Beta-Blockers for Hypertension: Time to Call a Halt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Angiotensin-Converting Enzyme (ACE) Inhibitors Single Entity Agents
Therapeutic Class Overview Angiotensin-Converting Enzyme (ACE) Inhibitors Single Entity Agents Therapeutic Class Overview/Summary: The renin-angiotensin-aldosterone system (RAAS) is the most important component in the homeostatic regulation of blood pressure.1,2 Excessive activity of the RAAS may lead to hypertension and disorders of fluid and electrolyte imbalance.3 Renin catalyzes the conversion of angiotensinogen to angiotensin I. Angiotensin I is then cleaved to angiotensin II by angiotensin- converting enzyme (ACE). Angiotensin II may also be generated through other pathways (angiotensin I convertase).1 Angiotensin II can increase blood pressure by direct vasoconstriction and through actions on the brain and autonomic nervous system.1,3 In addition, angiotensin II stimulates aldosterone synthesis from the adrenal cortex, leading to sodium and water reabsorption. Angiotensin II exerts other detrimental cardiovascular effects including ventricular hypertrophy, remodeling and myocyte apoptosis.1,2 The ACE inhibitors block the conversion of angiotensin I to angiotensin II, and also inhibit the breakdown of bradykinin, a potent vasodilator.4 Evidence-based guidelines recognize the important role that ACE inhibitors play in the treatment of hypertension and other cardiovascular and renal diseases. With the exception of Epaned® (enalapril solution) and Qbrelis® (lisinopril solution), all of the ACE inhibitors are available generically. Table 1. Current Medications Available in Therapeutic Class5-19 Generic Food and Drug Administration -
Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension
Reprinted from ANCIOLOCY Vol. 29, No. -I April 1978 Copyright 0 1978 Prinred in U.S.A. All Rights Rewrced Advantages and Disadvantages of Beta- Adrenergic Blocking Drugs in Hypertension Eoin T. O'Brien DUBLIN, IRELAND General Measures Elevation of blood pressure should be regarded as one of a number of potential risk factors for cardiovascular disease-albeit a major risk factor- rather than a disease per se.' It is important to identify additional risk factors in the hypertensive patient, not only because collectively these factors may greatly magnify the cardiovascular risk, but also because modification of them may, of itself, lower the blood pressure and thus alleviate the risk and save the patient the inconvenience, expense, and potential harm that may result from even the simplest of drug regimes. Careful consideration should be given to the patient's diet (particularly in relation to the calorie intake in the case of obesity, the cholesterol and saturated fat content in the case of hyperlipidemia and patients at high risk, and the salt content) and to smoking habits, physical activity. stress. personality, and drug therapy, especially anovulant preparations. Other diseases, such as diabetes mellitus, which are associated with a high incidence of hypertension and pri- mary causes of hypertension must be excluded. Although there is still no statistical evidence to show that modification of these risk factors-with the exception of tobacco and anovulant preparations-will actually reduce mortal- ity, it does seem prudent on the basis of the evidence available to encourage the hypertensive patient to adjust his or her life-style not only to reduce the cardiovascular risk,2 but also because in many instances the mildly hypertensive patient will respond to this approach alone. -

Drug Class Review Antianginal Agents
Drug Class Review Antianginal Agents 24:12.08 Nitrates and Nitrites 24:04.92 Cardiac Drugs, Miscellaneous Amyl Nitrite Isosorbide Dinitrate (IsoDitrate ER®, others) Isosorbide Mononitrate (Imdur®) Nitroglycerin (Minitran®, Nitrostat®, others) Ranolazine (Ranexa®) Final Report May 2015 Review prepared by: Melissa Archer, PharmD, Clinical Pharmacist Carin Steinvoort, PharmD, Clinical Pharmacist Gary Oderda, PharmD, MPH, Professor University of Utah College of Pharmacy Copyright © 2015 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved. Table of Contents Executive Summary ......................................................................................................................... 3 Introduction .................................................................................................................................... 4 Table 1. Antianginal Therapies .............................................................................................. 4 Table 2. Summary of Agents .................................................................................................. 5 Disease Overview ........................................................................................................................ 8 Table 3. Summary of Current Clinical Practice Guidelines .................................................... 9 Pharmacology ............................................................................................................................... 10 Table 4. Pharmacokinetic Properties -

COPD Agents Review – October 2020 Page 2 | Proprietary Information
COPD Agents Therapeutic Class Review (TCR) October 1, 2020 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. October 2020 -

