Endometrium and Released
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Sexual Reproduction & the Reproductive System Visual
Biology 202: Sexual Reproduction & the Reproductive System 1) Label the diagram below. Some terms may be used more than once. Spermatozoa (N) Mitosis Spermatogonium (2N) Spermatids (N) Primary Oocyte (2N) Polar bodies (N) Ootid (N) Second polar body (N) Meiosis I Primary spermatocyte (2N) Oogonium (2N) Secondary oocyte (2N) Ovum (N) Secondary spermatocytes (2N) First polar body Meiosis II Source Lesson: Gametogenesis & Meiosis: Process & Differences 2) Label the diagram of the male reproductive system below. Seminal vesicle Testis Scrotum Pubic bone Penis Prostate gland Urethra Epididymis Vas deferens Bladder Source Lesson: Male Reproductive System: Structures, Functions & Regulation 3) Label the image below. Rectum Testis Ureter Bulbourethral gland Urethra Urinary bladder Pubic bone Penis Seminal vesicle Ductus deferens Epididymis Prostate gland Anus Source Lesson: Semen: Composition & Production 4) Label the structures below. Inner and outer lips of the vagina Mons pubis Vaginal opening Clitoris Anus Urethral opening Perineum Vulva Source Lesson: Female Reproductive System: Structures & Functions 5) Label the diagram below. Some terms may be used more than once. Clitoris Vulva Labia majora Labia minora Perineum Clitoral hood Vaginal opening Source Lesson: Female Reproductive System: Structures & Functions 6) Label the internal organs that make up the female reproductive system. Uterus Fallopian tubes Ovaries Cervix Vagina Endometrium Source Lesson: Female Reproductive System: Structures & Functions 7) Label the diagram below. LH Follicular -

Chapter 24 Primary Sex Organs = Gonads Produce Gametes Secrete Hormones That Control Reproduction Secondary Sex Organs = Accessory Structures
Anatomy Lecture Notes Chapter 24 primary sex organs = gonads produce gametes secrete hormones that control reproduction secondary sex organs = accessory structures Development and Differentiation A. gonads develop from mesoderm starting at week 5 gonadal ridges medial to kidneys germ cells migrate to gonadal ridges from yolk sac at week 7, if an XY embryo secretes SRY protein, the gonadal ridges begin developing into testes with seminiferous tubules the testes secrete androgens, which cause the mesonephric ducts to develop the testes secrete a hormone that causes the paramesonephric ducts to regress by week 8, in any fetus (XX or XY), if SRY protein has not been produced, the gondal ridges begin to develop into ovaries with ovarian follicles the lack of androgens causes the paramesonephric ducts to develop and the mesonephric ducts to regress B. accessory organs develop from embryonic duct systems mesonephric ducts / Wolffian ducts eventually become male accessory organs: epididymis, ductus deferens, ejaculatory duct paramesonephric ducts / Mullerian ducts eventually become female accessory organs: oviducts, uterus, superior vagina C. external genitalia are indeterminate until week 8 male female genital tubercle penis (glans, corpora cavernosa, clitoris (glans, corpora corpus spongiosum) cavernosa), vestibular bulb) urethral folds fuse to form penile urethra labia minora labioscrotal swellings fuse to form scrotum labia majora urogenital sinus urinary bladder, urethra, prostate, urinary bladder, urethra, seminal vesicles, bulbourethral inferior vagina, vestibular glands glands Strong/Fall 2008 Anatomy Lecture Notes Chapter 24 Male A. gonads = testes (singular = testis) located in scrotum 1. outer coverings a. tunica vaginalis =double layer of serous membrane that partially surrounds each testis; (figure 24.29) b. -
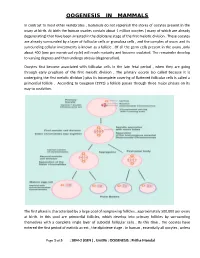
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

