Anti-Anginal Drugs OBJECTIVES
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension
Reprinted from ANCIOLOCY Vol. 29, No. -I April 1978 Copyright 0 1978 Prinred in U.S.A. All Rights Rewrced Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension Eoin T. O'Brien DUBLIN, IRELAND General Measures Elevation of blood pressure should be regarded as one of a number of potential risk factors for cardiovascular disease-albeit a major risk factor- rather than a disease per se.' It is important to identify additional risk factors in the hypertensive patient, not only because collectively these factors may greatly magnify the cardiovascular risk, but also because modification of them may, of itself, lower the blood pressure and thus alleviate the risk and save the patient the inconvenience, expense, and potential harm that may result from even the simplest of drug regimes. Careful consideration should be given to the patient's diet (particularly in relation to the calorie intake in the case of obesity, the cholesterol and saturated fat content in the case of hyperlipidemia and patients at high risk, and the salt content) and to smoking habits, physical activity. stress. personality, and drug therapy, especially anovulant preparations. Other diseases, such as diabetes mellitus, which are associated with a high incidence of hypertension and pri- mary causes of hypertension must be excluded. Although there is still no statistical evidence to show that modification of these risk factors-with the exception of tobacco and anovulant preparations-will actually reduce mortal- ity, it does seem prudent on the basis of the evidence available to encourage the hypertensive patient to adjust his or her life-style not only to reduce the cardiovascular risk,2 but also because in many instances the mildly hypertensive patient will respond to this approach alone. -

Drug Class Review Antianginal Agents
Drug Class Review Antianginal Agents 24:12.08 Nitrates and Nitrites 24:04.92 Cardiac Drugs, Miscellaneous Amyl Nitrite Isosorbide Dinitrate (IsoDitrate ER®, others) Isosorbide Mononitrate (Imdur®) Nitroglycerin (Minitran®, Nitrostat®, others) Ranolazine (Ranexa®) Final Report May 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Antianginal Therapies .............................................................................................. 4 Table 2. Summary of Agents .................................................................................................. 5 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Clinical Practice Guidelines .................................................... 9 Pharmacology ............................................................................................................................... 10 Table 4. Pharmacokinetic Properties -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

CORGARD® TABLETS Nadolol Tablets USP
CORGARD® TABLETS Nadolol Tablets USP Rx Only DESCRIPTION CORGARD (nadolol) is a synthetic nonselective beta-adrenergic receptor blocking agent designated chemically as 1-(tert-butylamino)-3-[(5,6,7,8-tetrahydro-cis-6,7-dihydroxy-1- naphthyl)oxy]-2-propanol. Structural formula: C17H27NO4 MW 309.40 Nadolol is a white crystalline powder. It is freely soluble in ethanol, soluble in hydrochloric acid, slightly soluble in water and in chloroform, and very slightly soluble in sodium hydroxide. CORGARD (nadolol) is available for oral administration as 20 mg, 40 mg, and 80 mg tablets. Inactive ingredients: microcrystalline cellulose, colorant (FD&C Blue No. 2), corn starch, magnesium stearate, povidone (except 20 mg and 40 mg), and other ingredients. CLINICAL PHARMACOLOGY CORGARD (nadolol) is a nonselective beta-adrenergic receptor blocking agent. Clinical pharmacology studies have demonstrated beta-blocking activity by showing (1) reduction in heart rate and cardiac output at rest and on exercise, (2) reduction of systolic and diastolic blood pressure at rest and on exercise, (3) inhibition of isoproterenol-induced tachycardia, and (4) reduction of reflex orthostatic tachycardia. CORGARD (nadolol) specifically competes with beta-adrenergic receptor agonists for available beta receptor sites; it inhibits both the beta1 receptors located chiefly in cardiac muscle and the beta2 receptors located chiefly in the bronchial and vascular musculature, inhibiting the chronotropic, inotropic, and vasodilator responses to beta-adrenergic stimulation proportionately. CORGARD has no intrinsic sympathomimetic activity and, unlike some other beta-adrenergic blocking agents, nadolol has little direct myocardial depressant activity and does not have an anesthetic-like membrane- stabilizing action. Animal and human studies show that CORGARD slows the sinus rate and depresses AV conduction. -

