The Initial Experience at a Single-Center in Turkey
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chemical Composition and Product Quality Control of Turmeric
Stephen F. Austin State University SFA ScholarWorks Faculty Publications Agriculture 2011 Chemical composition and product quality control of turmeric (Curcuma longa L.) Shiyou Li Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Wei Yuan Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Guangrui Deng Ping Wang Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Peiying Yang See next page for additional authors Follow this and additional works at: http://scholarworks.sfasu.edu/agriculture_facultypubs Part of the Natural Products Chemistry and Pharmacognosy Commons, and the Pharmaceutical Preparations Commons Tell us how this article helped you. Recommended Citation Li, Shiyou; Yuan, Wei; Deng, Guangrui; Wang, Ping; Yang, Peiying; and Aggarwal, Bharat, "Chemical composition and product quality control of turmeric (Curcuma longa L.)" (2011). Faculty Publications. Paper 1. http://scholarworks.sfasu.edu/agriculture_facultypubs/1 This Article is brought to you for free and open access by the Agriculture at SFA ScholarWorks. It has been accepted for inclusion in Faculty Publications by an authorized administrator of SFA ScholarWorks. For more information, please contact [email protected]. Authors Shiyou Li, Wei Yuan, Guangrui Deng, Ping Wang, Peiying Yang, and Bharat Aggarwal This article is available at SFA ScholarWorks: http://scholarworks.sfasu.edu/agriculture_facultypubs/1 28 Pharmaceutical Crops, 2011, 2, 28-54 Open Access Chemical Composition and Product Quality Control of Turmeric (Curcuma longa L.) ,1 1 1 1 2 3 Shiyou Li* , Wei Yuan , Guangrui Deng , Ping Wang , Peiying Yang and Bharat B. Aggarwal 1National Center for Pharmaceutical Crops, Arthur Temple College of Forestry and Agriculture, Stephen F. -

RCN DIVING BRANCH HISTORY – Part 7C by Robert Larsen 2014
RCN DIVING BRANCH HISTORY – Part 7C By Robert Larsen 2014 Robert “Red” Larsen wrote that this is a continuation from Part 7B, identifying some main topics and my knowledge of how we used, developed , or used the particular subject. Diving Equipment – SCUBA or CABA(Compressed Air Breathing Apparatus) On the West Coast in 1954, we were introduced to CABA during our initial course. When I look back on it, there did not seem to be a great deal of knowledge from out Instructor’s regarding this breathing apparatus. We referred to the system as an “Aqua Lung”. The breathing regulators had a “Canada Liquid Air” nameplate on them, plus a Serial Number. I just learned via the internet why these were labelled as such – in 1947 Emile Gagnan, co‐inventor with Jacques Cousteau of the Aqua Lung, emigrated to Montreal, Quebec, and worked at Canada Liquid Air Company, developing more regulators, which were the old double hose type. They apparently were a single stage regulator, reducing the tank supply pressure from 1800/2000 PSI to the Diver’s over‐bottom pressure, in one single control stage. You probably wonder why I would remember about the serial numbers? Well, these regulators took a mighty strong set of lungs to be able to draw in your air supply – compared to our more modern equipment, and some of these were much harder than others. Also, on the surface you could identify what Serial Number the Diver was using, by the sound of the exhaust bubbles! Number “1101” was always able to be identified in this manner(Jim Balmforth and I were discussing this feature recently when I travelled out to the West Coast). -

