Part 3: Female Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ovarian Cancer and Cervical Cancer
What Every Woman Should Know About Gynecologic Cancer R. Kevin Reynolds, MD The George W. Morley Professor & Chief, Division of Gyn Oncology University of Michigan Ann Arbor, MI What is gynecologic cancer? Cancer is a disease where cells grow and spread without control. Gynecologic cancers begin in the female reproductive organs. The most common gynecologic cancers are endometrial cancer, ovarian cancer and cervical cancer. Less common gynecologic cancers involve vulva, Fallopian tube, uterine wall (sarcoma), vagina, and placenta (pregnancy tissue: molar pregnancy). Ovary Uterus Endometrium Cervix Vagina Vulva What causes endometrial cancer? Endometrial cancer is the most common gynecologic cancer: one out of every 40 women will develop endometrial cancer. It is caused by too much estrogen, a hormone normally present in women. The most common cause of the excess estrogen is being overweight: fat cells actually produce estrogen. Another cause of excess estrogen is medication such as tamoxifen (often prescribed for breast cancer treatment) or some forms of prescribed estrogen hormone therapy (unopposed estrogen). How is endometrial cancer detected? Almost all endometrial cancer is detected when a woman notices vaginal bleeding after her menopause or irregular bleeding before her menopause. If bleeding occurs, a woman should contact her doctor so that appropriate testing can be performed. This usually includes an endometrial biopsy, a brief, slightly crampy test, performed in the office. Fortunately, most endometrial cancers are detected before spread to other parts of the body occurs Is endometrial cancer treatable? Yes! Most women with endometrial cancer will undergo surgery including hysterectomy (removal of the uterus) in addition to removal of ovaries and lymph nodes. -

In Hardening of the Zona Pellucida K
Disulfide formation in bovine zona pellucida glycoproteins during fertilization: evidence for the involvement of cystine cross-linkages in hardening of the zona pellucida K. Kwamoto, K. Ikeda, N. Yonezawa, S. Noguchi, K. Kudo, S. Hamano, M. Kuwayama and M. Nakano department ofChemistry, Faculty ofScience and 2Graduate School ofScience and Technology, Chiba University, 1-33 Yayoi-cho, Inage-ku, Chiba 263-8522, Japan; and3Animal Bio-Technology Center, Livestock Improvement Association, Tokyo, Japan The time for solubilization of the bovine zona pellucida in a hypotonic buffer containing 5% (v/v) \g=b\-mercaptoethanoland 7 mol urea l\m=-\1 increased by 10% after fertilization. Coupling with a specific fluorescent thiol probe, monobromobimane (mBBr), was markedly greater in the zona pellucida of ovarian eggs compared with fertilized eggs, indicating that the cysteine residues in the zona pellucida of unfertilized eggs are oxidized to cystines during fertilization. After endo-\g=b\-galactosidasedigestion to remove N-acetyllactosamine repeats of the carbohydrate chains, three zona pellucida glycoproteins (ZPA, ZPB and ZPC) coupled with the fluorescent bimane groups were fractionated efficiently by reverse-phase HPLC. Estimation of bimane groups in the three components and SDS-PAGE revealed that intramolecular disulfide bonds in ZPA and intra- and intermolecular disulfide bonds in ZPB were formed during fertilization, but oxidation of cysteine residues in ZPC was low. Specific proteolysis of ZPA during fertilization was also observed. These results indicate that the formation of disulfide linkages together with specific proteolysis result in the construction of a rigid zona pellucida structure, which is responsible for hardening of the zona pellucida. Introduction cross-linkages between tyrosine residues of the zona pellucida proteins formed by ovoperoxidase caused the The zona is one of the two sites at which pellucida In contrast to sea urchins (Foerder and is blocked and hardening. -
Chapter 28 *Lecture Powepoint
Chapter 28 *Lecture PowePoint The Female Reproductive System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • The female reproductive system is more complex than the male system because it serves more purposes – Produces and delivers gametes – Provides nutrition and safe harbor for fetal development – Gives birth – Nourishes infant • Female system is more cyclic, and the hormones are secreted in a more complex sequence than the relatively steady secretion in the male 28-2 Sexual Differentiation • The two sexes indistinguishable for first 8 to 10 weeks of development • Female reproductive tract develops from the paramesonephric ducts – Not because of the positive action of any hormone – Because of the absence of testosterone and müllerian-inhibiting factor (MIF) 28-3 Reproductive Anatomy • Expected Learning Outcomes – Describe the structure of the ovary – Trace the female reproductive tract and describe the gross anatomy and histology of each organ – Identify the ligaments that support the female reproductive organs – Describe the blood supply to the female reproductive tract – Identify the external genitalia of the female – Describe the structure of the nonlactating breast 28-4 Sexual Differentiation • Without testosterone: – Causes mesonephric ducts to degenerate – Genital tubercle becomes the glans clitoris – Urogenital folds become the labia minora – Labioscrotal folds -

