Oogenesis and Follicular Development AP Biology > Reproduction and Development > Reproduction and Development
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
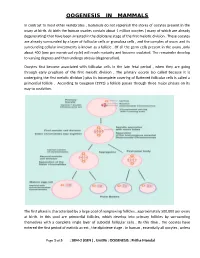
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model. -

Interactions Between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction Fritzsche H, Michelmann HW, Siebzehnrübl E Schmedemann RKA J
Journal für Reproduktionsmedizin und Endokrinologie – Journal of Reproductive Medicine and Endocrinology – Andrologie • Embryologie & Biologie • Endokrinologie • Ethik & Recht • Genetik Gynäkologie • Kontrazeption • Psychosomatik • Reproduktionsmedizin • Urologie Interactions between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction Fritzsche H, Michelmann HW, Siebzehnrübl E Schmedemann RKA J. Reproduktionsmed. Endokrinol 2006; 3 (6), 373-378 www.kup.at/repromedizin Online-Datenbank mit Autoren- und Stichwortsuche Offizielles Organ: AGRBM, BRZ, DVR, DGA, DGGEF, DGRM, D·I·R, EFA, OEGRM, SRBM/DGE Indexed in EMBASE/Excerpta Medica/Scopus Krause & Pachernegg GmbH, Verlag für Medizin und Wirtschaft, A-3003 Gablitz Interactions between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction H. Fritzsche1, H. W. Michelmann2, E. Siebzehnrübl3, R. K. A. Schmedemann4 The interactions between oocyte and surrounding cumulus cells, as well as between cumulus oophorus and theca cells, were investigated in IVF/ ICSI cycles. Gap junctions connect cumulus cells with the oocyte, thereby enabling a bi-directional exchange of products essential for optimal oocyte development. GnRH, FSH, LH and E2 play a major role during oocyte maturation. In general, FSH and LH are prerequisites for folliculogenesis, as well as oogenesis, but it is the quantitative threshold value of both that seems to determine oocyte quality and pregnancy rate. It remains to be determined how apoptosis and the anti-Muellerian hormone (AMH) can be used as predictive factors regarding the success of ART. In a retrospec- tive sub-analysis of comparative stimulation regimens, using either LH + FSH (hMG-HP) or FSH (rFSH) alone in GnRH-antagonist down-regulated cycles, it was possible to demonstrate that stimulation with LH and FSH results in a significantly higher pregnancy rate in IVF-patients compared to a stimulation with only FSH. -

Most Fertilizing Mouse Spermatozoa Begin Their Acrosome Reaction Before Contact with the Zona Pellucida During in Vitro Fertilization
Most fertilizing mouse spermatozoa begin their acrosome reaction before contact with the zona pellucida during in vitro fertilization Mayuko Jina, Eiji Fujiwarab, Yasutaka Kakiuchia,c, Masaru Okabed, Yuhkoh Satouhd,e, Shoji A. Babaa, Kazuyoshi Chibaa,f, and Noritaka Hirohashia,c,f,1 aDepartment of Biological Sciences, cDepartment of Genetic Counseling, and fGlycoscience Institute, Ochanomizu University, Tokyo 112-8610, Japan; bDocumentary Channel Co., Kawaguchi, Saitama 333-0844, Japan; and dResearch Institute for Microbial Disease and eWorld Premier International Research Center (WPI) Immunology Frontier Research Center, Osaka University, Osaka 565-0871, Japan Edited* by Ryuzo Yanagimachi, Institute for Biogenesis Research, University of Hawaii, Honolulu, HI, and approved February 16, 2011 (received for review December 5, 2010) To fuse with oocytes, spermatozoa of eutherian mammals must spermatozoa within the cumulus at various stages of the AR in pass through extracellular coats, the cumulus cell layer, and the various species has also been noted by several investigators (11– zona pellucida (ZP). It is generally believed that the acrosome 14). This prompted us to reexamine the site of the AR in those reaction (AR) of spermatozoa, essential for zona penetration and mouse spermatozoa that actually participate in fertilization. We fusion with oocytes, is triggered by sperm contact with the zona used a video microscopic in vitro fertilization (VMIVF) system, pellucida. Therefore, in most previous studies of sperm–oocyte which allowed us to determine the site of the AR in fertilizing interactions in the mouse, the cumulus has been removed before mouse spermatozoa, retrospectively (Fig. 1). We used double- insemination to facilitate the examination of sperm–zona interac- transgenic male mice whose spermatozoa express enhanced green tions. -