Antianginal Drugs
Antianginal Drugs Angina medications are used for angina pectoris or chest pain. The types of chest pain are chronic stable angina (which is associated with atherosclerosis), unstable angina (early stage of progressive coronary artery disease), and vasospastic angina (which results from spasms in the layer of smooth muscle that surrounds atherosclerotic coronary arteries). The three main classes of drugs used to treat angina pectoris are nitrates and nitrites, beta-blockers, and calcium channel blockers. The goal of the treatment is: 1. Minimize the frequency of attacks and decrease the duration and intensity of angina pain 2. Improve the patient’s functional capacity with as few adverse effects as possible 3. Increase blood flow to ischemic heart muscle and decrease myocardial oxygen demand 4. Prevent or delay the worst possible outcome, which is a myocardial infarction Nitrates and Nitrites Nitrates are available on many forms including sublingual, chewable tablets, oral capsules/tablets, IV solutions, transdermal patches, ointments and translingual sprays. They are broken down into rapid-acting forms and long-acting forms. The rapid-acting forms include sublingual and IV solutions. These are used to treat acute angina attacks. The long-acting forms are used to prevent angina episodes. Mechanism of Action Nitrates dilate all blood vessels; however, they predominately affect venous vascular beds and have a dose-dependent arterial vasodilator effect. This vasodilation happens because of relaxation of smooth muscle cells. 1. Vasodilation results in reduced myocardial oxygen demand and therefore more oxygen to ischemic myocardial tissue and reduction of angina symptoms. 2. By causing venous dilation, the nitrates reduce venous return and in turn reduce the leftventricular end-diastolic volume (preload) and results in a lower left ventricular pressure. -

Effects of Vasodilation and Arterial Resistance on Cardiac Output Aliya Siddiqui Department of Biotechnology, Chaitanya P.G
& Experim l e ca n i t in a l l C Aliya, J Clinic Experiment Cardiol 2011, 2:11 C f a Journal of Clinical & Experimental o r d l DOI: 10.4172/2155-9880.1000170 i a o n l o r g u y o J Cardiology ISSN: 2155-9880 Review Article Open Access Effects of Vasodilation and Arterial Resistance on Cardiac Output Aliya Siddiqui Department of Biotechnology, Chaitanya P.G. College, Kakatiya University, Warangal, India Abstract Heart is one of the most important organs present in human body which pumps blood throughout the body using blood vessels. With each heartbeat, blood is sent throughout the body, carrying oxygen and nutrients to all the cells in body. The cardiac cycle is the sequence of events that occurs when the heart beats. Blood pressure is maximum during systole, when the heart is pushing and minimum during diastole, when the heart is relaxed. Vasodilation caused by relaxation of smooth muscle cells in arteries causes an increase in blood flow. When blood vessels dilate, the blood flow is increased due to a decrease in vascular resistance. Therefore, dilation of arteries and arterioles leads to an immediate decrease in arterial blood pressure and heart rate. Cardiac output is the amount of blood ejected by the left ventricle in one minute. Cardiac output (CO) is the volume of blood being pumped by the heart, by left ventricle in the time interval of one minute. The effects of vasodilation, how the blood quantity increases and decreases along with the blood flow and the arterial blood flow and resistance on cardiac output is discussed in this reviewArticle. -

