Fecal Microbiota Alterations and Small Intestinal Bacterial Overgrowth in Functional Abdominal Bloating/Distention
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

16S Rdna Full-Length Assembly Sequencing Technology Analysis of Intestinal Microbiome in Polycystic Ovary Syndrome
ORIGINAL RESEARCH published: 10 May 2021 doi: 10.3389/fcimb.2021.634981 16S rDNA Full-Length Assembly Sequencing Technology Analysis of Intestinal Microbiome in Polycystic Ovary Syndrome Sitong Dong 1, Jiao jiao 1, Shuangshuo Jia 2, Gaoyu Li 1, Wei Zhang 1, Kai Yang 3, Zhen Wang 3, Chao Liu 4,DaLi1 and Xiuxia Wang 1* Edited by: 1 Center of Reproductive Medicine, Shengjing Hospital of China Medical University, Shenyang, China, 2 Department of 3 Tao Lin, Orthopedic Surgery, Shengjing Hospital of China Medical University, Shenyang, China, Department of Research and 4 Baylor College of Medicine, Development, Germountx Company, Beijing, China, Department of Biological Information, Kangwei Medical Analysis United States Laboratory, Shenyang, China Reviewed by: Barbara Obermayer-Pietsch, Objective: To study the characteristics and relationship of the gut microbiota in patients Medical University of Graz, Austria with polycystic ovary syndrome (PCOS). Julio Plaza-Diaz, Children’s Hospital of Eastern Ontario Method: We recruited 45 patients with PCOS and 37 healthy women from the (CHEO), Canada Alberto Sola-Leyva, Reproductive Department of Shengjing Hospital. We recorded their clinical indexes, University of Granada, Spain and sequenced their fecal samples by 16S rDNA full-length assembly sequencing Yanli Pang, technology (16S-FAST). Peking University Third Hospital, China Result: We found decreased a diversity and different abundances of a series of microbial *Correspondence: species in patients with PCOS compared to healthy controls. We found LH and AMH were Xiuxia Wang fi [email protected] signi cantly increased in PCOS with Prevotella enterotype when compared to control women with Prevotella enterotype, while glucose and lipid metabolism level remained no Specialty section: significant difference, and situations were opposite in PCOS and control women with This article was submitted to Bacteroides enterotype. -

WO 2018/064165 A2 (.Pdf)
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/064165 A2 05 April 2018 (05.04.2018) W !P O PCT (51) International Patent Classification: Published: A61K 35/74 (20 15.0 1) C12N 1/21 (2006 .01) — without international search report and to be republished (21) International Application Number: upon receipt of that report (Rule 48.2(g)) PCT/US2017/053717 — with sequence listing part of description (Rule 5.2(a)) (22) International Filing Date: 27 September 2017 (27.09.2017) (25) Filing Language: English (26) Publication Langi English (30) Priority Data: 62/400,372 27 September 2016 (27.09.2016) US 62/508,885 19 May 2017 (19.05.2017) US 62/557,566 12 September 2017 (12.09.2017) US (71) Applicant: BOARD OF REGENTS, THE UNIVERSI¬ TY OF TEXAS SYSTEM [US/US]; 210 West 7th St., Austin, TX 78701 (US). (72) Inventors: WARGO, Jennifer; 1814 Bissonnet St., Hous ton, TX 77005 (US). GOPALAKRISHNAN, Vanch- eswaran; 7900 Cambridge, Apt. 10-lb, Houston, TX 77054 (US). (74) Agent: BYRD, Marshall, P.; Parker Highlander PLLC, 1120 S. Capital Of Texas Highway, Bldg. One, Suite 200, Austin, TX 78746 (US). (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -
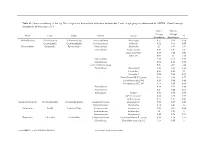
Genus Contributing to the Top 70% of Significant Dissimilarity of Bacteria Between Day 7 and 18 Age Groups As Determined by SIMPER
Table S1: Genus contributing to the top 70% of significant dissimilarity of bacteria between day 7 and 18 age groups as determined by SIMPER. Overall average dissimilarity between ages is 51%. Day 7 Day 18 Average Average Phyla Class Order Family Genus % Abundance Abundance Actinobacteria Actinobacteria Actinomycetales Actinomycetaceae Actinomyces 0.57 0.24 0.74 Coriobacteriia Coriobacteriales Coriobacteriaceae Collinsella 0.51 0.61 0.57 Bacteroidetes Bacteroidia Bacteroidales Bacteroidaceae Bacteroides 2.1 1.63 1.03 Marinifilaceae Butyricimonas 0.82 0.81 0.9 Sanguibacteroides 0.08 0.42 0.59 CAG-873 0.01 1.1 1.68 Marinifilaceae 0.38 0.78 0.91 Marinifilaceae 0.78 1.04 0.97 p-2534-18B5 gut group 0.06 0.7 1.04 Prevotellaceae Alloprevotella 0.46 0.83 0.89 Prevotella 2 0.95 1.11 1.3 Prevotella 7 0.22 0.42 0.56 Prevotellaceae NK3B31 group 0.62 0.68 0.77 Prevotellaceae UCG-003 0.26 0.64 0.89 Prevotellaceae UCG-004 0.11 0.48 0.68 Prevotellaceae 0.64 0.52 0.89 Prevotellaceae 0.27 0.42 0.55 Rikenellaceae Alistipes 0.39 0.62 0.77 dgA-11 gut group 0.04 0.38 0.56 RC9 gut group 0.79 1.17 0.95 Epsilonbacteraeota Campylobacteria Campylobacterales Campylobacteraceae Campylobacter 0.58 0.83 0.97 Helicobacteraceae Helicobacter 0.12 0.41 0.6 Firmicutes Bacilli Lactobacillales Enterococcaceae Enterococcus 0.36 0.31 0.64 Lactobacillaceae Lactobacillus 1.4 1.24 1 Streptococcaceae Streptococcus 0.82 0.58 0.53 Firmicutes Clostridia Clostridiales Christensenellaceae Christensenellaceae R-7 group 0.38 1.36 1.56 Clostridiaceae Clostridium sensu stricto 1 1.16 0.58 -

