The Capsulotomy: from There to Where?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wildlife Ophthalmology
Wildlife Ophthalmology DR. HEATHER REID TORONTO WILDLIFE CENTRE TORONTO, ON CANADA Why understand eyes? Wildlife need to have excellent vision to survive in the wild Eye related problems are common in wildlife admitted to rehabilitation centers What we will cover Anatomy of the eye Differences between birds and mammals The eye exam Recognizing common problems Prognosis Treatment options When to see the vet Anatomy Around the Eye: Muscles & nerves Skin Eye lids Nictitating eyelid Conjunctiva & sclera Tear glands & ducts Ossicles (birds) Anatomy Front of the Eye: Cornea Iris Pupil Ciliary body Anterior Chamber Aqueous humor Anatomy Back of the Eye: Lens Retina Optic nerve Choroid Pecten (birds) Posterior Chamber Vitreous humor Fundus of the Eye Mammal Eye Bird Eye The Avian Eye - Differences Small eye size in most birds and small pupil size makes it hard to examine Can control the size of their pupil Lower eyelid more developed The nictitating membrane spreads the tears allowing birds to blink less Moves horizontally across eye The Avian Eye - Differences Eyes are not as protected by skull Less muscles around eye so less eye movement Boney ossicles support the eye Three main eye shapes; flat, globose & tubular The Avian Eye - Differences Four different color receptors compared to the three in mammals means better color detail Can see in the ultraviolet range Higher flicker rate – can detect lights that flicker at more than 100 flashes per second (humans detect at 50) The Avian Eye - Differences In some species the eye -

Utah Eye Centers Now Offers the Latest Advance in Laser Eye Surgery
Mark G. Ballif, M.D. Scott O. Sykes, M.D. Michael B. Wilcox, M.D. John D. Armstrong, M.D. Robert W. Wing, M.D., FACS Keith Linford, O.D. Jed T. Poll, M.D. Claron D. Alldredge, M.D. Devin B. Farr, O.D. Michael L. Bullard, M.D. Court R. Wilkins, O.D. Utah Eye Centers Now Offers the Latest Advance In Laser Eye Surgery The New VICTUS® Femtosecond Laser Platform, from Bausch + Lomb is Designed to Support Positive Patient Experience and Outstanding Visual Results in Cataract and LASIK Procedures FOR RELEASE April 17, 2015 Ogden, Utah— Utah Eye Centers, the leading comprehensive ophthalmology practice in northern Utah, announced today the Mount Ogden facility now offers eye surgery for cataracts and LASIK with an advanced laser system, the VICTUS® femtosecond laser platform. They are the only practice north of Salt Lake City with a fixed site femtosecond laser for cataracts and LASIK. The versatile VICTUS platform is designed to provide greater precision compared to manual cataract and LASIK surgery techniques. According to Scott Sykes, M.D., the Victus laser is the only laser approved to perform treatments for both cataract and LASIK surgeries. "With the VICTUS platform, we are able to automate some of the steps that we have commonly performed manually," said Mark Ballif, M.D. "While we have performed thousands of successful cataract and LASIK surgeries, the VICTUS platform helps us to improve the procedures to give our patients the best outcomes possible." The VICTUS platform features a sophisticated, curved patient interface with computer-monitored pressure sensors designed to provide comfort during the procedure. -

Nd:YAG CAPS ULOTOMY AS a PRIMARY TREATMENT
PSEUDOPHAKIC MALIGNANT GLAUCOMA: Nd:YAG CAPS ULOTOMY AS A PRIMARY TREATMENT B. C. LITTLE and R. A. HITCHINGS London SUMMARY anisms of ciliolenticular block of aqueous flow leading to Malignant glaucoma is one of the most serious but rare the misdirection of aqueous posteriorly into or in front of complications of anterior segment surgery. It is best the vitreous gel leading to the characteristic diffuse shal known following trabeculectomy but has been reported lowing of the anterior chamber accompanied by a precipi following a wide variety of anterior segment procedures tous rise in intraocular pressure. The mechanistic including extracapsular cataract extraction with pos understanding of its pathogenesis has led to the use of the terior chamber lens implantation. It is notoriously refrac synonyms 'ciliolenticular block',7 'ciliovitreal block', tory to medical treatment alone and surgical intervention 'iridovitreal block',8 'aqueous misdirection' and 'aqueous has had only limited success. An additional treatment diversion syndrome'. Although probably more precise option in pseudophakic eyes is that of peripheral these are unlikely to succeed the original term 'malignant Nd:YAG posterior capsulotomy, which is minimally glaucoma', which more accurately evokes the fulminant invasive and can re-establish forward flow of posteriorly nature of the condition as well as the justified anxiety asso misdirected aqueous through into the drainage angle of ciated with it. Medical treatment alone is rarely successful the anterior chamber. We report our experience of seven in establishing control of the intraocular pressure.2•8 Pars cases of malignant glaucoma in pseudophakic eyes and of plana vitrectomy has been used in the surgical managment the successful use of Nd:YAG posterior capsulotomy in of malignant glaucoma with some definite but limited suc re-establishing pressure control in' five of these eyes, cess in phakic as well as pseudophakic eyes.9•10 thereby obviating the need for acute surgical However, when malignant glaucoma develops in intervention. -