GROSS and HISTOMORPHOLOGY of the OVARY of BLACK BENGAL GOAT (Capra Hircus)
VOLUME 7 NO. 1 JANUARY 2016 • pages 37-42 MALAYSIAN JOURNAL OF VETERINARY RESEARCH RE# MJVR – 0006-2015 GROSS AND HISTOMORPHOLOGY OF THE OVARY OF BLACK BENGAL GOAT (Capra hircus) HAQUE Z.1*, HAQUE A.2, PARVEZ M.N.H.3 AND QUASEM M.A.1 1 Department of Anatomy and Histology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh-2202, Bangladesh 2 Chittagong Veterinary and Animal Sciences University, Khulshi, Chittagong 3 Department of Anatomy and Histology, Faculty of Veterinary and Animal Science, Hajee Mohammad Danesh Science and Technology University, Basherhat, Dinajpur * Corresponding author: [email protected] ABSTRACT. Ovary plays a vital 130.07 ± 12.53 µm and the oocyte diameter role in the reproductive biology and was 109.8 ± 5.75 µm. These results will be biotechnology of female animals. In this helpful to manipulate ovarian functions in study, both the right and left ovaries of small ruminants. the Black Bengal goat were collected from Keywords: Morphometry, ovarian the slaughter houses of different Thanas follicles, cortex, medulla, oocyte. in the Mymensingh district. For each of the specimens, gross parameters such as INTRODUCTION weight, length and width were recorded. Then they were processed and stained with Black Bengal goat is the national pride of H&E for histomorphometry. This study Bangladesh. The most promising prospect revealed that the right ovary (0.53 ± 0.02 of Black Bengal goat in Bangladesh is g) was heavier than the left (0.52 ± 0.02 g). that this dwarf breed is a prolific breed, The length of the right ovary (1.26 ± 0.04 requiring only a small area to breed and cm) was lower than the left (1.28 ± 0.02 with the advantage of their selective cm) but the width of the right (0.94 ± 0.02 feeding habit with a broader feed range. -

Morphometric and Gene Expression Analyses of Stromal Expansion During Development of the Bovine Fetal Ovary', Reproduction, Fertility and Development
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Edinburgh Research Explorer Edinburgh Research Explorer Morphometric and gene expression analyses of stromal expansion during development of the bovine fetal ovary Citation for published version: Hartanti, MD, Hummitzsch, K, Irving-rodgers, HF, Bonner, WM, Copping, KJ, Anderson, RA, Mcmillen, IC, Perry, VEA & Rodgers, RJ 2018, 'Morphometric and gene expression analyses of stromal expansion during development of the bovine fetal ovary', Reproduction, Fertility and Development. https://doi.org/10.1071/RD18218 Digital Object Identifier (DOI): 10.1071/RD18218 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Reproduction, Fertility and Development General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 11. May. 2020 CSIRO PUBLISHING Reproduction, Fertility and Development https://doi.org/10.1071/RD18218 Morphometric and gene expression analyses of stromal expansion during development of the bovine fetal ovary M. D. HartantiA, K. HummitzschA, H. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Development of Mammalian Ovary
P SMITH and others Development of mammalian 221:3 R145–R161 Review ovary Development of mammalian ovary Peter Smith1,2, Dagmar Wilhelm3 and Raymond J Rodgers4 1AgResearch Invermay, Puddle Alley, Mosgiel 9053, New Zealand Correspondence 2Department of Anatomy, University of Otago, Dunedin 9054, New Zealand should be addressed 3Department of Anatomy and Developmental Biology, Monash University, Clayton, Victoria 3800, Australia to P Smith 4Robinson Research Institute, Discipline of Obstetrics and Gynaecology, School of Paediatrics and Reproductive Email Health, University of Adelaide, Adelaide, South Australia 5005, Australia [email protected] Abstract Pre-natal and early post-natal ovarian development has become a field of increasing Key Words importance over recent years. The full effects of perturbations of ovarian development on " ovary adult fertility, through environmental changes or genetic anomalies, are only now being " fetus truly appreciated. Mitigation of these perturbations requires an understanding of the " development processes involved in the development of the ovary. Herein, we review some recent findings " polycystic ovary syndrome from mice, sheep, and cattle on the key events involved in ovarian development. We discuss " premature ovary failure the key process of germ cell migration, ovigerous cord formation, meiosis, and follicle formation and activation. We also review the key contributions of mesonephric cells to ovarian development and propose roles for these cells. Finally, we discuss polycystic ovary syndrome, premature ovarian failure, and pre-natal undernutrition; three key areas in which perturbations to ovarian development appear to have major effects on post-natal fertility. Journal of Endocrinology (2014) 221, R145–R161 Journal of Endocrinology Introduction The developmental origins of health and disease are an development, bringing together the commonly accepted area of increasing research. -