CORGARD® TABLETS Nadolol Tablets USP
CORGARD® TABLETS Nadolol Tablets USP Rx Only DESCRIPTION CORGARD (nadolol) is a synthetic nonselective beta-adrenergic receptor blocking agent designated chemically as 1-(tert-butylamino)-3-[(5,6,7,8-tetrahydro-cis-6,7-dihydroxy-1- naphthyl)oxy]-2-propanol. Structural formula: C17H27NO4 MW 309.40 Nadolol is a white crystalline powder. It is freely soluble in ethanol, soluble in hydrochloric acid, slightly soluble in water and in chloroform, and very slightly soluble in sodium hydroxide. CORGARD (nadolol) is available for oral administration as 20 mg, 40 mg, and 80 mg tablets. Inactive ingredients: microcrystalline cellulose, colorant (FD&C Blue No. 2), corn starch, magnesium stearate, povidone (except 20 mg and 40 mg), and other ingredients. CLINICAL PHARMACOLOGY CORGARD (nadolol) is a nonselective beta-adrenergic receptor blocking agent. Clinical pharmacology studies have demonstrated beta-blocking activity by showing (1) reduction in heart rate and cardiac output at rest and on exercise, (2) reduction of systolic and diastolic blood pressure at rest and on exercise, (3) inhibition of isoproterenol-induced tachycardia, and (4) reduction of reflex orthostatic tachycardia. CORGARD (nadolol) specifically competes with beta-adrenergic receptor agonists for available beta receptor sites; it inhibits both the beta1 receptors located chiefly in cardiac muscle and the beta2 receptors located chiefly in the bronchial and vascular musculature, inhibiting the chronotropic, inotropic, and vasodilator responses to beta-adrenergic stimulation proportionately. CORGARD has no intrinsic sympathomimetic activity and, unlike some other beta-adrenergic blocking agents, nadolol has little direct myocardial depressant activity and does not have an anesthetic-like membrane- stabilizing action. Animal and human studies show that CORGARD slows the sinus rate and depresses AV conduction. -

Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss
Supplemental Material can be found at: /content/suppl/2020/12/18/73.1.202.DC1.html 1521-0081/73/1/202–277$35.00 https://doi.org/10.1124/pharmrev.120.000056 PHARMACOLOGICAL REVIEWS Pharmacol Rev 73:202–277, January 2021 Copyright © 2020 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: MICHAEL NADER Psychedelics in Psychiatry: Neuroplastic, Immunomodulatory, and Neurotransmitter Mechanismss Antonio Inserra, Danilo De Gregorio, and Gabriella Gobbi Neurobiological Psychiatry Unit, Department of Psychiatry, McGill University, Montreal, Quebec, Canada Abstract ...................................................................................205 Significance Statement. ..................................................................205 I. Introduction . ..............................................................................205 A. Review Outline ........................................................................205 B. Psychiatric Disorders and the Need for Novel Pharmacotherapies .......................206 C. Psychedelic Compounds as Novel Therapeutics in Psychiatry: Overview and Comparison with Current Available Treatments . .....................................206 D. Classical or Serotonergic Psychedelics versus Nonclassical Psychedelics: Definition ......208 Downloaded from E. Dissociative Anesthetics................................................................209 F. Empathogens-Entactogens . ............................................................209 -

Interaction of the Sympathetic Nervous System with Other Pressor Systems in Antihypertensive Therapy
Journal of Clinical and Basic Cardiology An Independent International Scientific Journal Journal of Clinical and Basic Cardiology 2001; 4 (3), 185-192 Interaction of the Sympathetic Nervous System with other Pressor Systems in Antihypertensive Therapy Wenzel RR, Baumgart D, Bruck H, Erbel R, Heemann U Mitchell A, Philipp Th, Schaefers RF Homepage: www.kup.at/jcbc Online Data Base Search for Authors and Keywords Indexed in Chemical Abstracts EMBASE/Excerpta Medica Krause & Pachernegg GmbH · VERLAG für MEDIZIN und WIRTSCHAFT · A-3003 Gablitz/Austria FOCUS ON SYMPATHETIC TONE Interaction of SNS J Clin Basic Cardiol 2001; 4: 185 Interaction of the Sympathetic Nervous System with Other Pressor Systems in Antihypertensive Therapy R. R. Wenzel1, H. Bruck1, A. Mitchell1, R. F. Schaefers1, D. Baumgart2, R. Erbel2, U. Heemann1, Th. Philipp1 Regulation of blood pressure homeostasis and cardiac function is importantly regulated by the sympathetic nervous system (SNS) and other pressor systems including the renin-angiotensin system (RAS) and the vascular endothelium. Increases in SNS activity increase mortality in patients with hypertension, coronary artery disease and congestive heart failure. This review summarizes some of the interactions between the main pressor systems, ie, the SNS, the RAS and the vascular endothelium including the endothelin-system. Different classes of cardiovascular drugs interfere differently with the SNS and the other pressor systems. Beta-blockers, ACE-inhibitors and diuretics have no major effect on central SNS activity. Pure vasodilators including nitrates, alpha-blockers and DHP-calcium channel blockers increase SNS activity. In contrast, central sympatholytic drugs including moxonidine re- duce SNS activity. The effects of angiotensin-II receptor antagonist on SNS activity in humans are not clear, experimental data are discussed in this review. -

