances in the science of periodontics have led to both a better understanding of the disease processes and a new classification system for the periodontal diseases and conditions. In addition, as implant dentistry continues to solidify its position, complications are becoming more commonplace. This course will focus on four main areas: The changes in science that have led to the new classification of the periodontal diseases and conditions. Current understanding of the perio-systemic connection. The “semi-surgical” approach to periodontal therapy. Peri-implant mucositis and peri-implantitis and what to do about it. At the end of this presentation, each participant will be able to: Identify the differences between the 1999 and 2017 disease classification systems. Identify key factors and systemic diseases that have a strong association with the periodontal diseases. Develop a “semi-surgical” treatment plan for a patient with periodontitis. Understand the key factors that contribute to peri-implant disease and possible therapeutic approaches. Periodontitis is a disease of the non-mineralized and mineralized connective tissues- What causes and contributes to its breakdown? Bacterial infections vs. Inflammation 1 Statistical vs. Clinical Significance Clinical significance- Jacobson, et al. -

Periodontal Health, Gingival Diseases and Conditions 99 Section 1 Periodontal Health
CHAPTER Periodontal Health, Gingival Diseases 6 and Conditions Section 1 Periodontal Health 99 Section 2 Dental Plaque-Induced Gingival Conditions 101 Classification of Plaque-Induced Gingivitis and Modifying Factors Plaque-Induced Gingivitis Modifying Factors of Plaque-Induced Gingivitis Drug-Influenced Gingival Enlargements Section 3 Non–Plaque-Induced Gingival Diseases 111 Description of Selected Disease Disorders Description of Selected Inflammatory and Immune Conditions and Lesions Section 4 Focus on Patients 117 Clinical Patient Care Ethical Dilemma Clinical Application. Examination of the gingiva is part of every patient visit. In this context, a thorough clinical and radiographic assessment of the patient’s gingival tissues provides the dental practitioner with invaluable diagnostic information that is critical to determining the health status of the gingiva. The dental hygienist is often the first member of the dental team to be able to detect the early signs of periodontal disease. In 2017, the American Academy of Periodontology (AAP) and the European Federation of Periodontology (EFP) developed a new worldwide classification scheme for periodontal and peri-implant diseases and conditions. Included in the new classification scheme is the category called “periodontal health, gingival diseases/conditions.” Therefore, this chapter will first review the parameters that define periodontal health. Appreciating what constitutes as periodontal health serves as the basis for the dental provider to have a stronger understanding of the different categories of gingival diseases and conditions that are commonly encountered in clinical practice. Learning Objectives • Define periodontal health and be able to describe the clinical features that are consistent with signs of periodontal health. • List the two major subdivisions of gingival disease as established by the American Academy of Periodontology and the European Federation of Periodontology. -

Deep Cleaning (Scaling and Root Planing) Home Care Instructions
Deep Cleaning (Scaling and Root Planing) Home Care Instructions Following the completion of your deep cleaning appointment please follow these home care instructions : - Days 1-3: Warm saltwater rinses 2-3 times daily. A soft food diet is recommended in these initial few days. Days 4-14: Rinse with 1 cap full of Chlorhexidine twice daily after brushing and flossing. Please refrain from eating or drinking for 30 minutes after. Resume twice daily brushing and flossing. Consistent daily oral hygiene is essential to allow proper healing of your gum tissues. - In some cases, local antibiotics may have been placed. If so, please follow the specific instructions that were given to you at your appointment. Others points to Consider: The local anesthesia administered will likely cause your lips, tongue, and cheeks to remain numb for several hours. During this time, please be very careful to not chew, burn, or otherwise injure your lips, tongue, or cheeks. If you must eat while still numb, it is advisable to do so on the opposite side. It is normal to have some mild discomfort after your cleaning. The discomfort is from cleaning plaque and calculus off of the teeth around already inflamed tissue. The multiple injections also will contribute towards your soreness. Motrin may be taken for pain relief, but do not exceed 800mg in 8 hours. After scaling and root planing, you can expect that your gum tissue will be less swollen or prone to bleeding. You may also notice that your teeth feel smoother and your breath smells better. You may experience some thermal sensitivity (especially cold) after your cleaning. -
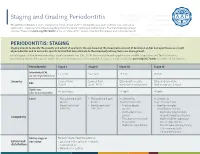
Staging and Grading Periodontitis
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