Bacteriophages As Potential New Mammalian Pathogens George V
www.nature.com/scientificreports OPEN Bacteriophages as potential new mammalian pathogens George V. Tetz 1, Kelly V. Ruggles2,3, Hua Zhou3, Adriana Heguy4,5,6, Aristotelis Tsirigos3,4,5 & Victor Tetz1 Received: 4 May 2017 Increased intestinal permeability and translocation of gut bacteria trigger various polyaetiological Accepted: 23 June 2017 diseases associated with chronic infammation and underlie a variety of poorly treatable pathologies. Published online: 1 August 2017 Previous studies have established a primary role of the microbiota composition and intestinal permeability in such pathologies. Using a rat model, we examined the efects of exposure to a bacteriophage cocktail on intestinal permeability and relative abundance of taxonomic units in the gut bacterial community. There was an increase in markers of impaired gut permeability, such as the lactulose/mannitol ratio, plasma endotoxin concentrations, and serum levels of infammation- related cytokines, following the bacteriophage challenge. We observed signifcant diferences in the alpha diversity of faecal bacterial species and found that richness and diversity index values increased following the bacteriophage challenge. There was a reduction in the abundance of Blautia, Catenibacterium, Lactobacillus, and Faecalibacterium species and an increase in Butyrivibrio, Oscillospira and Ruminococcus after bacteriophage administration. These fndings provide novel insights into the role of bacteriophages as potentially pathogenic for mammals and their possible implication in the development of diseases associated with increased intestinal permeability. Our knowledge of the intestinal microbiota has greatly expanded over the last decade, and growing evidence sug- gests that alterations of the intestinal microbiota are critical pathogenic factors that trigger various polyaetiologi- cal diseases associated with increased intestinal permeability and chronic infammation1–3. -

Gut Microbiome and Serum Metabolome Alterations in Isolated Dystonia
Gut microbiome and serum metabolome alterations in isolated dystonia Yongfeng Hu ( [email protected] ) Chinese Academy of Medical Sciences & Peking Union Medical College Institute of Pathogen Biology https://orcid.org/0000-0003-3799-5526 Ling yan Ma Center for Movement disorders Min Cheng China Institute of Veterinary Drug Control Bo Liu Institute of pathogen Biology Hua Pan Center for Movement Disorders Jian Yang Institute of Pathogen Biology Tao Feng Center for Movement Disorders Qi Jin Chinese Academy of Medical Sciences & Peking Union Medical College Institute of Pathogen Biology Research Keywords: Dystonia, Gut microbiome, Serum metabolomics, Multi-omics analysis Posted Date: January 6th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-139606/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/19 Abstract Background Dystonia is a complex neurological movement disorder characterised by involuntary muscle contractions. The relationship between the gut microbiota and isolated dystonia remains poorly explored. Methods We collected faeces and blood samples to study the microbiome and the serum metabolome from a cohort of 57 drug-naïve isolated dystonia patients and 27 age- and environment-matched healthy individuals. We rst sequenced the V4 regions of the 16S rDNA gene from all faeces samples. Further, we performed metagenomic sequencing of gut microbiome and non-targeted metabolomics proling of serum from dystonia patients with signicant dysbiosis. Results Gut microbial β-diversity was signicantly different, with a more heterogeneous community structure among dystonia individuals than healthy controls, while no difference in α-diversity was found. Gut microbiota in dystonia patients was enriched with Blautia obeum, Dorea longicatena and Eubacterium hallii, but depleted with Bacteroides vulgatus and Bacteroides plebeius. -

