Periodontitis Have Struggled to Decide If There Are Different Diseases Or Variations of a Single Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Importance of Chlorhexidine in Maintaining Periodontal Health
International Journal of Dentistry Research 2016; 1(1): 31-33 Review Article Importance of Chlorhexidine in Maintaining Periodontal IJDR 2016; 1(1): 31-33 December Health © 2016, All rights reserved www.dentistryscience.com Dr. Manpreet Kaur*1, Dr. Krishan Kumar1 1 Department of Periodontics, Post Graduate Institute of Dental Sciences, Rohtak-124001, Haryana, India Abstract Plaque is responsible for periodontal diseases. In order to prevent occurrence and progression of periodontal disease, removal of plaque becomes important. Mechanical tooth cleaning aids such as toothbrushes, dental floss, interdental brushes are used for removal of plaque. However, in some cases, chemical agents are used as an adjunct to mechanical methods to facilitate plaque control and prevent gingivitis. Chlorhexidine (CHX) mouthwash is the most commonly used and is considered as gold standard chemical agent. In this review, mechanism of action and other properties of CHX are discussed. Keywords: Plaque, Chemical agents, Chlorhexidine (CHX). INTRODUCTION Dental plaque is primary etiologic factor responsible for gingivitis and periodontitis [1]. Mechanical plaque control using toothbrushes, interdental brushes, dental floss prevent occurrence of gingivitis. However, in majority of population, mechanical methods of plaque control are ineffective due to less time spent[2] for plaque removal and lack of consistency. These limitations necessitate use of chemical plaque control agents as an adjunct to mechanical plaque control. Among various chemical agents, chlorhexidine (CHX) is considered to be a gold standard chemical agent for plaque control. Its structural formula consists of two symmetric 4-chlorophenyl rings and two biguanide groups connected by a central hexamethylene chain. Mechanism of action for CHX CHX is bactericidal and is effective against gram-positive bacteria, gram-negative bacteria and yeast organisms. -

DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

Management of Rapidly Progressing Periodontitis: an Overview
Review Article Management of Rapidly Progressing Periodontitis: An Overview Sadat SMA1, Chowdhury NM2, Baten RBA3 Abstract causes rapid destruction of periodontal ligament and History of periodontal diseases recognition and alveolar bone which occurs in otherwise systemically treatment is ancient for at least 5000 years. There are healthy individuals generally of a younger age group but 1,8 different presentations of periodontal diseases. Rapidly patients may be older . A familial aggregation of the 9 progression periodontitis or aggressive periodontitis disease is also noted . It includes both localized and causes rapid destruction of the periodontium which leads generalized forms. It was previously known as early onset to early tooth loss. It may be generalized or localized. periodontitis that included three categories of periodontitis Periodontitis may be treated surgically or non-surgically - Pubertal, Juvenile and rapidly progressing but patients with rapidly progressing periodontitis do not periodontitis10,11. Early diagnosis and appropriate respond predictably to conventional therapy due to its treatment is necessary to prevent early tooth loss. multi factorial etiology. Successful management of the disease is difficult if not diagnosed early and treated Classification appropriately. Regenerative therapy, tissue engineering Classification of diseases helps the clinicians to develop a and genetic technologies are the new hope for the structure which can be used to identify diseases in relation treatment of rapidly progressing periodontitis. -

Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters
microorganisms Article Probiotic Alternative to Chlorhexidine in Periodontal Therapy: Evaluation of Clinical and Microbiological Parameters Andrea Butera , Simone Gallo * , Carolina Maiorani, Domenico Molino, Alessandro Chiesa, Camilla Preda, Francesca Esposito and Andrea Scribante * Section of Dentistry–Department of Clinical, Surgical, Diagnostic and Paediatric Sciences, University of Pavia, 27100 Pavia, Italy; [email protected] (A.B.); [email protected] (C.M.); [email protected] (D.M.); [email protected] (A.C.); [email protected] (C.P.); [email protected] (F.E.) * Correspondence: [email protected] (S.G.); [email protected] (A.S.) Abstract: Periodontitis consists of a progressive destruction of tooth-supporting tissues. Considering that probiotics are being proposed as a support to the gold standard treatment Scaling-and-Root- Planing (SRP), this study aims to assess two new formulations (toothpaste and chewing-gum). 60 patients were randomly assigned to three domiciliary hygiene treatments: Group 1 (SRP + chlorhexidine-based toothpaste) (control), Group 2 (SRP + probiotics-based toothpaste) and Group 3 (SRP + probiotics-based toothpaste + probiotics-based chewing-gum). At baseline (T0) and after 3 and 6 months (T1–T2), periodontal clinical parameters were recorded, along with microbiological ones by means of a commercial kit. As to the former, no significant differences were shown at T1 or T2, neither in controls for any index, nor in the experimental -