Outcome of Lens Aspiration and Intraocular Lens Implantation in Children Aged 5 Years and Under
540 Br J Ophthalmol 2001;85:540–542 Outcome of lens aspiration and intraocular lens implantation in children aged 5 years and under Lorraine Cassidy, Jugnoo Rahi, Ken Nischal, Isabelle Russell-Eggitt, David Taylor Abstract However, final refraction is variable, such that Aims—To determine the visual outcome emmetropia in adulthood cannot be guaran- and complications of lens aspiration with teed, as there are insuYcient long term studies. intraocular lens implantation in children There have been many reports of the visual aged 5 years and under. outcome and complications of posterior cham- Methods—The hospital notes of all chil- ber lens implantation in children.4–12 Most of dren aged 5 years and under, who had these have been based on older children, undergone lens aspiration with intraocu- secondary lens implants, a high number of lar lens implantation between January traumatic cataracts, and many have reported 1994 and September 1998, and for whom early outcome. We report visual outcome and follow up data of at least 1 year were avail- complications of primary IOL implantation at able, were reviewed. least 1 year after surgery, in children aged 5 Results—Of 50 children who underwent years and under, with mainly congenital or surgery, 45 were eligible based on the juvenile lens opacities. follow up criteria. 34 children had bilat- eral cataracts and, of these, 30 had surgery Methods on both eyes. Cataract was unilateral in 11 SUBJECTS cases; thus, 75 eyes of 45 children had sur- We reviewed the notes of all children aged 5 gery. Cataracts were congenital in 28 years and under, who had undergone lens aspi- cases, juvenile in 16, and traumatic in one ration with primary posterior chamber in- case. -

Laser Learning Lecture and Lab: YAG Caps, LPI, And
5/9/17 Overview Laser Learning Lecture and Lab: • Why we use lasers YAG caps, LPI, and SLT • YAG capsulotomy • Laser Peripheral Iridotomy (LPI or PI) Aaron McNulty, O.D., F.A.A.O. • Argon Laser Peripheral Iridoplasty (ALPI) Nate Lighthizer, O.D., F.A.A.O. • Argon Laser Trabeculoplasty (ALT) • Selective Laser Trabeculoplasty (SLT) • Other Laser Trabeculoplasty Why do we use lasers? Posterior Capsular Opacification (PCO) • Vision is decreased from PCO following cataract surgery • Lens capsular bag has an anterior and • Narrow angles/angle closure posterior surface • Glaucoma is progressing in a pt on max meds – Anterior surface usually removed w/ capsulorhexis – Something else needs to be done – Surgery not wanted yet • PCO is the formation of a cloudy membrane • Compliance issues on the posterior surface of the capsular bag • Cost issues following ECCE • Convenience issues – AKA: Secondary cataract • Doctor preference PCO YAG Laser • Incidence: • Nd: YAG laser – Most common complication of post ECCE – Neodymium: Yttrium aluminum garnet laser – 10-80% of eyes following cataract surgery – Can form anywhere from a few days to years post surgery • Tissue interaction: Photodisruptive laser – Younger patients higher risk of PCO – High light energy levels cause the tissues to be reduced – IOL’s to plasma, disintegrating the tissue • Silicone > acrylic – A large amount of energy is delivered into very small focal spots in a very brief duration of time • Prevention: • 4 nsec – – Capsulotomy during surgery No thermal reaction/No coagulation when bv’s are hit – Posterior capsular polishing – Pigment independent* 1 5/9/17 YAG Cap Risks, Complications, YAG Cap Pre-op Exam Contraindications • Visual acuity, glare testing, PAM/Heine lambda Contraindications Risks/complications – Vision 20/30 or worse 1. -