Metatranscriptomic Analysis to Define the Secrebiome, and 16S Rrna
Gallardo‑Becerra et al. Microb Cell Fact (2020) 19:61 https://doi.org/10.1186/s12934‑020‑01319‑y Microbial Cell Factories RESEARCH Open Access Metatranscriptomic analysis to defne the Secrebiome, and 16S rRNA profling of the gut microbiome in obesity and metabolic syndrome of Mexican children Luigui Gallardo‑Becerra1†, Fernanda Cornejo‑Granados1†, Rodrigo García‑López1†, Alejandra Valdez‑Lara1, Shirley Bikel1, Samuel Canizales‑Quinteros2, Blanca E. López‑Contreras2, Alfredo Mendoza‑Vargas3, Henrik Nielsen4 and Adrián Ochoa‑Leyva1* Abstract Background: In the last decade, increasing evidence has shown that changes in human gut microbiota are asso‑ ciated with diseases, such as obesity. The excreted/secreted proteins (secretome) of the gut microbiota afect the microbial composition, altering its colonization and persistence. Furthermore, it infuences microbiota‑host interac‑ tions by triggering infammatory reactions and modulating the host’s immune response. The metatranscriptome is essential to elucidate which genes are expressed under diseases. In this regard, little is known about the expressed secretome in the microbiome. Here, we use a metatranscriptomic approach to delineate the secretome of the gut microbiome of Mexican children with normal weight (NW) obesity (O) and obesity with metabolic syndrome (OMS). Additionally, we performed the 16S rRNA profling of the gut microbiota. Results: Out of the 115,712 metatranscriptome genes that codifed for proteins, 30,024 (26%) were predicted to be secreted, constituting the Secrebiome of the -

Degradation of Marine Algae-Derived Carbohydrates by Bacteroidetes
Article Degradation of Marine Algae‐Derived Carbohydrates by Bacteroidetes Isolated from Human Gut Microbiota Miaomiao Li 1,2, Qingsen Shang 1, Guangsheng Li 3, Xin Wang 4,* and Guangli Yu 1,2,* 1 Shandong Provincial Key Laboratory of Glycoscience and Glycoengineering, School of Medicine and pharmacy, Ocean University of China, Qingdao 266003, China; [email protected] (M.L.); [email protected] (Q.S.) 2 Laboratory for Marine Drugs and Bioproducts of Qingdao National Laboratory for Marine Science and Technology, Qingdao 266237, China 3 DiSha Pharmaceutical Group, Weihai 264205, China; gsli‐[email protected] 4 State Key Laboratory of Breeding Base for Zhejiang Sustainable Pest and Disease Control and Zhejiang Key Laboratory of Food Microbiology, Academy of Agricultural Sciences, Hangzhou 310021, China * Correspondence: [email protected] (X.W.); [email protected] (G.Y.); Tel.: +86‐571‐8641‐5216 (X.W.); +86‐532‐8203‐1609 (G.Y.) Academic Editor: Paola Laurienzo Received: 2 January 2017; Accepted: 20 March 2017; Published: 24 March 2017 Abstract: Carrageenan, agarose, and alginate are algae‐derived undigested polysaccharides that have been used as food additives for hundreds of years. Fermentation of dietary carbohydrates of our food in the lower gut of humans is a critical process for the function and integrity of both the bacterial community and host cells. However, little is known about the fermentation of these three kinds of seaweed carbohydrates by human gut microbiota. Here, the degradation characteristics of carrageenan, agarose, alginate, and their oligosaccharides, by Bacteroides xylanisolvens, Bacteroides ovatus, and Bacteroides uniforms, isolated from human gut microbiota, are studied. Keywords: carrageenan; agarose; alginate; oligosaccharides; Bacteroides xylanisolvens; Bacteroides ovatus; Bacteroides uniforms 1. -

