EXHIBIT a Case 1:12-Cv-00128-DB Document 200-1 Filed 12/15/14 Page 2 of 36
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The University of Florida Diving Science and Safety Program AAUS STANDARDS for SCIENTIFIC DIVING
The University of Florida Diving Science and Safety Program AAUS STANDARDS FOR SCIENTIFIC DIVING 2019 1 FOREWORD Since 1951 the scientific diving community has endeavored to promote safe, effective diving through self-imposed diver training and education programs. Over the years, manuals for diving safety have been circulated between organizations, revised and modified for local implementation, and have resulted in an enviable safety record. This document represents the minimal safety standards for scientific diving at the present day. As diving science progresses so must this standard, and it is the responsibility of every member of the Academy to see that it always reflects state of the art, safe diving practice. American Academy of Underwater Sciences ACKNOWLEDGEMENTS The Academy thanks the numerous dedicated individual and organizational members for their contributions and editorial comments in the production of these standards. Revision History Approved by AAUS BOD December 2018 Available at www.aaus.org/About/Diving Standards 2 Table of Contents Volume 1 ..................................................................................................................................................... 6 Section 1.00 GENERAL POLICY .........................................................................................................................7 1.10 Scientific Diving Standards .........................................................................................................................7 1.20 Operational Control -

How Do Scientists Explore Underwater Ecosystems?
LESSON 2 How do scientists Age 11-14 explore underwater 60 minutes ecosystems? Curriculum links Lesson overview • Understand the scale of coral Throughout this lesson students explore underwater habitats reefs and the purpose of the and begin to understand the importance of the XL Catlin XL Catlin Seaview Survey Seaview Survey. Students consider why exploration of this • Identify the challenges kind can be challenging for humans and learn dive signs so scientist working underwater face they can communicate on their virtual dive. During the virtual • Sort and classify species dive students use 360 virtual reality to explore this dynamic environment, identifying some of the species that live there. Students go on to classify these species and record the findings of their first dive. Resources Lesson steps Learning outcomes Slideshow 2: How do scientists 1. What is the ocean habitat like? explorer underwater (10 mins) ecosystems? Students are introduced to the coral • Know that we live on a ‘blue planet’ Student Sheet 2a: ocean through a quiz to understand Video reflection the scale and complexity of this • Name a variety of ocean habitats ecosystem. and species that live there Student Sheet 2b: Species card sort 2. How is the baseline survey being Student Sheet 2c: Dive created? (10 mins) log Students become familiar with • Describe the XL Catlin Seaview the XL Catlin Seaview Survey and Survey and its scientific aims Video: the scientific rational behind the What kind of people exploration. make up a coral expedition team? 3. How do scientists work underwater? (15 mins) Video: Students consider some of the • Understand the different What are dive signs and challenges scientists face working techniques scientists use to work what do they mean? in this environment and practice underwater Google Map: using dive signs to communicate. -

Chemical Composition and Product Quality Control of Turmeric