Endogenous Estradiol in Elderly Individuals Cognitive and Noncognitive Associations
ORIGINAL CONTRIBUTION Endogenous Estradiol in Elderly Individuals Cognitive and Noncognitive Associations V. Senanarong, MD; S. Vannasaeng, MD; N. Poungvarin, MD; S. Ploybutr, MSC; S. Udompunthurak, MSC; P. Jamjumras, RN; L. Fairbanks, PhD; J. L. Cummings, MD Objective: To investigate an association between en- the Functional Assessment Questionnaire was used to as- dogenous estradiol (E2) levels and cognition and behav- sess instrumental activities of daily living. ior in elderly individuals. Results: There was no correlation between age and level of E2 in either men or women. Individuals with lower estro- Patients: We studied 135 community-based men and genlevelshadmorebehavioraldisturbances(men:r=−0.467, women aged 52 to 85 years in urban Bangkok, Thai- n=45;P=.001;women:r=−0.384,n=90;PϽ.001)andworse land; 72 had dementia and 63 did not. cognition (men: r=0.316, n=45; P=.03; women: r=0.243, n=90; P=.02) and function (men: r=−0.417, n=45; P=.004; women: r=−0.437, n=90; PϽ.001). The threshold level of Materials and Methods: Dementia was diagnosed endogenous E2 in elderly individuals for the risk of devel- using Diagnostic and Statistical Manual of Mental Disor- oping dementia was less than 15 pg/mL (Ͻ55 pmol/L) in ders, Fourth Edition, criteria after appropriate investiga- men and less than 1 pg/mL (Ͻ4 pmol/L) in women. tions. Blood samples for assay were collected in the morn- ing after 6 hours of fasting. Levels of E2 were measured Conclusion: Lower E2 levels are correlated with poor cog- by radioimmunoassay (double antibody technique). -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

0Bcore Safety Profile
Core Safety Profile Active substance: Levobunolol Pharmaceutical form(s)/strength: Eye drops solution/ 0,1%; 0,25%; 0,5%; 0,5% UD P-RMS: CZ/H/PSUR/0006/001 Date of FAR: 26.05.2009 4.2 Posology and method of administration Adults (including the elderly) Country specific posology and method of administration to be included. Children /.../ is not recommended for use in children due to lack of safety and efficacy data. If required, /.../ may be used with other agents to lower intra-ocular pressure. The use of two topical beta-adrenergic blocking agents is not recommended (see section 4.4). Intraocular pressure should be measured approximately four weeks after starting treatment with /.../ as a return to normal ocular pressure can take a few weeks. As with any eye drops, to reduce possible systemic absorption, it is recommended that the lachrymal sac is compressed at the medial canthus (punctual occlusion) for one minute. This should be performed immediately following the instillation of each drop. Transfer from other beta-blocking treatment When another beta blocking agent is being used treatment must be discontinued after a full day of therapy. Start treatment with /.../ the next day with X drop of /.../ topically applied into the conjunctival sac in the affected eye(s). If /.../ is to replace a combination of anti-glaucoma products, only a single product should be removed at a time. Use in renal and hepatic impairment Levobunolol hydrochloride has not been studied in patients with hepatic or renal impairment. Therefore, caution should be used in treating such patients (see section 4.4). -