Depression and Microbiome—Study on the Relation and Contiguity Between Dogs and Humans
applied sciences Article Depression and Microbiome—Study on the Relation and Contiguity between Dogs and Humans Elisabetta Mondo 1,*, Alessandra De Cesare 1, Gerardo Manfreda 2, Claudia Sala 3 , Giuseppe Cascio 1, Pier Attilio Accorsi 1, Giovanna Marliani 1 and Massimo Cocchi 1 1 Department of Veterinary Medical Science, University of Bologna, Via Tolara di Sopra 50, 40064 Ozzano Emilia, Italy; [email protected] (A.D.C.); [email protected] (G.C.); [email protected] (P.A.A.); [email protected] (G.M.); [email protected] (M.C.) 2 Department of Agricultural and Food Sciences, University of Bologna, Via del Florio 2, 40064 Ozzano Emilia, Italy; [email protected] 3 Department of Physics and Astronomy, Alma Mater Studiorum, University of Bologna, 40126 Bologna, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-051-209-7329 Received: 22 November 2019; Accepted: 7 January 2020; Published: 13 January 2020 Abstract: Behavioral studies demonstrate that not only humans, but all other animals including dogs, can suffer from depression. A quantitative molecular evaluation of fatty acids in human and animal platelets has already evidenced similarities between people suffering from depression and German Shepherds, suggesting that domestication has led dogs to be similar to humans. In order to verify whether humans and dogs suffering from similar pathologies also share similar microorganisms at the intestinal level, in this study the gut-microbiota composition of 12 German Shepherds was compared to that of 15 dogs belonging to mixed breeds which do not suffer from depression. Moreover, the relation between the microbiota of the German Shepherd’s group and that of patients with depression has been investigated. -

Composition of Rabbit Caecal Microbiota and the Effects of Dietary Quercetin Supplementation and Sex Thereupon North M.K
W orld World Rabbit Sci. 2019, 27: 185-198 R abbit doi:10.4995/wrs.2019.11905 Science © WRSA, UPV, 2003 COMPOSITION OF RABBIT CAECAL MICROBIOTA AND THE EFFECTS OF DIETARY QUERCETIN SUPPLEMENTATION AND SEX THEREUPON NORTH M.K. *, DALLE ZOTTE A. †, HOFFMAN L.C. *‡ *Department of Animal Sciences, Stellenbosch University, Private Bag X1, Matieland, STELLENBOSCH 7602, South Africa. †Department of Animal Medicine, Production and Health, University of Padova, Agripolis, Viale dell’Università, 16, 35020 LEGNARO, Padova, Italy. ‡Centre for Nutrition and Food Sciences, Queensland Alliance for Agriculture and Food Innovation (QAAFI), The University of Queensland, Health and Food Sciences Precinct, 39 Kessels Road, COOPERS PLAINS 4108, Australia. Abstract: The purpose of this study was to add to the current understanding of rabbit caecal microbiota. This involved describing its microbial composition and linking this to live performance parameters, as well as determining the effects of dietary quercetin (Qrc) supplementation (2 g/kg feed) and sex on the microbial population. The weight gain and feed conversion ratio of twelve New Zealand White rabbits was measured from 5 to 12 wk old, blood was sampled at 11 wk old for the determination of serum hormone levels, and the rabbits were slaughtered and caecal samples collected at 13 wk old. Ion 16STM metagenome sequencing was used to determine the microbiota profile. The dominance of Firmicutes (72.01±1.14% of mapped reads), Lachnospiraceae (23.94±1.01%) and Ruminococcaceae (19.71±1.07%) concurred with previous reports, but variation both between studies and individual rabbits was apparent beyond this. Significant correlations between microbial families and live performance parameters were found, suggesting that further research into the mechanisms of these associations could be useful. -