New Classification of Periodontal Diseases
BDJOpen www.nature.com/bdjopen ARTICLE OPEN New classification of periodontal diseases (NCPD): an application in a sub-Saharan country William Ndjidda Bakari 1, Diabel Thiam1, Ndeye Lira Mbow1, Anna Samb1, Mouhamadou Lamine Guirassy1, Ahmad Moustapha Diallo 1, Abdoulaye Diouf1, Adam Seck Diallo1 and Henri Michel Benoist1 PURPOSE: To determine the clinical and radiological profile of periodontitis according to the 2018 NCPD, in a Dakar (Senegal) based periodontal clinic. METHODS: This is a descriptive study based on patient’s records in the periodontology clinic. The study was conducted between November 2018 and February 2020 (15 months). All periodontitis cases were included in the study. Incomplete records (due to lack of radiographic workup or unusable periodontal charting) were excluded. Periodontitis diagnosis was established based on criteria used in the 2018 NCPD. Statistical analysis was carried out using SPSS version 20.0, with the significance threshold set at 0.05. RESULTS: A total number of 517 patient records were collected during the study period but only 127 periodontitis records were complete. The mean age of participants was 46.8 ± 13.8 years and 63.8% of participants were males. The mean plaque index and bleeding on probing (BOP) were 74% ± 21.3 and 58.1% ± 25.1, respectively. The mean maximum clinical attachment loss was 8.7 mm ±2.7, with a probing depth greater than 6 mm present in 50.4% of the sample. The median number of missing teeth was 3 (interquartile range 5–1). Pathological mobility was present in 60.6% of the patients and 78.0% had occlusion problems. -
04-301E Scaling and Root Planing
Dental Policy Subject: Scaling and Root Planing Guideline #: 04-301E Publish Date: 05/01/2019 Status: Revised Last Review Date: 04/22/2019 Description This document addresses Scaling and Root Planing. Scaling and root planing is a nonsurgical procedure considered appropriate for the treatment of mild to severe periodontal disease. Periodontal scaling and root planing involves instrumentation of the crown and root surfaces of teeth to remove plaque and calculus. This periodontal procedure involves the removal of cementum and dentin permeated by calculus, toxins, and microorganism. It is a definitive non-surgical therapeutic procedure, rather than prophylactic, to treat periodontal disease where migration of the epithelial attachment has caused the formation of periodontal pockets of at least 4 mm. Periodontal scaling and root planing is: 1. A demanding and time-consuming procedure which is technique sensitive involving instrumentation of the tooth crown and root structures. 2. To remove plaque and biofilm, adherent calculus deposits, and diseased cementum (root structure) that may be permeated with calculus, microorganisms and microbial toxins. 3. involves hand instrumentation The plan performs review of scaling and root planing due to contractual requirements that necessitate benefits for dental services meet specific contract requirements. For example, plan contract(s) may require the provision of benefits for services that meet generally accepted standards of dental care at the lowest cost that properly addresses the patient’s condition. The conclusion that a particular service is medically or dentally necessary does not constitute an indication or warranty that the service requested is a covered benefit payable by the dental plan. Documentation Criteria #1 In order to perform review of the scaling and root planning service, diagnostic information is required. -

TO GRAFT OR NOT to GRAFT? an UPDATE on GINGIVAL GRAFTING DIAGNOSIS and TREATMENT MODALITIES Richard J
October 2018 Gingival Recession Autogenous Soft Tissue Grafting Tissue Engineering JournaCALIFORNIA DENTAL ASSOCIATION TO GRAFT OR NOT TO GRAFT? AN UPDATE ON GINGIVAL GRAFTING DIAGNOSIS AND TREATMENT MODALITIES Richard J. Nagy, DDS Ready to save 20%? Let’s go! Discover The Dentists Supply Company’s online shopping experience that delivers CDA members the supplies they need at discounts that make a difference. Price compare and save at tdsc.com. Price comparisons are made to the manufacturer’s list price. Actual savings on tdsc.com will vary on a product-by-product basis. Oct. 2018 CDA JOURNAL, VOL 46, Nº10 DEPARTMENTS 605 The Editor/Nothing but the Tooth 607 Letter to the Editor 609 Impressions 663 RM Matters/Are Your Patients Who They Say They Are? Preventing Medical Identity Theft 667 Regulatory Compliance/OSHA Regulations: Fire Extinguishers, Eyewash, Exit Signs 609 674 Tech Trends FEATURES 615 To Graft or Not To Graft? An Update on Gingival Grafting Diagnosis and Treatment Modalities An introduction to the issue. Richard J. Nagy, DDS 617 Gingival Recession: What Is It All About? This article reviews factors that enhance the risk for gingival recession, describes at what stage interceptive treatment should be recommended and expected outcomes. Debra S. Finney, DDS, MS, and Richard T. Kao, DDS, PhD 625 Autogenous Soft Tissue Grafting for the Treatment of Gingival Recession This article reviews the use of autogenous soft tissue grafting for root coverage. Advantages and disadvantages of techniques are discussed. Case types provide indications for selection and treatment. Elissa Green, DMD; Soma Esmailian Lari, DMD; and Perry R. -