About Ovarian Cancer Overview and Types
cancer.org | 1.800.227.2345 About Ovarian Cancer Overview and Types If you have been diagnosed with ovarian cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is Ovarian Cancer? Research and Statistics See the latest estimates for new cases of ovarian cancer and deaths in the US and what research is currently being done. ● Key Statistics for Ovarian Cancer ● What's New in Ovarian Cancer Research? What Is Ovarian Cancer? Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer and can spread. To learn more about how cancers start and spread, see What Is Cancer?1 Ovarian cancers were previously believed to begin only in the ovaries, but recent evidence suggests that many ovarian cancers may actually start in the cells in the far (distal) end of the fallopian tubes. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 What are the ovaries? Ovaries are reproductive glands found only in females (women). The ovaries produce eggs (ova) for reproduction. The eggs travel from the ovaries through the fallopian tubes into the uterus where the fertilized egg settles in and develops into a fetus. The ovaries are also the main source of the female hormones estrogen and progesterone. One ovary is on each side of the uterus. The ovaries are mainly made up of 3 kinds of cells. Each type of cell can develop into a different type of tumor: ● Epithelial tumors start from the cells that cover the outer surface of the ovary. -

Reproductive System, Day 2 Grades 4-6, Lesson #12
Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Reproductive System, day 2 Grades 4-6, Lesson #12 Time Needed 40-50 minutes Student Learning Objectives To be able to... 1. Distinguish reproductive system facts from myths. 2. Distinguish among definitions of: ovulation, ejaculation, intercourse, fertilization, implantation, conception, circumcision, genitals, and semen. 3. Explain the process of the menstrual cycle and sperm production/ejaculation. Agenda 1. Explain lesson’s purpose. 2. Use transparencies or your own drawing skills to explain the processes of the male and female reproductive systems and to answer “Anonymous Question Box” questions. 3. Use Reproductive System Worksheets #3 and/or #4 to reinforce new terminology. 4. Use Reproductive System Worksheet #5 as a large group exercise to reinforce understanding of the reproductive process. 5. Use Reproductive System Worksheet #6 to further reinforce Activity #2, above. This lesson was most recently edited August, 2009. Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 1 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. Materials Needed Classroom Materials: OPTIONAL: Reproductive System Transparency/Worksheets #1 – 2, as 4 transparencies (if you prefer not to draw) OPTIONAL: Overhead projector Student Materials: (for each student) Reproductive System Worksheets 3-6 (Which to use depends upon your class’ skill level. Each requires slightly higher level thinking.) Public Health - Seattle & King County • Family Planning Program • © 1986 • revised 2009 • www.kingcounty.gov/health/flash 12 - 2 Family Life and Sexual Health, Grades 4, 5 and 6, Lesson 12 F.L.A.S.H. -

Chapter 24 Primary Sex Organs = Gonads Produce Gametes Secrete Hormones That Control Reproduction Secondary Sex Organs = Accessory Structures
Anatomy Lecture Notes Chapter 24 primary sex organs = gonads produce gametes secrete hormones that control reproduction secondary sex organs = accessory structures Development and Differentiation A. gonads develop from mesoderm starting at week 5 gonadal ridges medial to kidneys germ cells migrate to gonadal ridges from yolk sac at week 7, if an XY embryo secretes SRY protein, the gonadal ridges begin developing into testes with seminiferous tubules the testes secrete androgens, which cause the mesonephric ducts to develop the testes secrete a hormone that causes the paramesonephric ducts to regress by week 8, in any fetus (XX or XY), if SRY protein has not been produced, the gondal ridges begin to develop into ovaries with ovarian follicles the lack of androgens causes the paramesonephric ducts to develop and the mesonephric ducts to regress B. accessory organs develop from embryonic duct systems mesonephric ducts / Wolffian ducts eventually become male accessory organs: epididymis, ductus deferens, ejaculatory duct paramesonephric ducts / Mullerian ducts eventually become female accessory organs: oviducts, uterus, superior vagina C. external genitalia are indeterminate until week 8 male female genital tubercle penis (glans, corpora cavernosa, clitoris (glans, corpora corpus spongiosum) cavernosa), vestibular bulb) urethral folds fuse to form penile urethra labia minora labioscrotal swellings fuse to form scrotum labia majora urogenital sinus urinary bladder, urethra, prostate, urinary bladder, urethra, seminal vesicles, bulbourethral inferior vagina, vestibular glands glands Strong/Fall 2008 Anatomy Lecture Notes Chapter 24 Male A. gonads = testes (singular = testis) located in scrotum 1. outer coverings a. tunica vaginalis =double layer of serous membrane that partially surrounds each testis; (figure 24.29) b. -
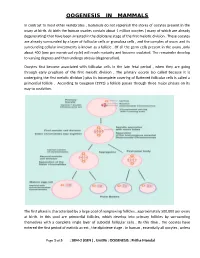
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