Other Useful Books
Other Useful Books Dictionaries: Leeson TS, Leeson CR: Histology, 4th ed. Philadel phia: Saunders, 1981. Dorland's Illustrated Medical Dictionary, 26th ed. Lentz, TL: Cell Fine Structure. Philadelphia: Saun Philadelphia: Saunders, 1981. ders, 1971. Melloni's Illustrated Medical Dictionary. Balti Rhodin JAG: Histology, A Text and Atlas. New more: Williams and Wilkins, 1979. York: Oxford University Press, 1974. Stedman's Illustrated Medical Dictionary, 24th ed. Williams PL, Warwick R: Gray's Anatomy, 36th Baltimore: Williams and Wilkins, 1982. English edition. Philadelphia: Saunders, 1980. Weiss L, Greep ROO: Histology, 4th ed. New York: McGraw-Hill, 1977. Textbooks: Histology and Cytology Wheater PR, Burkitt HG, Daniels VG: Functional Arey LB: Human Histology, 4th ed. Philadelphia: Histology. Edinburgh: Churchill Livingstone, 1979. Saunders, 1974. Bloom W, Fawcett DW: A Textbook of Histology, Textbooks: Pathology 10th ed. Philadelphia: Saunders, 1974. Anderson WAD, Kissane JM: Pathology, 7th ed. Borysenko M, Borysenko J, Beringer T, Gustafson St. Louis: Mosby, 1977. A: Functional Histology. A Core Text. Boston: Lit tle, Brown, 1979. Anderson WAD, Scotti TM: Synopsis of Pathology, 10th ed. St. Louis: Mosby, 1980. Copenhaver WM, Kelly DE, Wood RL: Bailey's Golden A: Pathology. Understanding Human Dis Textbook of Histology, 17th ed. Baltimore: Wil ease. Baltimore: Williams and Wilkins, 1982. liams and Wilkins, 1978. King D, Geller LM, Krieger P, Silva F, Lefkowitch Cowdry EV: A Textbook of Histology, 4th ed. Phila JH: A Survey of Pathology. New York: Oxford delphia: Lea and Febiger, 1950. University Press, 1976. Dyson RD: Cell Biology. A Molecular Approach, Robbins SL, Cotran RS: Pathologic Basis of Dis 2nd ed. Boston: Allyn and Bacon, 1978. -

Histology of Female Reproductive System
Histology of Female Reproductive System Dr. Rajesh Ranjan Assistant Professor Deptt. of Veterinary Anatomy C.V.Sc., Rewa Female Reproductive System ▪Ovaries ▪Oviducts ▪Uterus ▪Vagina ▪Vulva Ovaries Ovoid structure divided into outer cortex and inner medulla. Cortex ( outer portion) ◦ Broad peripheral zone containing follicles in various stages of development embedded in loose connective tissue stroma and covered by Germinal epithelium which is Simple cuboidal/ columnar (young) and low cuboidal/ squamous (adult). ◦ Stroma: supporting tissue and covered by Tunica albuginea just beneath the germinal epithelium. Medulla (Inner portion) ◦ Contains nerves, blood vessels, lymphatics, loose connective tissue and smooth muscles. ◦ Also contains rete ovarii which is a solid cellular cords or networks of irregular channels lined by cuboidal epithelium. Ovarian Follicles Primordial follicle: ◦ Unilaminar, preantral, resting follicle. ◦ Comprises of primary oocyte surrounded by simple squamous epithelium. Primary follicle: ◦ Unilaminar, preantral, growing follicle. ◦ Comprises of primary oocyte surrounded by simple cuboidal epithelium. Early Secondary follicle: ◦ Multilaminar, preantral, growing follicle. ◦ Comprises of primary oocyte surrounded zona pellucida and stratified epithelium of polyhedral/ follicular cells called as Granulosa cell. ◦ Zona pellucida is a glycoprotein layer. Late Secondary follicle: • Multilaminar, antral, growing follicle. • Comprises of primary oocyte surrounded by zona pellucida and stratified epithelium of polyhedral/ follicular cells called as Granulosa cell (Zona Granulosa) with an outer covering of theca interna. • Antral pockets are formed containing liquor folliculi. • Theca layer (Theca interna) comprises of vascularized multilaminar layer of spindle shaped stroma cells. Graafian follicle: Also calledVesicular/ Tertiary follicle. Multilaminar, antral, growing follicle. Comprises of primary oocyte surrounded by Zona pellucida, Granulosa cells (Stratum granulosum) with Antrum and Theca layers. -