Periodontal Practice Patterns
PERIODONTAL PRACTICE PATTERNS A Thesis Presented in Partial Fulfillment of the Requirements for the Degree Master of Science in the Graduate School of the Ohio State University By Janel Kimberlay Yu, D.D.S. Graduate Program in Dentistry The Ohio State University 2010 Dissertation Committee: Dr. Angelo Mariotti, Advisor Dr. Jed Jacobson Dr. Eric Seiber Copyright by Janel Kimberlay Yu 2010 Abstract Background: Differences in the rates of dental services between geographic regions are important since major discrepancies in practice patterns may suggest an absence of evidence-based clinical information leading to numerous treatment plans for similar dental problems and the misallocation of limited resources. Variations in dental care to patients may result from characteristics of the periodontist. Insurance claims data in this study were compared to the characteristics of periodontal providers to determine if variations in practice patterns exist. Methods: Claims data, between 2000-2009 from Delta Dental of Ohio, Michigan, Indiana, New Mexico, and Tennessee, were examined to analyze the practice patterns of 351 periodontists. For each provider, the average number of select CDT periodontal codes (4000-4999), implants (6010), and extractions (7140) were calculated over two time periods in relation to provider variable, including state, urban versus rural area, gender, experience, location of training, and membership in organized dentistry. Descriptive statistics were performed to depict the data using measures of central tendency and measures of dispersion. ii Results: Differences in periodontal procedures were present across states. Although the most common surgical procedure in the study period was osseous surgery, greater increases over time were observed in regenerative procedures (bone grafts, biologics, GTR) when compared to osseous surgery. -

Aggressive Periodontitis and Its Multidisciplinary Focus: Review of the Literature
ODOVTOS-International Journal of Dental Sciences Frías et al: Aggressive Periodontitis and its Multidisciplinary Focus: Review of the Literature Aggressive Periodontitis and its Multidisciplinary Focus: Review of the Literature Periodontitis agresiva y su enfoque multidisciplinario: Revisión de literatura Maribel Frías-Muñoz DDS¹; Roxana Araujo-Espino DDS, MSc, PhD²; Víctor Manuel Martínez-Aguilar DDS, MSc³; Teresina Correa Alcalde DDS⁴; Luis Alejandro Aguilera-Galaviz DDS, MSc, PhD⁴; César Gaitán-Fonseca DDS, MSc, PhD⁴ 1. Estudiante, Maestría en Ciencias Biomédicas, Área Ciencias de la Salud, Universidad Autónoma de Zacatecas “Francisco García Salinas” (UAZ), Zacatecas, Zac., Mexico. 2. Docente-investigador, Unidad Académica de Enfermería, Área Ciencias de la Salud, Universidad Autónoma de Zacatecas “Francisco García Salinas” (UAZ), Zacatecas, Zac., Mexico. 3. Docente-investigador, Facultad de Odontología, Universidad Autónoma de Yucatán (UADY), Mérida, Yuc., Mexico. 4. Docente-investigador, Área Ciencias de la Salud, Maestría en Ciencias Biomédicas, Universidad Autónoma de Zacatecas “Francisco García Salinas” (UAZ), Zacatecas, Zac., Mexico. Correspondence to: Dr. César Gaitán-Fonseca - [email protected] Received: 1-V-2017 Accepted: 5-V-2017 Published Online First: 8-V-2017 DOI: http://dx.doi.org/10.15517/ijds.v0i0.28869 ABSTRACT The purpose of this review is to have a current prospect of periodontal diseases and, in particular, aggressive periodontitis. To know its classification and clinical characteristics, such as the extent and age group affected, as well as its distribution in the population, etiology, genetic variations, among other factors that could affect the development of this disease. Also, reference is made to different diagnostic options and, likewise, the current treatment options. KEYWORDS Aggressive periodontitis; Periodontal diseases; Diagnosis. -