Stephen F. Austin State University SFA ScholarWorks Faculty Publications Agriculture 2011 Chemical composition and product quality control of turmeric (Curcuma longa L.) Shiyou Li Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Wei Yuan Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Guangrui Deng Ping Wang Stephen F Austin State University, Arthur Temple College of Forestry and Agriculture, [email protected] Peiying Yang See next page for additional authors Follow this and additional works at: http://scholarworks.sfasu.edu/agriculture_facultypubs Part of the Natural Products Chemistry and Pharmacognosy Commons, and the Pharmaceutical Preparations Commons Tell us how this article helped you. Recommended Citation Li, Shiyou; Yuan, Wei; Deng, Guangrui; Wang, Ping; Yang, Peiying; and Aggarwal, Bharat, "Chemical composition and product quality control of turmeric (Curcuma longa L.)" (2011). Faculty Publications. Paper 1. http://scholarworks.sfasu.edu/agriculture_facultypubs/1 This Article is brought to you for free and open access by the Agriculture at SFA ScholarWorks. It has been accepted for inclusion in Faculty Publications by an authorized administrator of SFA ScholarWorks. For more information, please contact [email protected]. Authors Shiyou Li, Wei Yuan, Guangrui Deng, Ping Wang, Peiying Yang, and Bharat Aggarwal This article is available at SFA ScholarWorks: http://scholarworks.sfasu.edu/agriculture_facultypubs/1 28 Pharmaceutical Crops, 2011, 2, 28-54 Open Access Chemical Composition and Product Quality Control of Turmeric (Curcuma longa L.) ,1 1 1 1 2 3 Shiyou Li* , Wei Yuan , Guangrui Deng , Ping Wang , Peiying Yang and Bharat B. Aggarwal 1National Center for Pharmaceutical Crops, Arthur Temple College of Forestry and Agriculture, Stephen F. -
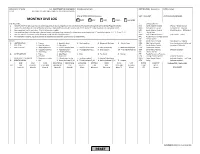
MONTHLY DIVE LOG ⃝ NMFS ⃝ NOS ⃝ OAR ⃝ OMAO ⃝ Non-NOAA
NOAA Form 57-10-24 U.S. DEPARTMENT OF COMMERCE NAME (Last, First MI) CERTIFICATION (see note 1) DATE (mm/yy) (7-12) NATIONAL OCEANIC AND ATMOSPHERIC ADMINISTRATION LINE or STAFF OFFICE (Check one) UNIT / SUB-UNIT UNIT DIVING SUPERVISOR MONTHLY DIVE LOG ⃝ NMFS ⃝ NOS ⃝ OAR ⃝ OMAO ⃝ non-NOAA INSTRUCTIONS: 7. DIVE LOCATION 1. NOAA Form 57-03-24 (1-12) may be used to log dives in lieu of using the on-line, electronic form available through the NOAA Diving Program website. NAC North Atlantic Coastal (Maine – Rhode Island) 2. Submit this form directly to the NOAA Diving Center, 7600 Sand Point Way NE, Seattle, WA, 98115 by the 5th of the month for the preceding month. MAC Mid-Atlantic Coastal (Connecticut – Virginia) 3. Use a separate line for each dive. Print all information legibly. SAC South Atlantic Coastal (North Carolina – SE Florida) 4. Log repetitive dives using the date, a decimal point, and consecutive numbers (i.e. three dives conducted on the 15th would be listed as 15.1, 15.2, and 15.3). KEY Florida Keys 5. Use the codes in the NOTES section below to encode the dive log information. GMC Gulf of Mexico Coastal (SW Florida – Texas) 6. For saturation missions, log all excursions as separate dives and time of excursions as bottom time. PVC Puerto Rico/U.S. Virgin Islands AKC Alaska Coastal NOTES: NPC North Pacific Coastal (Washington – Oregon) 1. CERTIFICATION 1 - Trainee 2 - Scientific Diver 3 - Working Diver 4 - Advanced Working 5 – Master Diver MPC Mid-Pacific Coastal (north and central California) 2. -

Diving and Hyperbaric Medicine
Diving and Hyperbaric Medicine 7KH-RXUQDORIWKH6RXWK3DFL¿F8QGHUZDWHU0HGLFLQH6RFLHW\ ,QFRUSRUDWHGLQ9LFWRULD $% ISSN 1833 - 3516 Volume 37 No. 4 ABN 29 299 823 713 December 2007 Diving expeditions: from Antarctica to the Tropics Diving deaths in New Zealand Epilepsy and diving – time for a change? Mechanical ventilation of patients at pressure Print Post Approved PP 331758/0015 9^k^c\VcY=neZgWVg^XBZY^X^cZKdajbZ(,Cd#)9ZXZbWZg'%%, PURPOSES OF THE SOCIETY IdegdbdiZVcY[VX^a^iViZi]ZhijYnd[VaaVheZXihd[jcYZglViZgVcY]neZgWVg^XbZY^X^cZ Idegdk^YZ^c[dgbVi^dcdcjcYZglViZgVcY]neZgWVg^XbZY^X^cZ IdejWa^h]V_djgcVa IdXdckZcZbZbWZghd[i]ZHdX^ZinVccjVaanViVhX^Zci^ÄXXdc[ZgZcXZ OFFICE HOLDERS EgZh^YZci 9g8]g^h6Xdii (%EVg`6kZcjZ!GdhhancEVg` :çbV^a1XVXdii5deijhcZi#Xdb#Vj3 Hdji]6jhigVa^V*%,' EVhiçEgZh^YZci 9gGdWncLVa`Zg &'7VggVaa^ZgHigZZi!<g^[Äi] :çbV^a1GdWnc#LVa`Zg5YZ[ZcXZ#\dk#Vj3 68I'+%( HZXgZiVgn 9gHVgV]H]Vg`Zn E#D#7DM&%*!CVggVWZZc :çbV^a1hejbhhZXgZiVgn5\bV^a#Xdb3 CZlHdji]LVaZh'&%& IgZVhjgZg 9g<jnL^aa^Vbh E#D#7dm&.%!GZY=^aaHdji] :çbV^a1hejbh5[VhibV^a#cZi3 K^Xidg^V(.(, :Y^idg 6hhdX#Egd[#B^`Z9Vk^h 8$d=neZgWVg^XBZY^X^cZJc^i :çbV^a1hejbh_5XY]W#\dki#co3 8]g^hiX]jgX]=dhe^iVa!Eg^kViZ7V\),&%!8]g^hiX]jgX]!CO :YjXVi^dcD[ÄXZg 9g;^dcVH]Vge ').XC^X]dahdcGdVY!H]ZcidcEVg` :çbV^a1h]Vge^Z[5YdXidgh#dg\#j`3 LZhiZgc6jhigVa^V+%%- EjWa^XD[ÄXZg 9gKVcZhhV=VaaZg E#D#7dm-%'(!8Vggjb9dlch :çbV^a1kVcZhhV#]VaaZg5XYbX#Xdb#Vj3 K^Xidg^V('%& 8]V^gbVc6CO=B< 9g9Vk^YHbVgi 9ZeVgibZcid[9^k^c\VcY=neZgWVg^XBZY^X^cZ :çbV^a1YVk^Y#hbVgi5Y]]h#iVh#\dk#Vj3 GdnVa=dWVgi=dhe^iVa!=dWVgi!IVhbVc^V,%%% LZWbVhiZg -