Uterus – Dilation
Uterus – Dilation Figure Legend: Figure 1 Uterus - Dilation of the uterine lumen in a female B6C3F1/N mouse from a chronic study. There is dilation of the uterine horn. Figure 2 Uterus - Dilation in a female B6C3F1/N mouse from a chronic study (higher magnification of Figure 1). The endometrial epithelium is cuboidal. Figure 3 Uterus - Dilation in a female B6C3F1/N mouse from a chronic study. There is dilation of the uterine lumen, which contains flocculent, eosinophilic material. Figure 4 Uterus - Dilation in a female B6C3F1/N mouse from a chronic study (higher magnification of Figure 3). There is flattened epithelium and eosinophilic material in the uterine lumen. Comment: Dilation of uterine horns (Figure 1, Figure 2, Figure 3, and Figure 4) is commonly observed at necropsy, and frequently these uteri have accumulations of excessive amounts of fluid within the 1 Uterus – Dilation lumen. Uterine dilation is relatively commonly seen in both rats and mice and may be segmental. Luminal dilation may be associated with stromal polyps or occur secondarily to hormonal imbalances from ovarian cysts or to a prolonged estrus state after cessation of the estrus cycle in aged rodents. Administration of progestins, estrogens, and tamoxifen in rats has been associated with uterine dilation. Luminal dilation is normally observed at proestrus and estrus in cycling rodents and should not be diagnosed. Increased serous fluid production is part of the proestrus phase of the cycle judged by the vaginal epithelium (which shows early keratinization covered by a layer of mucified cells) and should not be diagnosed. With uterine dilation, the endometrial lining is usually attenuated or atrophic and the wall of the uterus thinned due to the increasing pressure, but in less severe cases the endometrium can be normal (Figure 2). -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model. -

The Functions of Uterine Secretions R
Printed in Great Britain J. Reprod. Fert. (1988) 82,875-892 @ 1988 Journals of Reproduction & Fertility Ltd The functions of uterine secretions R. M. Roberts and F. W. Bazer Departments of Biochemistry and Animal Sciences, University of Missouri, Columbia, MO 65211, U.S.A.; and Department of Animal Science, University of Florida, Gainesville, FL 32611, U.S.A. Summary. The likely functions of uterine secretions, often termed histotroph, in the nurture of the early conceptus are reviewed. Particular emphasis has been placed on the pig in which the uterus synthesizes and secretes large amounts of protein in response to progesterone. In this species, which possesses a non-invasive, diffuse type of epithelio- chorial placentation, the secretions provide a sustained embryotrophic environment which is distinct from that of serum. A group of basic proteins dominates these uterine secretions after Day 1 1 of pregnancy and its best characterized member is uteroferrin, an iron-containing acid phosphatase with a deep purple colour. Evidence has accumulated to suggest that uteroferrin, rather than functioning as an acid phosphatase, is involved in transporting iron to the conceptus. Three basic polypeptides which are found non- covalently associated with uteroferrin have been shown to be antigenically closely related to one another and to have arisen by post-translational processing from a common precursor molecule. Their function is unknown. A group of basic protease inhibitors has been identified which bear considerable sequence homology to bovine pancreatic trypsin inhibitor (aprotinin) and may control intrauterine proteolytic events initiated by the conceptuses. The last basic protein so far characterized is lysozyme which is presumed to have an antibacterial role. -

Female Reproductive System & Regulation of Ovarian Function
1 ONPRC Module 1B: Female Reproductive System & Regulation of Ovarian Function Guiding Question: How does the female reproductive system work? Module Question Laboratory Questions • How does a scientist obtain ovaries for a study? What are the important • How do researchers look at follicle morphology? parts of the female • How does female reproductive anatomy differ between reproductive system, mammalian species (mice, humans, monkeys, sheep, and how does the horses, cats, dogs)? • What can female reproductive anatomy tell us about menstrual cycle work? pregnancy in the different species? Learning Outcomes: Identify female reproductive anatomical structures of different species (mice, humans, monkeys, sheep, horses, cats, dogs). Explain the ovarian cycle (process of follicular development, ovulation, corpus luteum formation). Explain the menstrual cycle (changes that occur in the uterus under the influence of ovarian hormones). Define the source and function of hormones involved in the female reproductive system. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. 2 Additional Reproductive Vocabulary Gamete: a haploid sex cell called the oocyte in females and a sperm in males Gametogenesis – one of the two major functions of the follicle in the ovary and the stem cells in the testes and the process by which precursor cells undergo meiotic cell division and differentiation to form the mature haploid gametes. In the ovary the oocyte and in the testes the sperm form as a result of gametogenesis. Zygote: diploid cell formed by the union of sperm and oocyte; the product of fertilization Hormone – a chemical messenger that carries information from one cell to another via the bloodstream.