The Effect of Diffusion on Asymmetric Spin Echo Based Quantitative BOLD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RESENTS the DIN6 SOLEMMZEI) V姣fcfb)Te& to Hate Nts
\ PRICE TWO pieyea are COONCHJIAN FOULES REP- SBOWnZ-FARBER WED- •&•'*'-> • •-'- • JslMR RESENTS THE DIN6 SOLEMMZEI) Board of water Cemsiiuioa«r* j ceremony m^tersooa At -sa5) HUSfrtii aiemoem jiuei!tbi«cS ye«wrtaj at Vdcck o'clock following ta« m«*stlai of thm 4n«3Stcr of Ftrv ittai Commco Council toe crsaslaatloa pai" C&l«f asd Urs. Thomas nxitaxVJ. of • tatff po«««, Ul« xn««tlH3 bein< call«d to or- lt>3 Uaioa screes. b«cxia« th* bjrfd* of EJiaossft by Cl«rir Albert F. KlrMola. Com- j P^lilp J BorUn. ion of Mr. and Str* y Boylia. of 123 &oti fitted ^7". Harrtmas. over-osta their ... Tse- -bertsa Ca&ftw*: Blaror Harry Simmon* :• Ured in utin vith silver lace asd Councilman Trass I* Foulks as ' %ad p«arl trlnxmiar*. She wore m, escort to conduct Mr. Laagstroth to \ tore hat of wblta aatla asd silver tact 0 the chair. The latter feelingly ex-! end carri«d aa arm bouquet of wait* 0 hi* appreciation of the honor 'rose* and UUes of the reiley. The 5 b«atow«d upon aim. ; aaij ornament worn by the bridet was -"' "'•'>f^i&Ei. ••"•-•• ••. Next in order case tis« readlag' a> diamond brooca. the tXtX at the 0 COUUOH COUKCIL AND CTTV OPPftf^tS^llrtn <%•' - y v of a com rannication fsom> City* Clerk.' brtdacroom. The bridesmaid ' Mayo? to right—Steeet Commissioner George Getsel* City Attorney 51. V. TfafchftM^'^Mrftiiia^ Joka B. Thompson. Coosdlmas Chartvs H. Lambert, asnoasdag. Utathandscmaiy attired ta whits- - a ; 1 y?>y*y flnfffflwn, Cm^Mi^^ y*y^^% yA.. -

Towards a Neighborhood Simplification of Tile Systems: From
Nat Comput (2011) 10:103–117 DOI 10.1007/s11047-010-9193-1 Towards a neighborhood simplification of tile systems: From Moore to quasi-linear dependencies Eugen Czeizler • Lila Kari Published online: 28 April 2010 Ó Springer Science+Business Media B.V. 2010 Abstract Self-assembly is the process by which objects aggregate independently and form complex structures. One of the theoretical frameworks in which the process of self- assembly can be embedded and formally studied is that of tile systems. A Wang tile is a square unit, with glues on its edges, attaching to other tiles which have matching glues, and forming larger and larger structures. In this paper we concentrate over two basic, but essential, self-assembling structures done by Wang tiles. The first one, called ribbon, is a non-self-crossing wire-like structure, in which successive tiles are adjacent along an edge, and where tiles are glued to their predecessor and successor by use of matching glues. The second one, called zipper, is a similar contiguous structure, only that here, all touching tiles must have matching glues on their abutting edges, independently of their position in the structure. In case of Wang tiles, it has been shown that these two structures are equivalent. Here we generalize this result for the case when the tiles have eight glues, four on their edges and four on their corners. Thus we show that an eight neighborhood dependency, namely the Moore neighborhood, can be simulated by a quasi-linear dependency. Keywords Wang tiles Á Self-assembly Á Neighborhoods 1 Introduction Nano-technology is a new emergent field of research and development of the last couple of decades. -