Smartphone-Based Dilated Fundus Photography and Near Visual Acuity Testing As Inexpensive Screening Tools to Detect Referral Warranted Diabetic Eye Disease
Smartphone-Based Dilated Fundus Photography and Near Visual Acuity Testing as Inexpensive Screening Tools to Detect Referral Warranted Diabetic Eye Disease BRIAN C. TOY, MD,*† DAVID J. MYUNG, MD, PHD,*† LINGMIN HE, MD,*† CAROLYN K. PAN, MD,*† ROBERT T. CHANG, MD,* ALISON POLKINHORNE, MA,‡ DOUGLAS MERRELL, BS,‡ DOUG FOSTER, MBA,‡ MARK S. BLUMENKRANZ, MD* Purpose: To compare clinical assessment of diabetic eye disease by standard dilated examination with data gathered using a smartphone-based store-and-forward teleoph- thalmology platform. Methods: 100 eyes of 50 adult patients with diabetes from a health care safety-net ophthalmology clinic. All patients underwent comprehensive ophthalmic examination. Concurrently, a smartphone was used to estimate near visual acuity and capture anterior and dilated posterior segment photographs, which underwent masked, standardized review. Quantitative comparison of clinic and smartphone-based data using descriptive, kappa, Bland-Altman, and receiver operating characteristic analyses was performed. Results: Smartphone visual acuity was successfully measured in all eyes. Anterior and posterior segment photography was of sufficient quality to grade in 96 and 98 eyes, respectively. There was good correlation between clinical Snellen and smartphone visual acuity measurements (rho = 0.91). Smartphone-acquired fundus photographs demon- strated 91% sensitivity and 99% specificity to detect moderate nonproliferative and worse diabetic retinopathy, with good agreement between clinic and photograph grades (kappa = 0.91 ± 0.1, P , 0.001; AUROC = 0.97, 95% confidence interval, 0.93–1). Conclusion: The authors report a smartphone-based telemedicine system that demon- strated sensitivity and specificity to detect referral-warranted diabetic eye disease as a proof-of-concept. Additional studies are warranted to evaluate this approach to expanding screening for diabetic retinopathy. -

Effects of Nd:YAG Laser Capsulotomy in Posterior Capsular Opacification
Original Research Article Effects of Nd:YAG laser capsulotomy in posterior capsular opacification Praveen Kumar G S1, Lavanya P2*, Raviprakash D3 1Assistant Professor, 2Associate Professor, 3Professor & HOD, Department of Ophthalmology, Shridevi institute of Medical Sciences and Research Hospital, Sira Road, NH-4 Bypass Road, Tumkur- 572106, INDIA. Email: [email protected] Abstract Background: Posterior capsular opacification (PCO) is the most common long-term complication of cataract surgery in both phacoemulsification and extracapsular cataract extraction (ECCE). The overall incidence of PCO and the incidence of neodymium-doped yttrium–aluminum–garnet (Nd:YAG) laser posterior capsulotomy has decreased from 50% in the 1980s and early 1990s to less than 10% today. Reported complications of Nd:YAG laser posterior capsulotomy include elevated intraocular pressure, iritis, corneal damage, intraocular lens (IOL) damage, cystoids macular edema, disruption of the anterior hyaloid surface, increased risk of retinal detachment, and IOL movement or dislocation. In some patients, a refraction change is noticed after Nd:YAG laser posterior capsulotomy, but proving this remains difficult. Materials and Methods: Nd; YAG LASER capsulotomy was performed in 200 eyes of 200 patients, some with pseudophakia and some with aphakia at Kurnool medical college, Kurnool. They were followed up between October 2008 and September 2010. Results: Elevation of IOP has been well documented after anterior segment laser procedures. The IOP rise after YAG laser posterior capsulotomy is of short duration starting about 1 hr after laser procedure and lasting for 24 hrs. In this study, in 1case IOP came down to normal level after 3 days and in another case after 7 days. -
Intraocular Lenses and Spectacle Correction
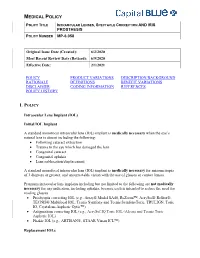
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