Review an Oocentric View of Folliculogenesis and Embryogenesis
RBMOnline - Vol 14. No 6. 2007 758-764 Reproductive BioMedicine Online; www.rbmonline.com/Article/2772 on web 26 April 2007 Review An oocentric view of folliculogenesis and embryogenesis Karla J Hutt conducted her graduate studies, which focused on receptor-ligand interactions and female gamete biology, at the Australian National University in Canberra. She was awarded her PhD degree in 2006 and is now at the University of Kansas Medical Center where she is a post-doctoral fellow under the supervision of David F Albertini. Dr Hutt’s research interests include using confocal imaging techniques to understand the characteristics of meiotic spindle assembly, dynamics and integrity of in-vitro matured and cryopreserved oocytes. Karla J Hutt, David F Albertini1 The Center for Reproductive Sciences, Molecular and Integrative Physiology, University of Kansas Medical Centre, 3901 Rainbow Boulevard, Kansas City, KS 66160, USA 1Correspondence: Tel: +11 913 588 0412; Fax: +11 913 588 0456; e-mail: [email protected] Abstract The mammalian oocyte undertakes a highly complex journey to maturity during which it successively acquires a series of characteristics necessary for fertilization and the development of a healthy embryo. While the contribution of granulosa cells to oocyte development has been studied for many years, it has recently become apparent that the oocyte itself plays a key role in directing its own fate as well as the growth and differentiation of the follicle. This regulatory capacity is achieved through the synthesis and secretion of oocyte-specifi c factors, such as growth and differentiation factor 9 and bone morphogenetic protein 15, which act on granulosa cells to modify their proliferation, function and differentiation, as well as through direct physical contacts that occur at the granulosa cell–oocyte interface. -
Endometrium and Released
FEMALE REPRODUCTIVE SYSTEM The female reproductive system consist of bilateral located ovarium, oviduct, uterus, cervix, vagina and vulva. This system; • Haploid gametes (ovum) produce. • It provides a convenient environment for fertilization. • It secretes hormones necessary for the implantation of the embryo and allows the development until birth. • It secretes hormones that regulate the reproductive cycle. OVARIUM: The ovaries produce and release oocytes into the female reproductive tract and effect on other organs of the reproductive system with hormones secreted and regulate the genital cycle. • Two major groups of steroid hormones, estrogens, and progestogens, are secreted by the ovaries. • The releasing to the genital canal of the ovum is an exocrine function of the ovarium. • Producing its own hormones also constitutes endocrine functions. • Oval or bean-shaped. The hilus which is the place the entry and exit of vessels and nerves hold the pelvic wall and uterus with some ties and connective tissue called mesovarium. • Mesovarium is covered with of visceral peritoneum (mesothelium and connective tissue). • The ovaries of all mammals have a similar basic structure. • It is composed of a cortex and a medulla. • Medulla located in the central portion of the ovary and contains loose connective tissue. • The cortex contains the ovarian follicles embedded in a richly cellular connective tissue. • The surface of the ovarium is covered by a single layer of cuboidal and, in some parts, almost squamous cells. • This cellular layer, known as the germinal epithelium, is continuous with the mesothelium that covers the mesovarium. • The ovarium has two parts: the cortex and the medulla. • The cortex is located outside the ovarium. -

Newly Identified Regulators of Ovarian Folliculogenesis and Ovulation
International Journal of Molecular Sciences Review Newly Identified Regulators of Ovarian Folliculogenesis and Ovulation Eran Gershon 1 and Nava Dekel 2,* 1 Department of Ruminant Science, Agricultural Research Organization, PO Box 6, Rishon LeZion 50250, Israel; [email protected] 2 Department of Biological Regulation, Weizmann Institute of Science, Rehovot 76100, Israel * Correspondence: [email protected] Received: 7 May 2020; Accepted: 23 June 2020; Published: 26 June 2020 Abstract: Each follicle represents the basic functional unit of the ovary. From its very initial stage of development, the follicle consists of an oocyte surrounded by somatic cells. The oocyte grows and matures to become fertilizable and the somatic cells proliferate and differentiate into the major suppliers of steroid sex hormones as well as generators of other local regulators. The process by which a follicle forms, proceeds through several growing stages, develops to eventually release the mature oocyte, and turns into a corpus luteum (CL) is known as “folliculogenesis”. The task of this review is to define the different stages of folliculogenesis culminating at ovulation and CL formation, and to summarize the most recent information regarding the newly identified factors that regulate the specific stages of this highly intricated process. This information comprises of either novel regulators involved in ovarian biology, such as Ube2i, Phoenixin/GPR73, C1QTNF, and α-SNAP, or recently identified members of signaling pathways previously reported in this context, namely PKB/Akt, HIPPO, and Notch. Keywords: folliculogenesis; ovulation 1. Folliculogenesis Folliculogenesis is initiated during fetal life. The migration of the primordial germ cells (PGCs) to the embryonic genital ridge [1] may, in fact, be considered as the earliest event along this process. -