5892 Cisco Category: Standards Track August 2010 ISSN: 2070-1721
Internet Engineering Task Force (IETF) P. Faltstrom, Ed. Request for Comments: 5892 Cisco Category: Standards Track August 2010 ISSN: 2070-1721 The Unicode Code Points and Internationalized Domain Names for Applications (IDNA) Abstract This document specifies rules for deciding whether a code point, considered in isolation or in context, is a candidate for inclusion in an Internationalized Domain Name (IDN). It is part of the specification of Internationalizing Domain Names in Applications 2008 (IDNA2008). Status of This Memo This is an Internet Standards Track document. This document is a product of the Internet Engineering Task Force (IETF). It represents the consensus of the IETF community. It has received public review and has been approved for publication by the Internet Engineering Steering Group (IESG). Further information on Internet Standards is available in Section 2 of RFC 5741. Information about the current status of this document, any errata, and how to provide feedback on it may be obtained at http://www.rfc-editor.org/info/rfc5892. Copyright Notice Copyright (c) 2010 IETF Trust and the persons identified as the document authors. All rights reserved. This document is subject to BCP 78 and the IETF Trust's Legal Provisions Relating to IETF Documents (http://trustee.ietf.org/license-info) in effect on the date of publication of this document. Please review these documents carefully, as they describe your rights and restrictions with respect to this document. Code Components extracted from this document must include Simplified BSD License text as described in Section 4.e of the Trust Legal Provisions and are provided without warranty as described in the Simplified BSD License. -

Zhangzhung Dictionary 35
**KA** KA YA Stein 242. (lus) body. LZ 3. KA YA BAG (bkrag mdangs rgyas) *KA See ti ka, ti ka rmad du, ti ka wide and full brightness, hi, ram lo ka ta. ZZH. lustre. ZZH. Zhu. Spelled ka ya KA (yul) country, realm. Sgra 135. ba in ZB. This meaning not found in KA YA A SHO TRI TRI SUM (lus Zhu. ngag yid gsum) body, speech KA KU (’gyur med) unchanged. and mind, these three. ZZH. Sgra 124. Could not find this in Zhu. There is some Sanskri- Mdzod. See the following. tization at work here. KA KYU [1] (’gyur med) unchan- KA YAB (bkrag mdangs) brilliance, ged, universal. ZZH. Zhu, once splendor. ZB. Of course, this only. ZB. [2] (mi ’gyur) im- can be read as: ka ya ba. mutable, unchanging. Mdzod. KA RI GYIN In Mdzod, ch. 7, it LZ 3. seems to corresp. to Tib. bstan KA TA (shes rab) insight. Sgra 124. pa, ‘teaching.’ This is likely to be a mistake. KA RU Stein 243. Tib. shes rab is always for ZZ ti *KA LA See su ri ka la [-yi]. ZZH. shan or tri shen in Mdzod. ZB gives also alternative spelling KA LA (ma g.yos) unbudged, im- ka te. mobile. ZB. LZ 3. KA TI (kun ’dud) ‘all bow,’ KA LA SHA (bdud rtsi) nectar. LZ apparently one of the seven 3. mountain chains in the cosmo- KA LAN TA KA (byi’ u mchil pa) logy. Mdzod, ch. 5. (kun ’dud sparrow the little bird. LZ 3. pa) to whom all bow. -

Kyrillische Schrift Für Den Computer