MEDICINAL PLANTS OPIUM POPPY: BOTANY, TEA: CULTIVATION to of NORTH AFRICA Opidjd CHEMISTRY and CONSUMPTION by Loutfy Boulos
hv'IERIGAN BCXtlNICAL COJNCIL -----New Act(uisition~---------l ETHNOBOTANY FLORA OF LOUISIANA Jllll!llll GUIDE TO FLOWERING FLORA Ed. by Richard E. Schultes and Siri of by Margaret Stones. 1991. Over PLANT FAMILIES von Reis. 1995. Evolution of o LOUISIANA 200 beautiful full color watercolors by Wendy Zomlefer. 1994. 130 discipline. Thirty-six chapters from and b/w illustrations. Each pointing temperate to tropical families contributors who present o tru~ accompanied by description, habitat, common to the U.S. with 158 globol perspective on the theory and and growing conditions. Hardcover, plates depicting intricate practice of todoy's ethnobotony. 220 pp. $45. #8127 of 312 species. Extensive Hardcover, 416 pp. $49.95. #8126 glossary. Hardcover, 430 pp. $55. #8128 FOLK MEDICINE MUSHROOMS: TAXOL 4t SCIENCE Ed. by Richard Steiner. 1986. POISONS AND PANACEAS AND APPLICATIONS Examines medicinal practices of by Denis Benjamin. 1995. Discusses Ed. by Matthew Suffness. 1995. TAXQL® Aztecs and Zunis. Folk medicine Folk Medicine signs, symptoms, and treatment of Covers the discovery and from Indio, Fup, Papua New Guinea, poisoning. Full color photographic development of Toxol, supp~. Science and Australia, and Africa. Active identification. Health and nutritional biology (including biosynthesis and ingredients of garlic and ginseng. aspects of different species. biopharmoceutics), chemistry From American Chemical Society Softcover, 422 pp. $34.95 . #8130 (including structure, detection and Symposium. Softcover, isolation), and clinical studies. 223 pp. $16.95. #8129 Hardcover, 426 pp. $129.95 #8142 MEDICINAL PLANTS OPIUM POPPY: BOTANY, TEA: CULTIVATION TO OF NORTH AFRICA OpiDJD CHEMISTRY AND CONSUMPTION by Loutfy Boulos. 1983. Authoritative, Poppy PHARMACOLOGY TEA Ed. -

Coding Competencies for Ophthalmic Techs – 2020 Coding Update
3/5/2020 Coding Competencies for Ophthalmic Techs – 2020 Coding Update OAO Ophthalmic Medical Technology Friday, March 13, 2020 Joy Woodke, COE, OCS, OCSR 1 Financial Disclosure Joy Woodke, COE, OCS o This presenter does not have a financial interest or relationship to disclose relative to this activity. o Academy Coding & Practice Management Executive 2 Topics 2020 Coding Updates Coding Competencies Diagnostic testing services Modifiers Tech Takeaways Understanding insurance policies Ongoing coding education Resources 3 1 3/5/2020 2020 Coding Updates Extended Ophthalmoscopy & Cataract Surgery 4 Extended Ophthalmoscopy (EO) • CPT eliminated initial and subsequent codes for EO • New codes for drawing of • Peripheral retina, with scleral depression: 5% in work value over deleted initial EO • Optic nerve or macula: 32% compared to deleted initial EO 5 Extended Ophthalmoscopy (EO) • 92225 Ophthalmoscopy, extended, with retinal drawing (eg, for retinal detachment, melanoma), with interpretation and report; initial • 92226 subsequent 6 2 3/5/2020 Extended Ophthalmoscopy (EO) 92201 Ophthalmoscopy, extended; with retinal drawing and scleral depression of peripheral retinal disease (eg, for retinal tear, retinal detachment, retinal tumor) with interpretation and report, unilateral or bilateral 7 Ophthalmoscopy 92201 8 8 Extended Ophthalmoscopy (EO) 92202 with drawing of optic nerve or macula (eg, for glaucoma, macular pathology, tumor) with interpretation and report, unilateral or bilateral 9 3 3/5/2020 Ophthalmoscopy 92202 10 Extended Ophthalmoscopy (EO) • Payment was unilateral. 2020 is bilateral. 2019 2020 92225 $29.87 per eye 92201 $27.21 Only bill for the eye that has 92202 $17.21 pathology. 92226 $27.63 per eye Only bill for the eye that has pathology 11 Extended Ophthalmoscopy (EO) • Payment is the same whether one or both eyes are examined and pathology is drawn and labeled. -