Classification and Diagnosis of Aggressive Periodontitis
Received: 3 November 2016 Revised: 11 October 2017 Accepted: 21 October 2017 DOI: 10.1002/JPER.16-0712 2017 WORLD WORKSHOP Classification and diagnosis of aggressive periodontitis Daniel H. Fine1 Amey G. Patil1 Bruno G. Loos2 1 Department of Oral Biology, Rutgers School Abstract of Dental Medicine, Rutgers University - Newark, NJ, USA Objective: Since the initial description of aggressive periodontitis (AgP) in the early 2Department of Periodontology, Academic 1900s, classification of this disease has been in flux. The goal of this manuscript is to Center of Dentistry Amsterdam (ACTA), review the existing literature and to revisit definitions and diagnostic criteria for AgP. University of Amsterdam and Vrije Universiteit, Amsterdam, The Netherlands Study analysis: An extensive literature search was performed that included databases Correspondence from PubMed, Medline, Cochrane, Scopus and Web of Science. Of 4930 articles Dr. Daniel H. Fine, Department of Oral reviewed, 4737 were eliminated. Criteria for elimination included; age > 30 years old, Biology, Rutgers School of Dental Medicine, Rutgers University - Newark, NJ. abstracts, review articles, absence of controls, fewer than; a) 200 subjects for genetic Email: fi[email protected] studies, and b) 20 subjects for other studies. Studies satisfying the entrance criteria The proceedings of the workshop were were included in tables developed for AgP (localized and generalized), in areas related jointly and simultaneously published in the Journal of Periodontology and Journal of to epidemiology, microbial, host and genetic analyses. The highest rank was given to Clinical Periodontology. studies that were; a) case controlled or cohort, b) assessed at more than one time-point, c) assessed for more than one factor (microbial or host), and at multiple sites. -
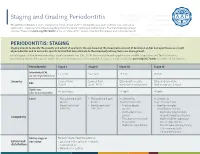
Staging and Grading Periodontitis
Staging and Grading Periodontitis The 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions resulted in a new classification of periodontitis characterized by a multidimensional staging and grading system. The charts below provide an overview. Please visit perio.org/2017wwdc for the complete suite of reviews, case definition papers, and consensus reports. PERIODONTITIS: STAGING Staging intends to classify the severity and extent of a patient’s disease based on the measurable amount of destroyed and/or damaged tissue as a result of periodontitis and to assess the specific factors that may attribute to the complexity of long-term case management. Initial stage should be determined using clinical attachment loss (CAL). If CAL is not available, radiographic bone loss (RBL) should be used. Tooth loss due to periodontitis may modify stage definition. One or more complexity factors may shift the stage to a higher level. Seeperio.org/2017wwdc for additional information. Periodontitis Stage I Stage II Stage III Stage IV Interdental CAL 1 – 2 mm 3 – 4 mm ≥5 mm ≥5 mm (at site of greatest loss) Severity Coronal third Coronal third Extending to middle Extending to middle RBL (<15%) (15% - 33%) third of root and beyond third of root and beyond Tooth loss No tooth loss ≤4 teeth ≥5 teeth (due to periodontitis) Local • Max. probing depth • Max. probing depth In addition to In addition to ≤4 mm ≤5 mm Stage II complexity: Stage III complexity: • Mostly horizontal • Mostly horizontal • Probing depths • Need for -

The Roots of Periodontology
THE ROOTS OF PERIODONTOLOGY NMDHA 24th Annual Scientific Session Dennis Miller DMD, MS Diplomate, American Board of Periodontology Oct 19, 2012 A word about the value of history…… Those who don’t know history are destined to repeat it. Edmond Burke (1729-1797) Those of you who don’t remember the past are condemned to repeat it. • George Santayama, 1890 The History of Dentistry • Barbers and blacksmiths were the first dentists in America • 1840 – opening of the first dental school, University of Baltimore • 1859 – ADA was founded, oldest and largest national Dental Society in the world • 1890 – Dr. John Riggs describes periodontal disease • Calls it Riggs disease or pyorrhea • Marketed Anti-Riggs mouthwash (156 proof) • 1896 – Dr. G.V. Black who is known as the father of modern dentistry, describes cavity preparations • 1906 – Dr. C. Edmund Kells exposes first dental radiograph; also the first to use female dental assistants and surgical aspirators • 1929 – Orthodontics recognized as first dental specialty History of Periodontics • 1914 – Dr. Grace Rodgers Spalding and Dr. Gillette Hayden (both physicians) formed the American Academy of Oral Prophylaxis and Periodontology • 1919 – became the American Academy of Periodontology • Circa 1941 - Periodontics recognized as a dental specialty History of Hygiene • 1867 – Lucy Hobbs Taylor graduated from Ohio College of Dental Surgery as a hygienist • 1884 – paper presented at the NY 1st District Dental Society meeting advocating teeth cleaning for prevention, done by “staff” • 1923 – formation of ADHA Historical names of periodontitis • Loculosis • Blennorrhea gingivae • Periostitis • Alveolodental periostitis • Infectious arthrodental gingivitis • Phagedenic pericementitis • Expulsive gingivitis • Symptomatic alveolar arthritis • Smutz pyorrhea • Riggs disease • Periodontoclasia • Pyorrhea alveolaris The roots of Periodontology • The roots of the dental profession including periodontics and dental hygiene were not concocted by some entrepreneur. -