Hanna-Chris Gast Kyrillische Schrift für den Computer Benennung der Buchstaben, Vergleich der Transkriptionen in Bibliotheken und Standesämtern, Auflistung der Unicodes sowie Tastaturbelegung für Windows XP Inhalt Seite Vorwort ................................................................................................................................................ 2 1 Kyrillische Schriftzeichen mit Benennung................................................................................... 3 1.1 Die Buchstaben im Russischen mit Schreibschrift und Aussprache.................................. 3 1.2 Kyrillische Schriftzeichen anderer slawischer Sprachen.................................................... 9 1.3 Veraltete kyrillische Schriftzeichen .................................................................................... 10 1.4 Die gebräuchlichen Sonderzeichen ..................................................................................... 11 2 Transliterationen und Transkriptionen (Umschriften) .......................................................... 13 2.1 Begriffe zum Thema Transkription/Transliteration/Umschrift ...................................... 13 2.2 Normen und Vorschriften für Bibliotheken und Standesämter....................................... 15 2.3 Tabellarische Übersicht der Umschriften aus dem Russischen ....................................... 21 2.4 Transliterationen veralteter kyrillischer Buchstaben ....................................................... 25 2.5 Transliterationen bei anderen slawischen -

Original Sources Used for Teaching the Lion’S Dance Guadalajara Retreat, July 2017
ORIGINAL SOURCES USED FOR TEACHING THE LION’S DANCE GUADALAJARA RETREAT, JULY 2017 ♦This diamond mark indicates the start of a source work section; the dollar sign ($) indicates a concept or section beginning; curly braces with a percentage sign {%} indicate a mistake in the carving or input; notes are informal notes made by Geshe Michael to assist him in the teaching ♦Source text: The Jewel of Realizations (Abhisamayalankara) by Lord Maitreya, recorded by Arya Asanga (350ad) ,DE NAS SENG GE RNAM BSGYINGS PA'I, ,TING NGE 'DZIN LA SNYOMS ZHUGS NAS, ,RTEN CING 'BREL 'BYUNG LUGS MTHUN DANG, ,LUGS MI MTHUN LA RTOG PAR BYED, ,CES PA'I GZHUNG 'DI BYUNG, {SW: relate this to your experience of going up & coming down, a physical sensation; this was the Lion’s Dance} {this is all a reference to mngon rtogs rgyan: /Users/michaelroach/Documents/C DRIVE FILES/A/TENGYUR before Ven Phil/ 03_SHES_PHYIN/080_KA/TD3786E.ACT ,SBYIN PA LA SOGS RE RER NI, ,DE DAG PHAN TSUN BSDUS PA GANG, ,SKAD CIG GCIG PA'I BZOD PA YIS, ,BSDUS PA DE 'DIR MTHONG BA'I LAM, ,DE NAS SENG GE RNAM BSGYINGS PA'I, , TING NGE 'DZIN LA SNYOMS ZHUGS NAS, ,RTEN CING 'BREL 'BYUNG LUGS MTHUN DANG, ,LUGS MI MTHUN LA RTOG {sw: examine} PAR BYED, ,'GOG DANG BCAS PA'I SNYOMS 'JUG DGUR, ,RNAM PA GNYIS SU SONG 'ONGS NAS, ,'DOD PAR GTOGS PA'I RNAM PAR SHES, ,MNYAM GZHAG MIN PA'I MTSAMS BZUNG STE, ,THOD RGAL DU NI SNYOMS 'JUG PA,} 1 $Sanskrit for Lion’s Dance: \SENG GE RNAM PAR BSGYINGS ('GYINGS) PA ZHES BYA BA'I TING NGE 'DZIN\ |sim*havijr%mbhito na#ma sama#dhih%| {ma.vyu.533} {/ jr%mbh}, "gape". -
San Antonio Express 1869 06