The a Aviato Or Prog Gram
CAN UNCLASSIFIED The Aviator Program Juliana Fung Wendy Sullivan-Kwantes DRDC – Toronto Research Centre Vaughn Cosman DRDC – Corporate Office Defence Research and Development Canada Reference Document DRDC-RDDC-2018-D094 November 2018 CAN UNCLASSIFIED CAN UNCLASSIFIED IMPORTANT INFORMATIVE STATEMENTS This document was reviewed for Controlled Goods by Defence Research and Development Canada (DRDC) using the Schedule to the Defence Production Act. Disclaimer: Her Majesty the Queen in right of Canada, as represented by the Minister of National Defence ("Canada"), makes no representations or warranties, express or implied, of any kind whatsoever, and assumes no liability for the accuracy, reliability, completeness, currency or usefulness of any information, product, process or material included in this document. Nothing in this document should be interpreted as an endorsement for the specific use of any tool, technique or process examined in it. Any reliance on, or use of, any information, product, process or material included in this document is at the sole risk of the person so using it or relying on it. Canada does not assume any liability in respect of any damages or losses arising out of or in connection with the use of, or reliance on, any information, product, process or material included in this document. Endorsement statement: This publication has been published by the Editorial Office of Defence Research and Development Canada, an agency of the Department of National Defence of Canada. Inquiries can be sent to: Publications.DRDC-RDDC@drdc- rddc.gc.ca. This document refers to an attachment. To request access to this attachment, please email [email protected], citing the DRDC document number. -
Dive Log Australia
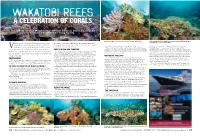
WAKATOBI REEFS A CELEBRATION OF CORALS The famous resort of Wakatobi in South East Sulawesi, Indonesia, probably needs no introduction for many readers. The shallow reef flats in 1 or 2 meters are a great place to start Blue waters swirl above and a hint of clouds in a blue sky prevail. Early morning shafts of sunlight bathe a coral head with light producing a surreal image of corals in the sunlight. eteran pioneer Australian Underwater Photographer the idyllic location and accommodation, the wonderful hospitality, Kevin Deacon decided to forgo all other genres of the range of dive sites, dive boat facilities and all round diver support, one will not suffer for their art here! clown fish and fast growing Acropora & soft corals. produced a portfolio that I believe is faithful to the genre of Vunderwater photography during his most recent tour While cruising this area the creative mind must be fully engaged "Beautiful Reefs". I hope you enjoy these images and the to concentrate on capturing the simple beauty of Wakatobi REEF HUNTING AND SHOOTING looking for the right coral reef elements. By its very nature coral reefs information here helps you on your way as a `Master of the Light’. Indo Pacific coral reefs. A task not as simple as it might seem Creating such images comes with some great challenges. Cruising and their inhabitants are designed to create confusion to the eye, all Kevin Deacon is one of the pioneers of underwater photography in but the resulting images illustrate the value in the age old rule, a coral reef leaves one with an impression of living beauty with part of nature's survival strategy. -

RCN DIVING BRANCH HISTORY – Part 7C by Robert Larsen 2014
RCN DIVING BRANCH HISTORY – Part 7C By Robert Larsen 2014 Robert “Red” Larsen wrote that this is a continuation from Part 7B, identifying some main topics and my knowledge of how we used, developed , or used the particular subject. Diving Equipment – SCUBA or CABA(Compressed Air Breathing Apparatus) On the West Coast in 1954, we were introduced to CABA during our initial course. When I look back on it, there did not seem to be a great deal of knowledge from out Instructor’s regarding this breathing apparatus. We referred to the system as an “Aqua Lung”. The breathing regulators had a “Canada Liquid Air” nameplate on them, plus a Serial Number. I just learned via the internet why these were labelled as such – in 1947 Emile Gagnan, co‐inventor with Jacques Cousteau of the Aqua Lung, emigrated to Montreal, Quebec, and worked at Canada Liquid Air Company, developing more regulators, which were the old double hose type. They apparently were a single stage regulator, reducing the tank supply pressure from 1800/2000 PSI to the Diver’s over‐bottom pressure, in one single control stage. You probably wonder why I would remember about the serial numbers? Well, these regulators took a mighty strong set of lungs to be able to draw in your air supply – compared to our more modern equipment, and some of these were much harder than others. Also, on the surface you could identify what Serial Number the Diver was using, by the sound of the exhaust bubbles! Number “1101” was always able to be identified in this manner(Jim Balmforth and I were discussing this feature recently when I travelled out to the West Coast). -
IQ-1301 TC1 Dive Computer
TUSA TC1 ( IQ1301 ) DIVE COMPUTER USER GUIDE【1st/en】 The CE mark is used to mark conformity with the European Union EMC directive 2014/30/EU. IN-TC1-EN-1ST Page 1 ■■■■■■■■■ USER GUIDE【1st.】 Thank you for choosing the TUSA TC1(IQ1301) Dive Computer. ◆This dive computer does not conform to Dive watches (100m) stated in the ISO6425 and JISB7023. Applications This is a dive computer to support no decompression diving safely. The TUSA TC1(IQ1301) functions as a watch, alarm, timer, stopwatch. In Dive Mode, information of water depth, water temperature, dive time, ascent rate and decompression are provided. When divers exceed no decompression limits, the dive computer will show audible and visual alarms. Comprehensive accelerated decompression is possible because each fraction of oxygen (O2) % can be set from 21% to 56% in 1% increments. The calculation model used for decompression is based on the decompression theory of Dr. A. Buhlmann (ZHL-16C). Before use, you need understand all warnings and cautions of the dive computer written in this Instruction Manual. To avoid any serious accidents, please make sure to read and fully understand the dive computer and its functions. Understanding and using the functions of the dive computer ensures your safe diving. Page 2 Safety Precautions Please read the following before use. TUSA shall assume no responsibility on damage, lost profit and/or any claims caused in use or by malfunctions of this dive computer from customers and any third parties. Danger • Make sure you understand how to use the warnings, and cautions of this dive computer within this Instruction Manual before use. -
Diving Safe Practices Manual
Diving Safe Practices Manual Underwater Inspection Program U.S. Department of the Interior February 2021 Mission Statements The Department of the Interior conserves and manages the Nation’s natural resources and cultural heritage for the benefit and enjoyment of the American people, provides scientific and other information about natural resources and natural hazards to address societal challenges and create opportunities for the American people, and honors the Nation’s trust responsibilities or special commitments to American Indians, Alaska Natives, and affiliated island communities to help them prosper. The mission of the Bureau of Reclamation is to manage, develop, and protect water and related resources in an environmentally and economically sound manner in the interest of the American public. Diving Safe Practices Manual Underwater Inspection Program Prepared by R. L. Harris (September 2006) Regional Dive Team Leader and Chair Reclamation Diving Safety Advisory Board Revised by Reclamation Diving Safety Advisory Board (February 2021) Diving Safe Practices Manual Contents Page Contents .................................................................................................................................. iii 1 Introduction .............................................................................................................. 1 1.1 Use of this Manual ............................................................................................. 1 1.2 Diving Safety ..................................................................................................... -

2018 September;48(3):132−140
Diving and Hyperbaric Medicine The Journal of the South Pacific Underwater Medicine Society and the European Underwater and Baromedical Society Volume 48 No. 3 September 2018 Subclavian Doppler bubble monitoring Australian snorkelling and diving fatalities 2012 Inner ear barotrauma – a tool for diagnosis Which tooth restoration for divers? HBOT for large bowel anastomosis problems ISSN 2209-1491 (online); ISSN 1833-3516 (print) ABN 29 299 823 713 CONTENTS Diving and Hyperbaric Medicine Volume 48 No.3 September 2018 Editorials 198 Baltic Symposium on Diving and Hyperbaric Medicine 2018 129 The Editor’s offering Fiona Sharp 130 Decompression sickness, fatness and active hydrophobic spots Pieter Jan AM van Ooij Book review 199 Gas bubble dynamics in the human body Original articles John Fitz-Clarke 132 Reliability of venous gas embolism detection in the subclavian area for decompression stress assessment following scuba diving Julien Hugon, Asya Metelkina, Axel Barbaud, Ron Nishi, Fethi Bouak, SPUMS notices and news Jean-Eric Blatteau, Emmanuel Gempp 141 Provisional report on diving-related fatalities in Australian 201 ANZ Hyperbaric Medicine Group waters in 2011 Introductory Course in Diving John Lippmann, Chris Lawrence, Andrew Fock, Scott Jamieson and Hyperbaric Medicine 2019 168 Impact of various pressures on fracture resistance and 201 Australian and New Zealand microleakage of amalgam and composite restorations College of Anaesthetists Diving Elnaz Shafigh, Reza Fekrazad, Amir Reza Beglou and Hyperbaric Medicine Special 173 Meta-analysis -

À 02:00 PM 2021-03-31 On
1 1 RETURN BIDS TO: Title - Sujet MAINTENANCE DIVING EQUIPMENT RETOURNER LES SOUMISSIONS À: Bid Receiving - PWGSC / Réception des Solicitation No. - N° de l'invitation Date soumissions - TPSGC W8482-182212/B 2021-02-11 11 Laurier St. / 11, rue Laurier Client Reference No. - N° de référence du client GETS Ref. No. - N° de réf. de SEAG Place du Portage, Phase III Core 0B2 / Noyau 0B2 W8482-182212 PW-$ISM-027-28097 Gatineau File No. - N° de dossier CCC No./N° CCC - FMS No./N° VME Quebec 027ism.W8482-182212 K1A 0S5 Bid Fax: (819) 997-9776 Solicitation Closes - L'invitation prend fin at - à 02:00 PM Eastern Daylight Saving Time EDT on - le 2021-03-31 Heure Avancée de l'Est HAE LETTER OF INTEREST F.O.B. - F.A.B. LETTRE D'INTÉRÊT Plant-Usine: Destination: Other-Autre: Address Enquiries to: - Adresser toutes questions à: Buyer Id - Id de l'acheteur Beaumier, Julie 027ism Telephone No. - N° de téléphone FAX No. - N° de FAX (613) 851-9981 ( ) ( ) - Destination - of Goods, Services, and Construction: Destination - des biens, services et construction: Specified Herein Précisé dans les présentes Comments - Commentaires Instructions: See Herein Instructions: Voir aux présentes Vendor/Firm Name and Address Raison sociale et adresse du fournisseur/de l'entrepreneur Delivery Required - Livraison exigée Delivery Offered - Livraison proposée See Herein – Voir ci-inclus Vendor/Firm Name and Address Raison sociale et adresse du fournisseur/de l'entrepreneur Telephone No. - N°de téléphone Facsimile No. - N° de télécopieur Issuing Office - Bureau de distribution Name and title of person authorized to sign on behalf of Vendor/Firm In-Service Support Marine / Soutien en Service Maritime (type or print) 11 Laurier St.