Taxonomy of Lactobacilli and Bifidobacteria
Curr. Issues Intestinal Microbiol. 8: 44–61. Online journal at www.ciim.net Taxonomy of Lactobacilli and Bifdobacteria Giovanna E. Felis and Franco Dellaglio*† of carbohydrates. The genus Bifdobacterium, even Dipartimento Scientifco e Tecnologico, Facoltà di Scienze if traditionally listed among LAB, is only poorly MM. FF. NN., Università degli Studi di Verona, Strada le phylogenetically related to genuine LAB and its species Grazie 15, 37134 Verona, Italy use a metabolic pathway for the degradation of hexoses different from those described for ‘genuine’ LAB. Abstract The interest in what lactobacilli and bifdobacteria are Genera Lactobacillus and Bifdobacterium include a able to do must consider the investigation of who they large number of species and strains exhibiting important are. properties in an applied context, especially in the area of Before reviewing the taxonomy of those two food and probiotics. An updated list of species belonging genera, some basic terms and concepts and preliminary to those two genera, their phylogenetic relationships and considerations concerning bacterial systematics need to other relevant taxonomic information are reviewed in this be introduced: they are required for readers who are not paper. familiar with taxonomy to gain a deep understanding of The conventional nature of taxonomy is explained the diffculties in obtaining a clear taxonomic scheme for and some basic concepts and terms will be presented for the bacteria under analysis. readers not familiar with this important and fast-evolving area, -

000572305300015.Pdf(1.52
www.nature.com/scientificreports OPEN Compositional and functional diferences of the mucosal microbiota along the intestine of healthy individuals Stefania Vaga1,15, Sunjae Lee1,15, Boyang Ji2, Anna Andreasson3,4,5, Nicholas J. Talley6, Lars Agréus7, Gholamreza Bidkhori1, Petia Kovatcheva‑Datchary8,9, Junseok Park10, Doheon Lee10, Gordon Proctor1, Stanislav Dusko Ehrlich11, Jens Nielsen2,12*, Lars Engstrand13* & Saeed Shoaie1,14* Gut mucosal microbes evolved closest to the host, developing specialized local communities. There is, however, insufcient knowledge of these communities as most studies have employed sequencing technologies to investigate faecal microbiota only. This work used shotgun metagenomics of mucosal biopsies to explore the microbial communities’ compositions of terminal ileum and large intestine in 5 healthy individuals. Functional annotations and genome‑scale metabolic modelling of selected species were then employed to identify local functional enrichments. While faecal metagenomics provided a good approximation of the average gut mucosal microbiome composition, mucosal biopsies allowed detecting the subtle variations of local microbial communities. Given their signifcant enrichment in the mucosal microbiota, we highlight the roles of Bacteroides species and describe the antimicrobial resistance biogeography along the intestine. We also detail which species, at which locations, are involved with the tryptophan/indole pathway, whose malfunctioning has been linked to pathologies including infammatory bowel disease. Our -
Sub-Clinical Detection of Gut Microbial Biomarkers of Obesity and Type 2 Diabetes Moran Yassour1,2, Mi Young Lim3, Hyun Sun Yun3, Timothy L
Yassour et al. Genome Medicine (2016) 8:17 DOI 10.1186/s13073-016-0271-6 RESEARCH Open Access Sub-clinical detection of gut microbial biomarkers of obesity and type 2 diabetes Moran Yassour1,2, Mi Young Lim3, Hyun Sun Yun3, Timothy L. Tickle4,5, Joohon Sung3, Yun-Mi Song6, Kayoung Lee7, Eric A. Franzosa1,4, Xochitl C. Morgan1,4, Dirk Gevers1,8, Eric S. Lander1,9,10, Ramnik J. Xavier1,2,11,12, Bruce W. Birren1, GwangPyo Ko3 and Curtis Huttenhower1,4* Abstract Background: Obesity and type 2 diabetes (T2D) are linked both with host genetics and with environmental factors, including dysbioses of the gut microbiota. However, it is unclear whether these microbial changes precede disease onset. Twin cohorts present a unique genetically-controlled opportunity to study the relationships between lifestyle factors and the microbiome. In particular, we hypothesized that family-independent changes in microbial composition and metabolic function during the sub-clinical state of T2D could be either causal or early biomarkers of progression. Methods: We collected fecal samples and clinical metadata from 20 monozygotic Korean twins at up to two time points, resulting in 36 stool shotgun metagenomes. While the participants were neither obese nor diabetic, they spanned the entire range of healthy to near-clinical values and thus enabled the study of microbial associations during sub-clinical disease while accounting for genetic background. Results: We found changes both in composition and in function of the sub-clinical gut microbiome, including a decrease in Akkermansia muciniphila suggesting a role prior to the onset of disease, and functional changes reflecting a response to oxidative stress comparable to that previously observed in chronic T2D and inflammatory bowel diseases.