Retrospective Analysis of the Risk Factors of Peri-Implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5
ORIGINAL RESEARCH Retrospective Analysis of the Risk Factors of Peri-implantitis Nathan Anderson1, Adam Lords2, Ronald Laux3, Wendy Woodall4, Neamat Hassan Abubakr5 ABSTRACT Aim and objective: Peri-implantitis is a key concern for dental implants and the main common reason for implant failure. This investigation evaluated the risk factors and their implications on peri-implantitis. Materials and methods: A retrospective search of the patients’ clinical notes was performed to identify the documented cases of peri-implantitis. The inclusion criteria encompassed patients who were 18 years and older and were seen at the School of Dental Medicine, University of Nevada, Las Vegas, from January 2014 through September 2018. The search revealed that the number of peri-implantitis cases was 28, with an overall 45 implants. Data were collected and analyzed using the Chi-square test. Results: Total 28 patients presented with peri-implantitis. The distribution of males to females with peri-implantitis was 60.7 and 39.3%, respectively. The highest number of patients (21.4%) presenting with peri-implantitis fell within the age range of 65–69 years; 53.3% of peri- implantitis cases were in the maxillary arch. The predilection area for peri-implantitis was the mandibular first molar (24.4%). Periodontitis was the most significant cause (60.7%); respiratory diseases (42.9%) followed by hypertension (28.6%) were the most prevalent medical conditions in the studied population. Peri-implantitis occurred most frequently among Caucasians (62.7%), followed by Hispanics (29%). Conclusion: Within the limitations of the current evaluation, findings support previous claims that periodontitis remains the strongest predictor of peri-implantitis. -

Tobacco and Your Oral Health
Oral Wellness Series Tobacco and Your Oral Health We all know smoking is bad for us, but did you know that chewing tobacco is just as harmful to your oral health as cigarettes? Tobacco causes bad breath, which nobody likes, but it has far more serious risks to your oral health, including: • Mouth sores • Slow healing after oral surgery • Difficulties correcting cosmetic dental problems • Stained teeth and tongue • Dulled sense of taste and smell The Biggest Risk? Did you know tobacco Cancer. The Centers for Disease Control have linked smoking and use is a huge risk factor tobacco use to oral cancer. Oral cancer is the eighth most common cancer in the U.S., and it’s very difficult to detect. As a result, two- for gum disease? thirds of all cases are diagnosed in late stages, making treatment and survival difficult.1 Tobacco and Gum Disease Tobacco use is also a huge risk factor for gum disease, a leading cause of tooth loss. More than 41% of daily smokers over the age of 65 are toothless because of gum disease, compared to only 20% of non-smokers.2 Maintain good oral health by avoiding tobacco. It keeps your whole body healthier. The Effects of Smoking on Your Gums Smoking reduces blood flow to your gums, cutting Is Smokeless Tobacco Safer? off vital nutrients and preventing bones from healing. Smokeless tobacco—chew, dip and snuff—is not This lets bacteria from tartar infect surrounding tissue, regulated by the FDA so it’s hard to know what’s in it. 3 forming deep pockets between teeth and gums. -

Treatment of Localized Aggressive Periodontitis Regenerative Periodontal Therapy Offers Alternative to Extraction/Implant Placement Ahmad Soolari, DMD, MS
Inside PERIODONTICS PEER-REVIEWED Treatment of Localized Aggressive Periodontitis Regenerative periodontal therapy offers alternative to extraction/implant placement Ahmad Soolari, DMD, MS ue to the effect of im- with inconsistent margins, which could be was localized aggressive periodontitis. The plant-related compli- measured from the cementoenamel junc- patient’s medical history was unremarkable, cations, the longevity of tion or from the crest of the alveolar bone but a significant finding was the retention of implants is often ques- to the base of the defect. A periapical ra- primary teeth with premolar impaction on tionable, even when diograph showed angular bone loss on the the lower right side. The patient was later compared with that of distal aspect of tooth No. 24 with an angle referred to an orthodontist for consultation. compromised but suc- of almost 45°. The interproximal space be- The goal of regenerative periodontal cessfully treated natural teeth. This article de- tween tooth No. 24 and tooth No. 23 was the therapy is to improve a tooth’s prognosis by Dscribes a case of severe, localized periodontal only site with severe bone loss throughout regenerating the supporting structures. In disease in which the patient rejected a recom- the patient’s mouth; therefore, the diagnosis this case, the prognosis for tooth No. 24 was mendation to undergo extraction followed by implant placement and restoration in favor of receiving regenerative periodontal therapy to save the natural tooth. Case Report A 17-year-old female patient presented with bone loss associated with tooth No. 24. A clinical examination and periodontal eval- uation (ie, assessment of mobility, probing depth, bleeding on probing, plaque score, and clinical attachment loss) revealed severe horizontal and vertical bone loss, deep prob- ing depth with bleeding, class II mobility, a FIG.