FEMALE REPRODUCTIVE SYSTEM Female Reproduc�Ve System
Human Anatomy Unit 3 FEMALE REPRODUCTIVE SYSTEM Female Reproducve System • Gonads = ovaries – almond shaped – flank the uterus on either side – aached to the uterus and body wall by ligaments • Gametes = oocytes – released from the ovary during ovulaon – Develop within ovarian follicles Ligaments • Broad ligament – Aaches to walls and floor of pelvic cavity – Connuous with parietal peritoneum • Round ligament – Perpendicular to broad ligament • Ovarian ligament – Lateral surface of uterus ‐ ‐> medial surface of ovary • Suspensory ligament – Lateral surface of ovary ‐ ‐> pelvic wall Ovarian Follicles • Layers of epithelial cells surrounding ova • Primordial follicle – most immature of follicles • Primary follicle – single layer of follicular (granulosa) cells • Secondary – more than one layer and growing cavies • Graafian – Fluid filled antrum – ovum supported by many layers of follicular cells – Ovum surrounded by corona radiata Ovarian Follicles Corpus Luteum • Ovulaon releases the oocyte with the corona radiata • Leaves behind the rest of the Graafian follicle • Follicle becomes corpus luteum • Connues to secrete hormones to support possible pregnancy unl placenta becomes secretory or no implantaon • Becomes corpus albicans when no longer funconal Corpus Luteum and Corpus Albicans Uterine (Fallopian) Tubes • Ciliated tubes – Passage of the ovum to the uterus and – Passage of sperm toward the ovum • Fimbriae – finger like projecons that cover the ovary and sway, drawing the ovum inside aer ovulaon The Uterus • Muscular, hollow organ – supports -

GROSS and HISTOMORPHOLOGY of the OVARY of BLACK BENGAL GOAT (Capra Hircus)
VOLUME 7 NO. 1 JANUARY 2016 • pages 37-42 MALAYSIAN JOURNAL OF VETERINARY RESEARCH RE# MJVR – 0006-2015 GROSS AND HISTOMORPHOLOGY OF THE OVARY OF BLACK BENGAL GOAT (Capra hircus) HAQUE Z.1*, HAQUE A.2, PARVEZ M.N.H.3 AND QUASEM M.A.1 1 Department of Anatomy and Histology, Faculty of Veterinary Science, Bangladesh Agricultural University, Mymensingh-2202, Bangladesh 2 Chittagong Veterinary and Animal Sciences University, Khulshi, Chittagong 3 Department of Anatomy and Histology, Faculty of Veterinary and Animal Science, Hajee Mohammad Danesh Science and Technology University, Basherhat, Dinajpur * Corresponding author: [email protected] ABSTRACT. Ovary plays a vital 130.07 ± 12.53 µm and the oocyte diameter role in the reproductive biology and was 109.8 ± 5.75 µm. These results will be biotechnology of female animals. In this helpful to manipulate ovarian functions in study, both the right and left ovaries of small ruminants. the Black Bengal goat were collected from Keywords: Morphometry, ovarian the slaughter houses of different Thanas follicles, cortex, medulla, oocyte. in the Mymensingh district. For each of the specimens, gross parameters such as INTRODUCTION weight, length and width were recorded. Then they were processed and stained with Black Bengal goat is the national pride of H&E for histomorphometry. This study Bangladesh. The most promising prospect revealed that the right ovary (0.53 ± 0.02 of Black Bengal goat in Bangladesh is g) was heavier than the left (0.52 ± 0.02 g). that this dwarf breed is a prolific breed, The length of the right ovary (1.26 ± 0.04 requiring only a small area to breed and cm) was lower than the left (1.28 ± 0.02 with the advantage of their selective cm) but the width of the right (0.94 ± 0.02 feeding habit with a broader feed range. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Luteal Phase Deficiency: What We Now Know
■ OBGMANAGEMENT BY LAWRENCE ENGMAN, MD, and ANTHONY A. LUCIANO, MD Luteal phase deficiency: What we now know Disagreement about the cause, true incidence, and diagnostic criteria of this condition makes evaluation and management difficult. Here, 2 physicians dissect the data and offer an algorithm of assessment and treatment. espite scanty and controversial sup- difficult to definitively diagnose the deficien- porting evidence, evaluation of cy or determine its incidence. Further, while Dpatients with infertility or recurrent reasonable consensus exists that endometrial pregnancy loss for possible luteal phase defi- biopsy is the most reliable diagnostic tool, ciency (LPD) is firmly established in clinical concerns remain about its timing, repetition, practice. In this article, we examine the data and interpretation. and offer our perspective on the role of LPD in assessing and managing couples with A defect of corpus luteum reproductive disorders (FIGURE 1). progesterone output? PD is defined as endometrial histology Many areas of controversy Linconsistent with the chronological date of lthough observational and retrospective the menstrual cycle, based on the woman’s Astudies have reported a higher incidence of LPD in women with infertility and recurrent KEY POINTS 1-4 pregnancy losses than in fertile controls, no ■ Luteal phase deficiency (LPD), defined as prospective study has confirmed these find- endometrial histology inconsistent with the ings. Furthermore, studies have failed to con- chronological date of the menstrual cycle, may be firm the superiority of any particular therapy. caused by deficient progesterone secretion from the corpus luteum or failure of the endometrium Once considered an important cause of to respond appropriately to ovarian steroids. -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model.