À 02:00 PM 2021-03-31 On
1 1 RETURN BIDS TO: Title - Sujet MAINTENANCE DIVING EQUIPMENT RETOURNER LES SOUMISSIONS À: Bid Receiving - PWGSC / Réception des Solicitation No. - N° de l'invitation Date soumissions - TPSGC W8482-182212/B 2021-02-11 11 Laurier St. / 11, rue Laurier Client Reference No. - N° de référence du client GETS Ref. No. - N° de réf. de SEAG Place du Portage, Phase III Core 0B2 / Noyau 0B2 W8482-182212 PW-$ISM-027-28097 Gatineau File No. - N° de dossier CCC No./N° CCC - FMS No./N° VME Quebec 027ism.W8482-182212 K1A 0S5 Bid Fax: (819) 997-9776 Solicitation Closes - L'invitation prend fin at - à 02:00 PM Eastern Daylight Saving Time EDT on - le 2021-03-31 Heure Avancée de l'Est HAE LETTER OF INTEREST F.O.B. - F.A.B. LETTRE D'INTÉRÊT Plant-Usine: Destination: Other-Autre: Address Enquiries to: - Adresser toutes questions à: Buyer Id - Id de l'acheteur Beaumier, Julie 027ism Telephone No. - N° de téléphone FAX No. - N° de FAX (613) 851-9981 ( ) ( ) - Destination - of Goods, Services, and Construction: Destination - des biens, services et construction: Specified Herein Précisé dans les présentes Comments - Commentaires Instructions: See Herein Instructions: Voir aux présentes Vendor/Firm Name and Address Raison sociale et adresse du fournisseur/de l'entrepreneur Delivery Required - Livraison exigée Delivery Offered - Livraison proposée See Herein – Voir ci-inclus Vendor/Firm Name and Address Raison sociale et adresse du fournisseur/de l'entrepreneur Telephone No. - N°de téléphone Facsimile No. - N° de télécopieur Issuing Office - Bureau de distribution Name and title of person authorized to sign on behalf of Vendor/Firm In-Service Support Marine / Soutien en Service Maritime (type or print) 11 Laurier St. -

Section 3.7 Marine Mammals
Point Mugu Sea Range Draft EIS/OEIS April 2020 Environmental Impact Statement/ Overseas Environmental Impact Statement Point Mugu Sea Range TABLE OF CONTENTS 3.7 Marine Mammals ............................................................................................................. 3.7-1 3.7.1 Introduction .......................................................................................................... 3.7-1 3.7.2 Region of Influence ............................................................................................... 3.7-1 3.7.3 Approach to Analysis ............................................................................................ 3.7-1 3.7.4 Affected Environment ........................................................................................... 3.7-2 3.7.4.1 General Background .............................................................................. 3.7-2 3.7.4.2 Mysticete Cetaceans Expected in the Study Area ............................... 3.7-28 3.7.4.3 Odontocete Cetaceans Expected in the Study Area ............................ 3.7-50 3.7.4.4 Otariid Pinnipeds Expected in the Study Area ..................................... 3.7-79 3.7.4.5 Phocid Pinnipeds Expected in the Study Area ..................................... 3.7-85 3.7.4.6 Mustelids (Sea Otter) Expected in the Study Area .............................. 3.7-89 3.7.5 Environmental Consequences ............................................................................ 3.7-91 3.7.5.1 Long-Term Consequences .................................................................. -

Mathematical Optimisation of Diver Ascent Profiles at a Constant Risk of Decompression Illness
MATHEMATICAL OPTIMISATION OF DIVER ASCENT PROFILES AT A CONSTANT RISK OF DECOMPRESSION ILLNESS A thesis submitted in partial fulfilment of the requirements for the Degree of Doctor of Philosophy m Computational and Applied Mathematics by B. J. Horn University of Canterbury 2003 11 rro my parents for encouraging a rove of [earning &V ~3~ 'blt ,Slf , HIS)3 iii Acknowledgements I wish to thank my supervisors Professor Graeme Wake (University of Canterbury) and Gavin Anthony (QinetiQ Alverstoke) for their encouragement and always being available for discussion, information and advice. I would also like to thank Dr. Chris Price for discussing the finer points of optimisation with me and Dr. Britta Basse for being a sounding board for ideas and sharing her MATLAB knowledge. I would also like to gratefully acknowledge the research grant and information provided by QinetiQ Alverstoke that made the research possible. This thesis would not have been completed without the never ending support and proof reading ability of my husband Clive who could always pick out the areas that needed clarification. As well as my kids who provided some light relief from the challenges of research. Finally I would like to acknowledge the ladies of the UCSA Creche, who welcomed my family into the creche community and provided a supportive, safe and fun environment for my daughters that allowed me to finish this research. - 1 JUN 2004 v Abstract Divers use decompression schedules that provide a stepped ascent to the surface from their maximum depth to help prevent the occurrence of decompression illness. The risk of decompression illness resulting from these schedules varies across different dives and the models used to generate them. -