Periodontal Parameters and Tooth Loss Were Associated with C- Reactive Protein and Leukocyte Counts in Adult Population Aged 50 Or Older
Oral Biology Research, 2017; March 31, 41(1):15-22 Copyright ⓒ 2017, Oral Biology Research Institute DOI: 10.21851/obr.41.01.201703.15 ORAL BIOLOGY Original Article RESEARCH Periodontal parameters and tooth loss were associated with C- reactive protein and leukocyte counts in adult population aged 50 or older Ji-Hyun Lee1, Min-Ho Shin2*, Sun-Seog Kweon2,3, Young-Hoon Lee4, Ok-Joon Kim5, Young-Joon Kim1, Hyun- Ju Chung1, and Ok-Su Kim1* 1Department of Periodontology, School of Dentistry, Dental Science Research Institute, Chonnam National University, Gwangju 61186, Republic of Korea 2Department of Preventive Medicine, Chonnam National University Medical School, Gwangju 61469, Republic of Korea 3Jeonnam Regional Cancer Center, Chonnam National University Hwasun Hospital, Hwasun 58128, Republic of Korea 4Department of Preventive Medicine & Institute of Wonkwang Medical Science, Wonkwang University School of Med- icine, Iksan 54538, Republic of Korea 5Department of Oral Pathology, School of Dentistry, Dental Science Research Institute, Chonnam National University, Gwangju 61186, Republic of Korea (Received Nov 8, 2016; Revised version received Jan 12, 2017; Accepted Feb 7, 2017) ABSTRACT ············································································································································································· The association between periodontal disease and cardiovascular disease (CVD) has received considerable attention. This study investigated the correlation between tooth loss (the chief -

Comparative Evaluation of Two Different One-Stage Full-Mouth
ORIGINAL RESEARCH Comparative Evaluation of Two Different One-stage Full-mouth Disinfection Protocols using BANA Assay: A Randomized Clinical Study Arjumand Farooqui1, Vineet V Kini2, Ashvini M Padhye3 ABSTRACT Aim: The aim of this study was to evaluate and compare two different one-stage full-mouth disinfection protocols in the treatment of chronic periodontitis by assessing dental plaque and tongue coat using BANA assay. Materials and methods: The present study was a prospective randomized clinical parallel arm study design including 40 healthy subjects randomly allocated into two groups, i.e., group A (Quirynen’s protocol of one-stage full-mouth disinfection) and group B (Bollen’s protocol of one-stage full-mouth disinfection). Subjects were assessed at baseline and six weeks using plaque index, gingival index, and sulcus bleeding index. Probing depth and relative clinical attachment level were also recorded at six weeks. Winkel tongue coat index and BANA were recorded at 8 weeks using subgingival plaque and tongue coat sample. Results: Both group A and group B demonstrated statistically significant reduction in plaque index, gingival index, sulcus bleeding index, Winkel tongue coat index, reduction in probing depth, and gain in relative clinical attachment level on intragroup comparison. There was no significant difference in BANA assay score of subgingival plaque and tongue coat samples in between group A and group B. Conclusion: From the findings of this study, both Quirynen’s protocol and Bollen’s protocol of one-stage full-mouth disinfection are effective in plaque reduction and tongue coat reduction and achieve comparable clinical healing outcomes. Clinical significance: The difference in duration and mode of use of chlorhexidine as a chemical plaque control agent in the two treatment interventions of Quirynen’s and Bollen’s protocol of one-stage full-mouth disinfection did not demonstrate statistical significance in reducing sulcus bleeding index scores, reducing probing depths, and gain in relative clinical attachment levels. -

Are You Suprised ?
Pretest 2003 with answers/explanations DAPE 761 – Advanced Periodontics Name: ________________________ Dr. Dwight E. McLeod October 24, 2003 PRETEST 1. Gingivectomy is a surgical procedure that is performed to eliminate periodontal pockets and includes eshaping of the gingiva. Gingivoplasty is a surgical procedure that includes reshaping of the gingiva to create physiologic contours with the sole purpose of recontouring the gingiva in the absence of pockets. A. Both statements are true.* B. Both statements are false. C. The first statement is true and the second statement is false. D. The first statement is false and the second statement is true. Gingivectomy means excision of the gingiva. By removing the pocket wall, gingivectomy provides visibility and accessibility for complete calculus removal and thorough smoothing of the roots, creating a favorable environment for gingival healing and restoration of a physiologic gingival contour. Gingivoplasty is similar to gingivectomy, but its purpose is different. Gingivectomy is performed to eliminate periodontal pockets and includes reshaping as part of the technique. Gingivoplasty is a reshaping of the gingival to create physiologic gingival contours, with the sole purpose of recontouring the gingiva in the absence of pockets. 2. Indications for the gingivectomy procedure include: A. Elimination of suprabony pockets. B. Elimination of gingival enlargements. C. Elimination of suprabony periodontal abscesses. D. A and B E. All of the above* The gingivectomy procedure may be performed for (1) elimination of suprabony pockets, regardless of their depth, if the pocket wall is fibrous and firm, (2) elimination of gingival enlargement, and (3) elimination of suprabony periodontal abscesses. 3. Contraindications for the gingivectomy procedure include: A.