(YAG) Laser Capsulotomy Reference Number: CP.VP.65 Coding Implications Last Review Date: 12/2020 Revision Log
Clinical Policy: Yttrium Aluminium Garnet (YAG) Laser Capsulotomy Reference Number: CP.VP.65 Coding Implications Last Review Date: 12/2020 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description This policy describes the medical necessity requirements for yttrium aluminium garnet (YAG) laser capsulotomy. Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® (Centene) that YAG laser capsulotomy is medically necessary for the following indications: A. Posterior capsular opacification following cataract surgery resulting in best corrected visual acuity of 20/30 or worse associated with symptoms of blurred vision, visual distortion or glare affecting activities of daily living; B. Contraction of the posterior capsule with resulting displacement of the intraocular lens; C. Posterior capsular opacification resulting in best corrected visual acuity of 20/25 or worse, reducing the ability to evaluate and treat retinal detachment. Background YAG capsulotomy is the incision of an opaque posterior lens capsule in an aphakic or pseudophakic eye. This incision allows the capsule to retract and no longer serve as an obstruction to the passage of light through the media to the retina. The incision is performed with YAG laser. The eye examination must confirm the diagnosis of posterior capsular opacification and excludes other ocular causes of functional impairment by one of the following methods: The eye examination should demonstrate decreased light transmission (visual acuity worse than 20/30 or 20/25 if the procedure is performed to assist in the diagnosis and treatment of retinal detachment). Manifest refraction must be recorded with decrease in best-corrected visual acuity. -

Albrecht Von Graefe – Ein Portrait Berliner Armenaugenarzt Und Begründer Der Modernen Augenheilkunde Von Wolfgang Hanuschik
Aktuell Albrecht von Graefe – ein Portrait Berliner Armenaugenarzt und Begründer der modernen Augenheilkunde von Wolfgang Hanuschik Albrecht von Graefe wurde am 22. Mai Die Villa Finkenherd war ein gesellschaft- Bereits mit 15 Jahren besuchte A. von 1828 im sogenannten „Finkenherd“, licher Treffpunkt der Stadt. Künstler wie Graefe die Berliner Universität, an der er dem Sommersitz der Familie von Graefe A. von Camisso, die Portraitmalerin Ca- Mathematik, Naturwissenschaften, Philo- im Berliner Tiergarten und heutigen Han- roline Bardua und der Bildhauer Christian sophie und schließlich vor allem Medizin saviertel, geboren und starb am 20. Juli D. Rauch trafen sich mit Freunden von A. studierte. Dabei wurde er von Koryphäen 1870 in Berlin an Tuberkulose. Sein Vater von Graefe und seinen Schwestern Wan- wie Johannes Müller (Physiologie), Jo- war Karl Friedrich Ferdinand von Graefe, da und Ottilie. Von Graefe gründete dort hannes Dieffenbach (Innere Medizin) und der angesehene erste Direktor der chirur- die „Kamelia“, eine Art nicht schlagen- Rudolf Virchow (Pathologie) unterrichtet. gischen Klinik der Charité, seine Mutter de Studentenvereinigung. Drei Freunde Nach seinem Staatsexamen mit 19 Jah- war Auguste von Alten. A. von Graefe von Graefes studierten ebenfalls Medi- ren fuhr er zur Vertiefung seiner Kennt- besuchte das französische Gymnasium zin und wurden später Assistenzärzte in nisse nach Prag, Paris, Wien und London in Berlin, wo er eine besondere Begabung seiner Augenklinik: Adolf Waldau, Eduard – auch um sich darüber klar zu werden, für Mathematik, Physik und Philosophie Michaelis und Julius Ahrend. Mit ihnen welches Fach der Medizin er beruflich zeigte und fließend französisch sprechen verband ihn eine lebenslange Freund- ausüben wollte. In Prag war es Ferdinand lernte.