PMSR LOA Application August 2020
REQUEST FOR REGULATIONS AND LETTER OF AUTHORIZATION FOR THE INCIDENTAL TAKING OF MARINE MAMMALS RESULTING FROM U.S. NAVY TESTING AND TRAINING ACTIVITIES IN THE POINT MUGU SEA RANGE STUDY AREA Submitted to: Office of Protected Resources National Marine Fisheries Service 1315 East-West Highway Silver Spring, Maryland 20910-3226 Submitted by: Commander, Naval Air Warfare Center Weapons Division Code: EB2R00M 575 I Street, Suite 1 M/S 0460 Point Mugu, CA 93042-5049 August 2020 Request for Letter of Authorization for the Incidental Taking of Marine Mammals Resulting from U.S. Navy Testing and Training Activities in the Point Mugu Sea Range Study Area Table of Contents TABLE OF CONTENTS 1 DESCRIPTION OF SPECIFIED ACTIVITY ...................................................................................................... 1-1 1.1 INTRODUCTION ............................................................................................................................................. 1-1 1.2 BACKGROUND .............................................................................................................................................. 1-3 1.3 PRIMARY MISSION AREAS ............................................................................................................................... 1-4 1.3.1 Air Warfare .......................................................................................................................................... 1-4 1.3.1.1 Air-to-Air ..................................................................................................................................................... -

Surface Supplied Diving Manual
B-GG-380-000/FP-003 CANADIAN FORCES DIVING MANUAL VOLUME 3 SURFACE SUPPLIED DIVING MANUAL (Supersedes B-GG-380-000/FP-003 dated 2002-09-01) Issued on Authority of the Chief of the Defence Staff. Publiée avec l’autorisation du Chef de l’étatmajor de la Défense. OPI: D DIVE S 2010-05-10 B-GG-380-000/FP-003 LIST OF EFFECTIVE PAGES Insert latest changed pages. Dispose of superseded pages in accordance with applicable orders. NOTE On a changed page, the portion of the text affected by the latest change is indicated by a vertical line | in the margin of the page. Changes to illustrations are indicated by miniature pointing hands ) or black vertical lines |. Dates of issue for original and changed pages are: Original 0 2010-05-10 Zero in Change No. column indicates an original page. Total number of pages in this publication is 388 consisting of the following: Page Nos. Change No. Page Nos. Change No. Title page ........................................ 0 3A-1 to 3A-68 ................................... 0 A ...................................................... 0 3B-1 to 3B-4 ..................................... 0 i to xvi ............................................... 0 3C-1 to 3C-49 .................................. 0 i, ii..................................................... 0 i to iii ................................................. 0 1-1-1, 1-1-2 ...................................... 0 4-1-1 ................................................. 0 1-2-1 to 1-2-6 ................................... 0 4-2-1 to 4-2-9 ................................... 0 1-3-1 to 1-3-3 ................................... 0 4-3-1 to 4-3-9 ................................... 0 i, ii..................................................... 0 4-4-1 to 4-4-9 ................................... 0 2-1-1 to 2-1-10 ................................. 0 4-5-1 ................................................ -

Structure-Activity Relationship of Dihydroxy-4-Methylcoumarins As
Biochimie 92 (2010) 1089e110 0 Contents lists available at ScienceDirect Biochimie journal homepage: www.elsevier.com/locate/biochi Research paper Structureeactivity relationship of dihydroxy-4-methylcoumarins as powerful antioxidants: Correlation between experimental & theoretical data and synergistic effect Vessela D. Kancheva a,**, Luciano Saso b, Petya V. Boranova a, Abdullah Khan c, Manju K. Saroj c, Mukesh K. Pandey c, Shashwat Malhotra c, Jordan Z. Nechev a, Sunil K. Sharma c, Ashok K. Prasad c, Maya B. Georgieva d, Carleta Joseph e, Anthony L. DePass e, Ramesh C. Rastogi c, Virinder S. Parmar c,* a Lipid Chemistry Department, Institute of Organic Chemistry with Centre of Phytochemistry, Bulgarian Academy of Sciences, 1113 Sofia, Bulgaria b Department of Human Physiology and Pharmacology “Vittorio Erspamer”, University La Sapienza, P.le Aldo Moro 5, 00185 Rome, Italy c Bioorganic Laboratory, Department of Chemistry, University of Delhi, Delhi 110 007, India d Department of Organic Synthesis and Fuels, University of Chemical Technology and Metallurgy, 1756 Sofia, Bulgaria e Department of Biology, Long Island University, DeKalb Avenue, Brooklyn, NY 11201, USA article info abstract Article history: The chain-breaking antioxidant activities of eight coumarins [7-hydroxy-4-methylcoumarin (1), Received 24 March 2010 5,7-dihydroxy-4-methylcoumarin (2), 6,7-dihydroxy-4-methylcoumarin (3), 6,7-dihydroxycoumarin (4), Accepted 11 June 2010 7,8-dihydroxy-4-methylcoumarin (5), ethyl 2-(7,8-dihydroxy-4-methylcoumar-3-yl)-acetate (6), 7,8- Available online 19 June 2010 diacetoxy-4-methylcoumarin (7) and ethyl 2-(7,8-diacetoxy-4-methylcoumar-3-yl)-acetate (8)] during bulk lipid autoxidation at 37 C and 80 C in concentrations of 0.01e1.0 mM and their radical scavenging Keywords: activities at 25 C using TLCeDPPH test have been studied and compared. -