Effect of Exogenous Glucocorticoid on Osmotically Stimulated Antidiuretic
European Journal of Endocrinology (2006) 155 845–848 ISSN 0804-4643 CLINICAL STUDY Effect of exogenous glucocorticoid on osmotically stimulated antidiuretic hormone secretion and on water reabsorption in man Volker Ba¨hr1, Norma Franzen1, Wolfgang Oelkers2, Andreas F H Pfeiffer1 and Sven Diederich1,2 1Department of Endocrinology, Diabetes and Nutrition, Charite-Universitatsmedizin Berlin, Campus Benjamin Franklin, Hindenburgdamm 30, 12200 Berlin, Germany and 2Endokrinologikum Berlin, Centre for Endocrine and Metabolic Diseases, Berlin, Germany (Correspondence should be addressed to V Ba¨hr; Email: [email protected]) Abstract Objective: Glucocorticoids exert tonic suppression of antidiuretic hormone (ADH) secretion. Hypocortisolism in secondary adrenocortical insufficiency can result in a clinical picture similar to the syndrome of inappropriate ADH secretion. On the other hand, in vitro and in vivo results provide evidence for ADH suppression in states of hypercortisolism. To test the hypothesis that ADH suppression is of relevance during glucocorticoid therapy, we investigated the influence of prednisolone on the osmotic stimulation of ADH. Design and methods: Seven healthy men were subjected to water deprivation tests with the measurement of plasma ADH (pADH) and osmolality (posmol) before and after glucocorticoid treatment (5 days 30 mg prednisolone per day). Results: Before glucocorticoid treatment, the volunteers showed a normal test with an adequate increase of pADH (basal 0.54G0.2 to 1.9G0.72 pg/ml (meanGS.D.)) in relation to posmol(basal 283.3G8.5 to 293.7G6 mosmol/kg). After prednisolone intake, pADH was attenuated (!0.4 pg/ml) in spite of an increase of posmol from 289.3G3.6 to 297.0G5.5 mosmol/kg. -
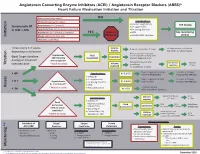
Initiation Titration Assess Monitoring **
Angiotensin Converting Enzyme Inhibitors (ACEI) / Angiotensin Receptor Blockers (ARBS)* Heart Failure Medication Initiation and Titration Bilateral renal artery stenosis NO Moderate/Severe aortic stenosis Considerations: • Baseline cough (ACEi) Hyperkalemia: K+ > 5.2 mmol/L See dosing Symptomatic HF • K+ supplements or LVEF < 40% Renal Dysfunction:Serum creatinine >220 µmol/L • K+ sparing diuretics Hypotension: SBP < 90 mmHg or symptoms YES Refer to • MRA See monitoring Initiation Allergy: angioedema, hives, rash Physician • NSAIDS/COX2 inhibitors section Intolerance: cough (ACEi) Titrate every 1-3 weeks, Volume Reduce/hold diuretic x 2-3 days No improvement, hold/reduce depending on tolerance deplete ACEI/ARB x 1-2 wks & reassess Reassess diuretic dose/other Hypotension Fluid non-essential BP lowering meds Goal: Target dose(see Euvolemic SBP<90mmHg Assessment Consider staggering doses dosing) or maximum with symptoms* Reduce/hold dose of other See Diuretic Reassess Titration * Watch for trends Volume tolerated dose vasodilators algorithm 1-2 wks overload +/- ACEI/ARB x 1-2 weeks Stop K+ supplements, reduce/ Serum K+ in 3-5 days, Considerations: • BP K+ 5.2-5.5 hold MRA (if applicable) Reassess ACEI/ARB dose • Dietary K+ • K+ supplements Stop K+ supplements, MRA. Serum K+ in 2-3 days, • K + Hyperkalemia • K+ sparing diuretics K+ 5.6-6.0 hold ACEI/ARB Reassess ACEI/ARB dose K+ > 5.2 mmol/L* • MRA Assess * Watch for trends • Renal dysfunction Treat hyperkalemia • Scr K+ > 6.0 Refer to MD/NP +/- send to ED Reduce/hold diuretic Scr in Considerations: -