Metered-Dose Inhalers (Mdis): Anti-Cholinergic Drugs
Texas Vendor Drug Program Drug Use Criteria: Aerosolized Agents - Metered-Dose Inhalers (MDIs): Anti-Cholinergic Drugs Publication History 1. Developed January 1995. 2. Revised April 2021; March 2019; March 2017; November 2015; March 2014; August 2012; June 2012; October 2010; January 2008; January 2003; January 2002; January 2001; March 2000; January 2000; February 1999; February 1998; February 1997; August 1995. Notes: All criteria may be applied retrospectively. The information contained is for the convenience of the public. The Texas Health and Human Services Commission is not responsible for any errors in transmission or any errors or omissions in the document. Medications listed in the tables and non-FDA approved indications included in these retrospective criteria are not indicative of Vendor Drug Program formulary coverage. Prepared by: • Drug Information Service, UT Health San Antonio. • The College of Pharmacy, The University of Texas at Austin 1 1 Dosage 1.1 Adults Ipratropium (Atrovent®), a short-acting, inhalational anticholinergic agent, is FDA- approved to manage bronchospasm associated with chronic bronchitis and emphysema, collectively known as chronic obstructive pulmonary disease (COPD). Ipratropium is considered a second-line agent in the treatment of asthma as the bronchodilatory effects seen with ipratropium are less than those seen with beta- adrenergic drugs. While not FDA approved, the Expert Panel 3 guidelines from the National Heart Lung and Blood Institute document benefit when multiple ipratropium doses are administered adjunctively with beta2-agonists in the emergency department to manage more severe acute asthma exacerbations, and the Global Initiative for Asthma (GINA) guidelines state that ipratropium may be considered an alternative bronchodilator in patients who experience adverse effects to short-acting beta2-agonists (e.g., tachycardia, arrhythmia, tremor). -
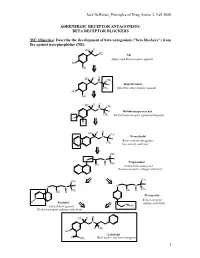
BETA RECEPTOR BLOCKERS MC Objective
Jack DeRuiter, Principles of Drug Action 2, Fall 2000 ADRENERGIC RECEPTOR ANTAGONISTS: BETA RECEPTOR BLOCKERS MC Objective: Describe the development of beta antagonists ("beta blockers") from the agonist norepinephrine (NE): HO H NH2 NE Alpha- and Beta-receptor agonist HO OH H H HO CH N 3 H Isoproterenol CH3 Selective beta-receptor agonist HO OH H H HO CH N 3 H Dichloroisoproterenol CH3 Partial beta-receptor agonist/antagonist Cl Cl H H HO CH N 3 Pronethalol H Beta-receptor antagonist, CH 3 low activity and toxic CH3 O N H Propranolol CH3 OH H Potent beta-antagonist No beta-receptor subtype selectivity CH3 CH3 O N H O N H CH CH OH H 3 OH H 3 Metoprolol N Beta-1-receptor H Pindolol O subtype selectivity Partial beta-agonist CH3 No beta-receptor subtype selectivity HO H H N H CH3 HO Labetolol O NH2 Dual alpha- and beta-antagonst 1 Jack DeRuiter, Principles of Drug Action 2, Fall 2000 MC Objective: Based on their structures, would the beta-blockers be expected to be relatively receptor selective? YES. They do not produce significant blockade of alpha- adrenergic receptors (alpha-1 or alpha-2), histamine receptors, muscarinic receptors or dopamine receptors. MC/PC Objective: Identify which beta blockers are classified as "non-selective": · The “non-selective" classification refers to those beta-blockers capable of blocking BOTH beta-1 and beta-2 receptors with equivalent efficacy. These drugs DO NOT have clinically significant affinity for other neurotransmitter receptors (alpha, dopamine, histamine, acetylcholine, etc.). · ALL of these beta-blockers (except satolol) consist of an aryloxypropanolamine side chain linked to an aromatic or “heteroaromatic” ring which is “ortho” substituted. -

Therapeutic Drug Class
BUREAU FOR MEDICAL SERVICES EFFECTIVE WEST VIRGINIA MEDICAID PREFERRED DRUG LIST WITH PRIOR AUTHORIZATION CRITERIA 07/01/2018 This is not an all-inclusive list of available covered drugs and includes only Version 2018.3e managed categories. Refer to cover page for complete list of rules governing this PDL. • Prior authorization for a non-preferred agent in any class will be given only if there has been a trial of the preferred brand/generic equivalent or preferred formulation of the active ingredient, at a therapeutic dose, that resulted in a partial response with a documented intolerance. • Prior authorization of a non-preferred isomer, pro-drug, or metabolite will be considered with a trial of a preferred parent drug of the same chemical entity, at a therapeutic dose, that resulted in a partial response with documented intolerance or a previous trial and therapy failure, at a therapeutic dose, with a preferred drug of a different chemical entity indicated to treat the submitted diagnosis. (The required trial may be overridden when documented evidence is provided that the use of these preferred agent(s) would be medically contraindicated.) • Unless otherwise specified, the listing of a particular brand or generic name includes all legend forms of that drug. OTC drugs are not covered unless specified. • PA criteria for non-preferred agents apply in addition to general Drug Utilization Review policy that is in effect for the entire pharmacy program, including, but not limited to, appropriate dosing, duplication of therapy, etc. • The use of pharmaceutical samples will not be considered when evaluating the members’ medical condition or prior prescription history for drugs that require prior authorization.