EXHIBIT a Case 1:12-Cv-00128-DB Document 200-1 Filed 12/15/14 Page 2 of 36
Case 1:12-cv-00128-DB Document 200-1 Filed 12/15/14 Page 1 of 36 EXHIBIT A Case 1:12-cv-00128-DB Document 200-1 Filed 12/15/14 Page 2 of 36 Dr. David Sawatzky SC, CD, BMedSc, MSc, MD 309-1350 Oxford Street Halifax, Nova Scotia B3H 3Y8 CANADA Phones: 902-266-2065 cell 902-720-1558 office Email: [email protected] EXPERT OPINION of Dr. David Sawatzky Tuvell v. Boy Scouts of America, PADI, Blue Water Scuba of Logan, Lowell Huber, Corbett Douglas, Bear Lake Aquatic Base and Great Salt Lake Council of the Boy Scouts of America AUTHOR PROFESSIONAL BACKGROUND: All of the opinions I express in this report are to a reasonable degree of medical and professional certainty in accordance with my experience and qualifications. My qualifications to comment on this case include the fact that I am a medical doctor who has specialized in diving medicine since 1982 and I have a Master of Science degree in Diving/Exercise Physiology. I have had over 300 articles published on diving medicine and have written a book (Dr. Sawatzky’s Diving Medicine Notes) that went through five editions. I have written a regular column on diving medicine for Diver Magazine Canada since 1993 and Sport Diving Australia since 2007. I have taught on a large number of diving medicine courses and I have been a Consultant in Diving Medicine since 1986. I have been an active recreational/cave/technical diver since 1982 and I am an Instructor Trainer with IANTD for many forms of diving including Technical, Cave, Wreck, Trimix, and Closed Circuit Rebreathers. -
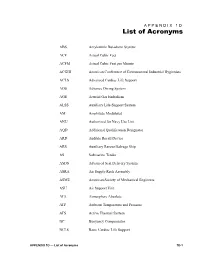
APPENDIX 1D — List of Acronyms 1D-1 BIBS Built-In Breathing System
APPENDIX 1D /LVWRI$FURQ\PV ABS Acrylonitile Butadiene Styrene ACF Actual Cubic Feet ACFM Actual Cubic Feet per Minute ACGIH American Conference of Governmental Industrial Hygienists ACLS Advanced Cardiac Life Support ADS Advance Diving System AGE Arterial Gas Embolism ALSS Auxiliary Life-Support System AM Amplitude Modulated ANU Authorized for Navy Use List AQD Additional Qualification Designator ARD Audible Recall Device ARS Auxiliary Rescue/Salvage Ship AS Submarine Tender ASDS Advanced Seal Delivery System ASRA Air Supply Rack Assembly ASME American Society of Mechanical Engineers ASU Air Support Unit ATA Atmosphere Absolute ATP Ambient Temperature and Pressure ATS Active Thermal System BC Buoyancy Compensator BCLS Basic Cardiac Life Support APPENDIX 1D — List of Acronyms 1D-1 BIBS Built-In Breathing System BPM Breaths per Minute BTPS Body Temperature, Ambient Pressure BTU British Thermal Unit CDO Command Duty Officer CDU Consolidated Diving Unit CETU Closed-Circuit Television CGA Compressed Gas Association CNO Chief of Naval Operations CNS Central Nervous System CONUS Continental United States COSAL Coordinated Shipboard Allowance List CPR Cardiopulmonary Resuscitation CRS Chamber Reducing Station CSMD Combat Swimmer Multilevel Dive CSS Coastal System Station CUMA Canadian Underwater Minecoutermeasures Apparatus CWDS Contaminated Water Diving System CWPDS Chemical Warfare Protective Dry Suit DATPS Divers Active Thermal Protection System DC Duty Cycle DCIEM Defense & Civil Institute of Environmental Medicine DCS Decompression Sickness -
2017 June;47(2):75-81.) Introduction: Important Developments in the Diagnosis of Scuba Diving Fatalities Have Been Made Thanks to Forensic Imaging Tool Improvements
Diving and Hyperbaric Medicine The Journal of the South Pacific Underwater Medicine Society and the European Underwater and Baromedical Society Volume 47 No. 2 June 2017 Oxygen explosion at a remote dive site Post-mortem cardiac gas analysis: can it help diagnosis? Otology 101: diving problems and their management Decompression illness: no clear consensus in Singapore HBO and ischaemia-reperfusion injury: a paradox Transcutaneous oximetry: normal values in healthy adults Hospital coding of HBOT: not fit for purpose Print Post Approved PP 100007612 ISSN 1833-3516, ABN 29 299 823 713 Diving and Hyperbaric Medicine Volume 47 No. 2 June 2017 PURPOSES OF THE SOCIETIES To promote and facilitate the study of all aspects of underwater and hyperbaric medicine To provide information on underwater and hyperbaric medicine To publish a journal and to convene members of each Society annually at a scientific conference SOUTH PACIFIC UNDERWATER EUROPEAN UNDERWATER AND MEDICINE SOCIETY BAROMEDICAL SOCIETY OFFICE HOLDERS OFFICE HOLDERS President President David Smart <[email protected]> Jacek Kot <[email protected]> Past President Vice President Michael Bennett <[email protected]> Ole Hyldegaard <[email protected]> Secretary Immediate Past President Douglas Falconer <[email protected]> Costantino Balestra <[email protected]> Treasurer Past President Sarah Lockley <[email protected]> Peter Germonpré <[email protected]> Education Officer Honorary Secretary David Wilkinson <[email protected]> Peter Germonpré -