A Comparative Analysis of Oocyte Development in Mammals
cells Review A Comparative Analysis of Oocyte Development in Mammals Rozenn Dalbies-Tran 1,*, Véronique Cadoret 1,2, Alice Desmarchais 1,Sébastien Elis 1 , Virginie Maillard 1, Philippe Monget 1, Danielle Monniaux 1 , Karine Reynaud 1, Marie Saint-Dizier 1 and Svetlana Uzbekova 1 1 INRAE, CNRS, Université de Tours, IFCE, PRC, F-37380 Nouzilly, France 2 CHU Bretonneau, Médecine et Biologie de la Reproduction-CECOS, 37044 Tours, France * Correspondence: [email protected] Received: 14 February 2020; Accepted: 9 April 2020; Published: 17 April 2020 Abstract: Sexual reproduction requires the fertilization of a female gamete after it has undergone optimal development. Various aspects of oocyte development and many molecular actors in this process are shared among mammals, but phylogeny and experimental data reveal species specificities. In this chapter, we will present these common and distinctive features with a focus on three points: the shaping of the oocyte transcriptome from evolutionarily conserved and rapidly evolving genes, the control of folliculogenesis and ovulation rate by oocyte-secreted Growth and Differentiation Factor 9 and Bone Morphogenetic Protein 15, and the importance of lipid metabolism. Keywords: oocyte; mammals; evolution; gene expression; posttranscriptional control; Gdf9; Bmp15; lipids 1. Introduction Sexual reproduction requires the fertilization of a female gamete after it has undergone optimal development. In animals, oogenesis has been studied in organisms as diverse as insects, worms, amphibians and mammals. In the latter, the mouse has long been the model of choice to delineate the complex mechanisms that regulate oogenesis and to identify the major genes and molecular actors involved throughout the process. -

Oocyte Differentiation Is Genetically Dissociable from the Meiotic Program in Mice
Oocyte differentiation is genetically dissociable from the meiotic program in mice by Gregoriy A. Dokshin B.A. Biology and German Language and Literature Cornell University, 2007 SUBMITTED TO THE DEPARTMENT OF BIOLOGY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN BIOLOGY AT THE ARCHNES MASSACHUSETTS INSTITUTE OF TECHNOLOGY MASSACHUSETTS INSTITTE OF TECHNOLOGY FEBRUARY 2013 FEB 1 3 UBRARIES C 2013 Massachusetts Institute of Technology. All rights reserved. N Signature of Author: Department of Biology .A Certified by: L. David C. Page Professor of Biology Thesis Supervisor Accepted by: 61 exC Stephen P. Bell Professor of Biology Chair, Committee for Graduate Students 1 2 Oocyte differentiation is genetically dissociable from the meiotic program in mice by Gregoriy A. Dokshin Submitted to the Department of Biology on January 25, 2013 in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Biology ABSTRACT: Oogenesis is a developmental program by which a gametogenesis-competent germ cell becomes a fertilization-competent egg. During oogenesis, growth and differentiation of oocytes are closely coordinated with initiation and progression through meiosis. In mammals, the timing of meiotic initiation is sexually dimorphic, with only ovarian and not testicular germ cells initiating meiosis during fetal development. Consequentially, fetal meiotic initiation is thought to be prerequisite to subsequent growth and differentiation of the ovarian germ cell into a fully grown oocyte. Here I present evidence that meiotic initiation and prophase I are genetically separable from oocyte growth and differentiation, thereby, demonstrating that oogenesis consists of two independent processes under separate regulation. -

GLOSSARY of HISTOLOGICAL & MICRO-ANATOMICAL TERMS
GLOSSARY of HISTOLOGICAL & MICRO-ANATOMICAL TERMS Abbreviations: ( ) plural form in brackets • A. Arabic abb. abbreviation • c. circa (= about) • F. French adj. adjective • G. Greek • Ge. German cf. compare • L. Latin dim. diminutive • NA. Nomina anatomica q.v. which see • OF. Old French A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat.