A Comparative Analysis of Oocyte Development in Mammals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
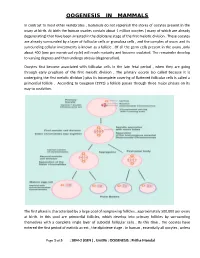
Oogenesis in Mammals
OOGENESIS IN MAMMALS In contrast to most other vertebrates , mammals do not replenish the stores of oocytes present in the ovary at birth. At birth the human ovaries contain about 1 million oocytes ( many of which are already degenerating) that have been arrested in the diplotene stage of the first meiotic division . These oocytes are already surrounded by a layer of follicular cells or granulosa cells , and the complex of ovum and its surrounding cellular investments is known as a follicle . Of all the germ cells present in the ovary ,only about 400 (one per menstrual cycle) will reach maturity and become ovulated. The remainder develop to varying degrees and then undergo atresia (degeneration). Oocytes first become associated with follicular cells in the late fetal period , when they are going through early prophase of the first meiotic division . The primary oocyte (so called because it is undergoing the first meiotic division ) plus its incomplete covering of flattened follicular cells is called a primordial follicle . According to Gougeon (1993) a follicle passes through three major phases on its way to ovulation. The first phase is characterized by a large pool of nongrowing follicles , approximately 500,000 per ovary at birth. In this pool are primordial follicles, which develop into primary follicles by surrounding themselves with a complete single layer of cuboidal follicular cells . By this time , the oocytes have entered the first period of meiotic arrest , the diplotene stage . In human , essentially all oocytes , unless Page 1 of 5 : SEM-2 (GEN ) , Unit#6 : OOGENESIS : Pritha Mondal they degenerate ,remain arrested in the diplotene stage until puberty ; some will not progress past the diplotene stage until the woman’s last reproductive cycle (age 45 to 55 years). -

Effect of Paternal Age on Aneuploidy Rates in First Trimester Pregnancy Loss
Journal of Medical Genetics and Genomics Vol. 2(3), pp. 38-43, August 2010 Available online at http://www.academicjournals.org/jmgg ©2010 Academic Journals Full Length Research Paper Effect of paternal age on aneuploidy rates in first trimester pregnancy loss Vitaly A. Kushnir, Richard T. Scott and John L. Frattarelli 1Department of Obstetrics, Gynecology and Women’s Health, New Jersey Medical School, MSB E-506, 185 South Orange Avenue, Newark, NJ, 07101-1709, USA. 2Department of Obstetrics, Gynecology and Reproductive Sciences, Robert Wood Johnson Medical School UMDNJ, Division of Reproductive Endocrinology and Infertility, New Brunswick, NJ. Reproductive Medicine Associates of New Jersey, Morristown NJ, USA. Accepted 16 July, 2010 A retrospective cohort analysis of patients undergoing IVF cycles at an academic IVF center was performed to test the hypothesis that male age may influence aneuploidy rates in first trimester pregnancy losses. All patients had a first trimester pregnancy loss followed by evacuation of the pregnancy and karyotyping of the abortus. Couples undergoing anonymous donor oocyte ART cycles (n = 50) and 23 couples with female age less than 30 years undergoing autologous oocyte ART cycles were included. The oocyte age was less than 30 in both groups; thereby allowing the focus to be on the reproductive potential of the aging male. The main outcome measure was the effect of paternal age on aneuploidy rate. No increase in aneuploidy rate was noted with increasing paternal age (<40 years = 25.0%; 40-50 years = 38.8%; >50 years = 25.0%). Although there was a significant difference in the male partner age between oocyte recipients and young patients using autologous oocytes (33.7 7.6 vs. -
Gametogenesis: Spermatogenesis & Oogenesis -Structure of Sperm and Egg Fertilization
Gametogenesis: Spermatogenesis & Oogenesis ‐Structure of Sperm and Egg Fertilization ‐ Definition, Mechanism Early development in Frog ‐ Cleavage, Blas tu la, GtlGastrula, DitiDerivatives of Germ layers Vikasana - CET 2012 y Human reproduction y Brief Account of Fertilization: Implantation, Placenta, Role of Gonadotropins and sex hormones , Menstrual cycle. y Fertility Control: Family Planning Methods- y Infertility Control: Meaning, Causes,Treatment y STD: AIDS , Syphilis and Gonorrhea Vikasana - CET 2012 1.Primary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 2.Secondary Oocyte is a) Haploid (n) b) Diploid (2n) c) Polyploid d) None of the above Vikasana - CET 2012 3.Centrioles of sperm control a) Movement of tail b) Hap lo id numb er of ch romosomes c) Help in fertilization d) None of the above. Vikasana - CET 2012 4.The Fertilization membrane is secreted because a) It checks the entry of more sperms after fertilization b) it checks the entry of antigens in ovum c))p it represents the left out tail of the sperm d) it represen tVikasanas the p - l CETasma 2012 mem brane of the sperm 5.Meiosis I occurs in a) Primary spermatocytes b) Secondary spermatocytes c) Both a and b d) Spermatogonia Vikasana - CET 2012 6.Meiosis II occurs in a) Secondary oocyte b))y Primary oocyte c) Spermatogonia d) Oogonia Vikasana - CET 2012 7.Axial filament of sperm is formed by a) Distal centriole b) Prox ima l centitrio le c) Mitochondria d) DNA Vikasana - CET 2012 8.Polar bodies are formed during a) oogenesis -

Anatomy of Male Reproductive System
Reproductive System Anatomy of Male Reproductive System Function: producing offspring Major Organs propagation of the species External Reproductive Organs !in terms of evolution penis and scrotum – the only reason all the other systems exist Internal Organs: only major system that doesn’t work continuously ! only activated at puberty these structures form continuous tube: unlike most other organisms on planet Testes ! mammals only reproduce sexually epididymus humans are dieocious vas deferens ! separate sexed (many animals are monoecious or ejaculatory duct hermaphrodites) urethra in penis th in 7 week of embryonic development genes are activated that trigger differentiation of gonads Accessory organs seminal vesicles prostate gland bulbourethral glands 1. Penis and Scrotum penis is transfer organ glans ! expanded head prepuce ! foreskin both have modified sebaceous glands that produce waxy secretion = smegma Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 1 Human Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2013.4 2 a. seminiferous tubules penis contains erectile tissues that surrounds (700’ of seminiferous tubules in testes) the urethra ! functions in spermatogenesis: ! fill with blood during sexual arousal formation and maturation of sperm cells corpus spongiosum (lower – surrounds urethra) passes along ventral side of penis and in cross section: encloses urethra seminiferous tubules appear roughly circular and contain germinal epithelium 2 coropora cavernosum (upper) (containing germ cells) and sustentacular on dorsal side (Sertoli) cells Sertoli cells protect germ cells and promote all contain numerous tiny blood sinuses their development = lacunae b. interstitial cells scrotum keeps testes at cooler temperature are scattered between the seminiferous tubules ! sperm can only be produced at several degrees below function in hormone secretion normal body temp !testosterone 2. -
![Oogenesis [PDF]](https://docslib.b-cdn.net/cover/2902/oogenesis-pdf-452902.webp)
Oogenesis [PDF]
Oogenesis Dr Navneet Kumar Professor (Anatomy) K.G.M.U Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Development of ovum (oogenesis) • Maturation of follicle • Fate of ovum and follicle Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Oogenesis • Site – ovary • Duration – 7th week of embryo –primordial germ cells • -3rd month of fetus –oogonium • - two million primary oocyte • -7th month of fetus primary oocyte +primary follicle • - at birth primary oocyte with prophase of • 1st meiotic division • - 40 thousand primary oocyte in adult ovary • - 500 primary oocyte attain maturity • - oogenesis completed after fertilization Dr Navneet Kumar Dr NavneetKumar Professor Professor (Anatomy) Anatomy KGMU Lko K.G.M.U Development of ovum Oogonium(44XX) -In fetal ovary Primary oocyte (44XX) arrest till puberty in prophase of 1st phase meiotic division Secondary oocyte(22X)+Polar body(22X) 1st phase meiotic division completed at ovulation &enter in 2nd phase Ovum(22X)+polarbody(22X) After fertilization Dr NavneetKumar Professor Anatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Dr Navneet Kumar Dr ProfessorNavneetKumar (Anatomy) Professor K.G.M.UAnatomy KGMU Lko Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Dr NavneetKumar Professor Anatomy KGMU Lko Maturation of follicle Primordial follicle -Follicular cells Primary follicle -Zona pallucida -Granulosa cells Secondary follicle Antrum developed Ovarian /Graafian follicle - Theca interna &externa -Membrana granulosa -Antrial -

Regulation and Roles of the Hyaluronan System in Mammalian Reproduction
REPRODUCTIONREVIEW Regulation and roles of the hyaluronan system in mammalian reproduction Ali A Fouladi-Nashta1, Kabir A Raheem1,2, Waleed F Marei1,3, Fataneh Ghafari1 and Geraldine M Hartshorne4 1Royal Veterinary College, Reproduction Research Group, Hawkshead Campus, Hatfield, UK, 2Department of Veterinary Surgery and Theriogenology, Michael Okpara University of Agriculture, Umudike, Nigeria, 3Department of Theriogenology, Faculty of Veterinary Medicine, Cairo University, Giza, Egypt and 4Warwick Medical School, University of Warwick, Coventry, UK and Centre for Reproductive Medicine, University Hospitals Coventry and Warwickshire NHS Trust, Coventry, UK Correspondence should be addressed to A A Fouladi-Nashta; Email: [email protected] Abstract Hyaluronan (HA) is a non-sulphated glycosaminoglycan polymer naturally occurring in many tissues and fluids of mammals, including the reproductive system. Its biosynthesis by HA synthase (HAS1–3) and catabolism by hyaluronidases (HYALs) are affected by ovarian steroid hormones. Depending upon its molecular size, HA functions both as a structural component of tissues in the form of high-molecular-weight HA or as a signalling molecule in the form of small HA molecules or HA fragments with effects mediated through interaction with its specific cell-membrane receptors. HA is produced by oocytes and embryos and in various segments of the reproductive system. This review provides information about the expression and function of members of the HA system, including HAS, HYALs and HA receptors. We examine their role in various processes from folliculogenesis through oocyte maturation, fertilisation and early embryo development, to pregnancy and cervical dilation, as well as its application in assisted reproduction technologies. Particular emphasis has been placed upon the role of the HA system in pre-implantation embryo development and embryo implantation, for which we propose a hypothetical sequential model. -

Progression from Meiosis I to Meiosis II in Xenopus Oocytes Requires De
Proc. Natl. Acad. Sci. USA Vol. 88, pp. 5794-5798, July 1991 Biochemistry Progression from meiosis I to meiosis II in Xenopus oocytes requires de novo translation of the mosxe protooncogene (cell cycle/protein kinase/maturation-promoting factor/germinal vesicle breakdown) JOHN P. KANKI* AND DANIEL J. DONOGHUEt Department of Chemistry, Division of Biochemistry and Center for Molecular Genetics, University of California at San Diego, La Jolla, CA 92093-0322 Communicated by Russell F. Doolittle, March 22, 1991 ABSTRACT The meiotic maturation of Xenopus oocytes controlling entry into and exit from M phase (for reviews, see exhibits an early requirement for expression of the mosxe refs. 17-19). protooncogene. The mosxc protein has also been shown to be a In Xenopus, protein synthesis is required for the initiation component of cytostatic factor (CSF), which is responsible for of meiosis I and also meiosis II (4, 20), even though stage VI arrest at metaphase ofmeiosis II. In this study, we have assayed oocytes already contain both p34cdc2 and cyclin (12, 21). the appearance of CSF activity in oocytes induced to mature These proteins are partially complexed in an inactive form of either by progesterone treatment or by overexpression ofmosxe. MPF (preMPF) that appears to be normally inhibited by a Progesterone-stimulated oocytes did not exhibit CSF activity protein phosphatase activity called "INH" (22, 23). These until 30-60 min after germinal vesicle breakdown (GVBD). observations indicate a translational requirement, both for Both the appearance of CSF activity and the progression from the initiation of maturation and for progression to meiosis II, meiosis I to meiosis II were inhibited by microinjection of mos"e for a regulatory factor(s) other than cyclin. -

Oocyte Or Embryo Donation to Women of Advanced Reproductive Age: an Ethics Committee Opinion
ASRM PAGES Oocyte or embryo donation to women of advanced reproductive age: an Ethics Committee opinion Ethics Committee of the American Society for Reproductive Medicine American Society for Reproductive Medicine, Birmingham, Alabama Advanced reproductive age (ARA) is a risk factor for female infertility, pregnancy loss, fetal anomalies, stillbirth, and obstetric com- plications. Oocyte donation reverses the age-related decline in implantation and birth rates of women in their 40s and 50s and restores pregnancy potential beyond menopause. However, obstetrical complications in older patients remain high, particularly related to oper- ative delivery and hypertensive and cardiovascular risks. Physicians should perform a thorough medical evaluation designed to assess the physical fitness of a patient for pregnancy before deciding to attempt transfer of embryos to any woman of advanced reproductive age (>45 years). Embryo transfer should be strongly discouraged or denied to women of ARA with underlying conditions that increase or exacerbate obstetrical risks. Because of concerns related to the high-risk nature of pregnancy, as well as longevity, treatment of women over the age of 55 should generally be discouraged. This statement replaces the earlier ASRM Ethics Committee document of the same name, last published in 2013 (Fertil Steril 2013;100:337–40). (Fertil SterilÒ 2016;106:e3–7. Ó2016 by American Society for Reproductive Medicine.) Key Words: Ethics, third-party reproduction, complications, pregnancy, parenting Discuss: You can discuss -

Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal
Female and Male Gametogenesis 3 Nina Desai , Jennifer Ludgin , Rakesh Sharma , Raj Kumar Anirudh , and Ashok Agarwal intimately part of the endocrine responsibility of the ovary. Introduction If there are no gametes, then hormone production is drastically curtailed. Depletion of oocytes implies depletion of the major Oogenesis is an area that has long been of interest in medicine, hormones of the ovary. In the male this is not the case. as well as biology, economics, sociology, and public policy. Androgen production will proceed normally without a single Almost four centuries ago, the English physician William spermatozoa in the testes. Harvey (1578–1657) wrote ex ovo omnia —“all that is alive This chapter presents basic aspects of human ovarian comes from the egg.” follicle growth, oogenesis, and some of the regulatory mech- During a women’s reproductive life span only 300–400 of anisms involved [ 1 ] , as well as some of the basic structural the nearly 1–2 million oocytes present in her ovaries at birth morphology of the testes and the process of development to are ovulated. The process of oogenesis begins with migra- obtain mature spermatozoa. tory primordial germ cells (PGCs). It results in the produc- tion of meiotically competent oocytes containing the correct genetic material, proteins, mRNA transcripts, and organ- Structure of the Ovary elles that are necessary to create a viable embryo. This is a tightly controlled process involving not only ovarian para- The ovary, which contains the germ cells, is the main repro- crine factors but also signaling from gonadotropins secreted ductive organ in the female. -

Review Article Physiologic Course of Female Reproductive Function: a Molecular Look Into the Prologue of Life
Hindawi Publishing Corporation Journal of Pregnancy Volume 2015, Article ID 715735, 21 pages http://dx.doi.org/10.1155/2015/715735 Review Article Physiologic Course of Female Reproductive Function: A Molecular Look into the Prologue of Life Joselyn Rojas, Mervin Chávez-Castillo, Luis Carlos Olivar, María Calvo, José Mejías, Milagros Rojas, Jessenia Morillo, and Valmore Bermúdez Endocrine-Metabolic Research Center, “Dr. Felix´ Gomez”,´ Faculty of Medicine, University of Zulia, Maracaibo 4004, Zulia, Venezuela Correspondence should be addressed to Joselyn Rojas; [email protected] Received 6 September 2015; Accepted 29 October 2015 Academic Editor: Sam Mesiano Copyright © 2015 Joselyn Rojas et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The genetic, endocrine, and metabolic mechanisms underlying female reproduction are numerous and sophisticated, displaying complex functional evolution throughout a woman’s lifetime. This vital course may be systematized in three subsequent stages: prenatal development of ovaries and germ cells up until in utero arrest of follicular growth and the ensuing interim suspension of gonadal function; onset of reproductive maturity through puberty, with reinitiation of both gonadal and adrenal activity; and adult functionality of the ovarian cycle which permits ovulation, a key event in female fertility, and dictates concurrent modifications in the endometrium and other ovarian hormone-sensitive tissues. Indeed, the ultimate goal of this physiologic progression is to achieve ovulation and offer an adequate environment for the installation of gestation, the consummation of female fertility. Strict regulation of these processes is important, as disruptions at any point in this evolution may equate a myriad of endocrine- metabolic disturbances for women and adverse consequences on offspring both during pregnancy and postpartum. -

Interactions Between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction Fritzsche H, Michelmann HW, Siebzehnrübl E Schmedemann RKA J
Journal für Reproduktionsmedizin und Endokrinologie – Journal of Reproductive Medicine and Endocrinology – Andrologie • Embryologie & Biologie • Endokrinologie • Ethik & Recht • Genetik Gynäkologie • Kontrazeption • Psychosomatik • Reproduktionsmedizin • Urologie Interactions between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction Fritzsche H, Michelmann HW, Siebzehnrübl E Schmedemann RKA J. Reproduktionsmed. Endokrinol 2006; 3 (6), 373-378 www.kup.at/repromedizin Online-Datenbank mit Autoren- und Stichwortsuche Offizielles Organ: AGRBM, BRZ, DVR, DGA, DGGEF, DGRM, D·I·R, EFA, OEGRM, SRBM/DGE Indexed in EMBASE/Excerpta Medica/Scopus Krause & Pachernegg GmbH, Verlag für Medizin und Wirtschaft, A-3003 Gablitz Interactions between Oocyte and Surrounding Cumulus Cells Influence the Results of Assisted Reproduction H. Fritzsche1, H. W. Michelmann2, E. Siebzehnrübl3, R. K. A. Schmedemann4 The interactions between oocyte and surrounding cumulus cells, as well as between cumulus oophorus and theca cells, were investigated in IVF/ ICSI cycles. Gap junctions connect cumulus cells with the oocyte, thereby enabling a bi-directional exchange of products essential for optimal oocyte development. GnRH, FSH, LH and E2 play a major role during oocyte maturation. In general, FSH and LH are prerequisites for folliculogenesis, as well as oogenesis, but it is the quantitative threshold value of both that seems to determine oocyte quality and pregnancy rate. It remains to be determined how apoptosis and the anti-Muellerian hormone (AMH) can be used as predictive factors regarding the success of ART. In a retrospec- tive sub-analysis of comparative stimulation regimens, using either LH + FSH (hMG-HP) or FSH (rFSH) alone in GnRH-antagonist down-regulated cycles, it was possible to demonstrate that stimulation with LH and FSH results in a significantly higher pregnancy rate in IVF-patients compared to a stimulation with only FSH. -

Biology of Oocyte Maturation Oogenesis
Biology of Reproduction Unit Biology of Oocyte Maturation Carlos E. Plancha1,2 1 Unidade de Biologia da Reprodução, Inst. Histologia e Biologia do Desenvolvimento, . Faculdade de Medicina de Lisboa, Portugal 2 CEMEARE – Centro Médico de Assistência à Reprodução, Lisboa, Portugal Basic principles in ovarian physiology: relevance for IVF, ESHRE Campus Workshop Lisbon, 19-20 September, 2008 Biology of Reproduction Unit Oogenesis Growth Phase: - Oocyte diameter increases OOCYTE GROWTH - Organelle redistribution - High transcriptional and translational activity - Accumulation of RNA / proteins - Incompetent Æ Competent ooc. Oocyte Maturation: GV Complex series of nuclear and cytoplasmic events with resumption of the 1st meiotic OOCYTE MATURATION division and arrest at MII OVULATION shortly before ovulation MII Ovulation Growth Maturation FERTILIZATION Resumption of meiosis Æ PN formation Embryo development Prophase I Metaphase II Basic principles in ovarian physiology: relevance for IVF, ESHRE Campus Workshop Lisbon, 19-20 September, 2008 Biology of Reproduction Unit Oogenesis in vivo (including oocyte maturation) takes place inside a morfo-functional unit: The Ovarian Follicle Basic principles in ovarian physiology: relevance for IVF, ESHRE Campus Workshop Lisbon, 19-20 September, 2008 Biology of Reproduction Unit Factors involved in oogenesis Igf-1,2,3 and folliculogenesis GDF - 9 FSH,LH Cellular interactions Perifolicular matrix Laminin Basic principles in ovarian physiology: relevance for IVF, ESHRE Campus Workshop Lisbon, 19-20 September,