Acute Carbon Monoxide Poisoning
Case Report THE JOURNAL OF ACADEMIC 43 Olgu Sunumu EMERGENCY MEDICINE An Unusual Cause of Rhabdomyolysis: Acute Carbon Monoxide Poisoning Rabdomyolizin Nadir Bir Sebebi: Akut Karbon Monoksit Zehirlenmesi Suat Zengin, Behçet Al, Cuma Yıldırım, Erdal Yavuz, Aycan Akcalı Department of Emergency Medicine, Faculty of Medicine, Gaziantep University, Gaziantep, Turkey Abstract Özet Carbon monoxide (CO) is a toxic gas produced by the incomplete combustion Karbon monoksit (CO); karbon ihtiva eden bileşiklerin tam yanmaması ile mey- of carbon-containing compounds. Exposure to high concentrations of CO can dana gelen toksik bir gazdır. CO’e yüksek konsantrasyonlarda maruz kalmak be lethal and is the most common cause of death from poisoning worldwide. öldürücü olabilir ve dünya genelinde zehirlenme ölümlerinin en sık nedenidir. Rhabdomyolysis caused by CO poisoning is uncommon. Early recognition of CO zehirlenmesinin sebep olduğu rabdomiyoliz nadirdir. Böyle olgularda rab- rhabdomyolysis in such cases is important, since this complication can be domiyolizin erken tanınması önemlidir. Çünkü bu komplikasyon akut böbrek fatal as it leads to acute renal failure. However, the prognosis is excellent if yetmezliğine yol açarak ölümcül olabilir. Ancak, uygun tıbbi yönetimi sağlanır- proper medical management is provided. In the present study, we discuss sa, prognozu mükemmeldir. Bu çalışmada, CO zehirlenmesi nedeniyle rabdomi- rhabdomyolysis caused by CO poisoning in a 68-year-old man. yoliz gelişen 68 yaşındaki bir adamı değerlendirdik. (JAEM 2013; 12: 43-5) (JAEM 2013; 12: 43-5) Anahtar kelimeler: Karbon monoksit zehirlenmesi, karboksihemoglobin, Key words: Carbon monoxide poisoning, carboxyhemoglobin, rhabdomyolysis rabdomyoliz Introduction respiratory rate was 22 breaths per min, and blood pressure was 158/80 mmHg. According to the information acquired from his rela- Carbon monoxide (CO) is a colorless, odorless, tasteless, and non- tives, he had no other diseases and did not use any drugs.