3. Diuretics for Hypertension-A Review and Update
REVIEW Diuretics for Hypertension: A Review and Update George C. Roush1 and Domenic A. Sica2 Downloaded from https://academic.oup.com/ajh/article-abstract/29/10/1130/2622231 by Xenia Agorogianni user on 17 July 2019 This review and update focuses on the clinical features of hydrochlo- ectopy and reduce the risk for sudden cardiac death relative to thi- rothiazide (HCTZ), the thiazide-like agents chlorthalidone (CTDN) and azide-type diuretics used alone. A recent synthesis of 44 trials has indapamide (INDAP), potassium-sparing ENaC inhibitors and aldos- shown that the relative potencies in milligrams among spironolac- terone receptor antagonists, and loop diuretics. Diuretics are the sec- tone (SPIR), amiloride, and eplerenone (EPLER) are approximately ond most commonly prescribed class of antihypertensive medication, from 25 to 10 to 100, respectively, which may be important when SPIR and thiazide-related diuretics have increased at a rate greater than is poorly tolerated. SPIR reduces proteinuria beyond that provided by that of antihypertensive medications as a whole. The latest hyper- other renin angiotensin aldosterone inhibitors. EPLER also reduces tension guidelines have underscored the importance of diuretics for proteinuria and has beneficial effects on endothelial function. While all patients, but particularly for those with salt-sensitive and resist- guidelines often do not differentiate among specific diuretics, this ant hypertension. HCTZ is 4.2–6.2 systolic mm Hg less potent than review demonstrates that these distinctions are important for man- CTDN, angiotensin-converting enzyme inhibitors, beta blockers, and aging hypertension. calcium channel blockers by 24-hour measurements and 5.1 mm Hg systolic less potent than INDAP by office measurements. -

Calcium Channel Blockers
Calcium Channel Blockers Summary In general, calcium channel blockers (CCBs) are used most often for the management of hypertension and angina. There are 2 classes of CCBs: the dihydropyridines (DHPs), which have greater selectivity for vascular smooth muscle cells than for cardiac myocytes, and the non-DHPs, which have greater selectivity for cardiac myocytes and are used for cardiac arrhythmias. The DHPs cause peripheral edema, headaches, and postural hypotension most commonly, all of which are due to the peripheral vasodilatory effects of the drugs in this class of CCBs. The non-DHPs are negative inotropes and chronotropes; they can cause bradycardia and depress AV node conduction, increasing the risk of heart failure exacerbation, bradycardia, and AV block. Clevidipine is a DHP calcium channel blocker administered via continuous IV infusion and used for rapid blood pressure reductions. All CCBs are substrates of CYP3A4, but both diltiazem and verapamil are also inhibitors of 3A4 and have an increased risk of drug interactions. Verapamil also inhibits CYP2C9, CYP2C19, and CYP1A2. Pharmacology CCBs selectively inhibit the voltage-gated L-type calcium channels on cardiac myocytes, vascular smooth muscle cells, and cells within the sinoatrial (SA) and atrioventricular (AV) nodes, preventing influx of extracellular calcium. CCBs act by either deforming the channels, inhibiting ion-control gating mechanisms, and/or interfering with the release of calcium from the major cellular calcium store, the endoplasmic reticulum. Calcium influx via these channels serves for excitation-contraction coupling and electrical discharge in the heart and vasculature. A decrease in intracellular calcium will result in inhibition of the contractile process of the myocardial smooth muscle cells, resulting in dilation of the coronary and peripheral arterial vasculature. -

Energy Drinks 800.232.4424 (Voice/TTY) 860.793.9813 (Fax)
Caffeine and Energy Boosting Drugs: Energy Drinks 800.232.4424 (Voice/TTY) 860.793.9813 (Fax) www.ctclearinghouse.org A Library and Resource Center on Alcohol, Tobacco, Other Drugs, Mental Health and Wellness What are energy drinks? you. You wouldn't use Mountain Dew as a sports Energy drinks are beverages like drink. And a drink like Red Bull and vodka is Red Bull, Venom, Adrenaline Rush, more like strong coffee and whisky than 180, ISO Sprint, and Whoopass, anything else. which contain large doses of caffeine and other legal stimulants What happens when energy drinks are like ephedrine, guarana, and ginseng. combined with alcohol? Energy drinks may contain as much as 80 mg. Energy drinks are also used as mixers with of caffeine, the equivalent of a cup of coffee. alcohol. This combination carries a number of Compared to the 37 mg. of caffeine in a dangers: Mountain Dew, or the 23 mg. in a Coca-Cola Classic, that's a big punch. These drinks are • Since energy drinks are stimulants and marketed to people under 30, especially to alcohol is a depressant, the combination of college students, and are widely available both effects may be dangerous. The stimulant on and off campus. effects can mask how intoxicated you are and prevent you from realizing how much Are there short-term dangers to drinking alcohol you have consumed. Fatigue is one energy drinks? of the ways the body normally tells Individual responses to caffeine vary, and someone that they've had enough to drink. these drinks should be treated carefully • The stimulant effect can give the person the because of how powerful they are.