rotul nbmll TO5ATB to tlie eoapony ot April, to wt tlw filARKIIT tatnetooMtiMiAp^l ® k » f a i l s t t f t m . •oven bnadred uiwl fifty loud itixlQr «ercir"Vi I Md A*- two Vtlirec ( k Alton W« an CteILKY aUata tm OfU^Jm f. IjurilMI HM IrHOOt fOa tea fri ^o«t^ I Judgwieii orer entlii Nothing but Ik* alaaOara shrill Waara T o x a a k a ^ har Arum reeeiviug her; whteh Tlwn|nln iMItL. KTOWK, "w b d m k b d a t JU N K «. 1*6». ueoriy oho JaMtcaat They iiropoop t<» ptedge tl share of thaao IndMattioua awtndm w v& rit r o * CONOKBM. rOUBTH DiaTHItT. able citiaena. I phMce tw* paMwafiKof motel were in- I hw orlveo, ,yillOM A*lI. HTRIBIdNO, WkttNtt^ A.miMMKC. muswraf*oH tualmuiac tiAf i I h r i 'h ^ aaa|»hit bV BKXUt ■an of the North, are working■kina thawthSr al tha Ptem th» till. ■■ieaiiiM eHt' r-----*— ' lb tlw ftwih, tn fitipinia ^ ■at haperitiaMa. Wa ara tlieoi tho oImivo mmo- auw twn wihl tha^’ pTnSwRI * rv jtcA ttr BoTthi mnt' «P «w i day; Mi Mondu* Uoged dn^inm^r «i»ditip!i«d jgiga Loc uuwilliag to. work UwitMl * r J 3 w the aamplriiai agitha «w L ..t » 4Mr Itar^doea Jiai aUr PpMMh, Waan t'.lan uAm I, oad pet ww legri dtp, to poah the work wllh aM pao- af>'. gd r granta an lhaarim oonpottedluoliUo.lhot w ( alM* diapatch. Thay did ant atala Pk «M M « A ro. -
Chilula Texts, 1914
3- (CONTINUED) ,red in exchange for the I libraries. Complete lists I ;t. For sample copies, lis A- ;he University Press, Berl UNIVERSITY OF CALIFORNIA PUBLICATIONS Be addressed to The Excl A. IN AMERICAN ARCHAEOLOGY AND y, Mt. Hamilton, Cal.) ETHNOLOGY [I, and X completed. Vol Vol. 10, No. 7, pp. 289-379 November 25, 1914 Volumes I (pp. 418), II ogress). Merrill, Herbert C. Nut 0) completed. Volume II ice per volume $2.50. ring Departments. This s Lfics, Mining, and Civil I CHILULA TEXTS *ew C. Lawson and Johb 1 (pp. 428), II (pp. 450), ;s), completed. Volume V L progress. BY volume, $2.50. Volume I PLINY EARLE GODDARD ), completed. Volume II 00. Volume I (pp. 217) c pp. 197) completed). Vol ress). per volume $3.50. Volum and V (pp. 440) comple olume II, this series contL Biological Association of rto). to the American Forms, 1-18; 154 text-figures. ............................................ 1; plates 85. December, Ll record of University I Price, $1.00 per year. C F CALIFORNIA.-Edited the President's Report, UNIVERSITY OF CALIFORNIA PRESS he above publications to I BERKELEY ad Ethnology, Classical P: Philology, Otto Harrassow. logy, Zoology and also Am in. UNIVERSITY OF CALIFORNIA PUBLICATIONS IN AMERICAN ARCHAEOLOGY AND ETHNOLOGY Vol. 10, No. 7, pp. 289-379 November 25, 1914 CHILULA TEXTS BY PLINY EARLE GODDARD CONTENTS PAGE Introduction ............. ................. ..... .............. ... 2.1........291 Sound Values of Characters Used . 291 TEXTS PART I. From Tom Hill and Dan Hill. I. The War with the Lassik Indians ......... ... ------- 293 II. Panther and Grizzly Bear ............... .. 295 III. -

Water Ice Cloud Feedbacks Over the North Polar Residual Cap at Moderate Obliquity
WATER ICE CLOUD FEEDBACKS OVER THE NORTH POLAR RESIDUAL CAP AT MODERATE OBLIQUITY. M. A. Kahre1 ([email protected]) and R. M. Haberle1 ([email protected]), 1NASA Ames Research Center, MS 245-3, Moffett Field, CA, 94035. Introduction: Several global climate modeling Ap Te (K) Tse (K) Te-Tse (K) Tg (K) studies have now shown that water ice clouds can warm Active 0.34 202 226 24 219 the surface 10s of K at moderate obliquities [1,2,3]. Sig- Inert 0.26 208 216 8 204 nificant greenhouse warming occurs because the pre- A-1 .08 -6 10 16 15 dicted clouds are optically thick, the cloud particles are Table 1: Planetary Albedo (A ), effective temperature at the top of the large enough to efficiently interact with infrared radia- p atmosphere (Te), effective surface temperature, greenhouse power (Te- tion, and the clouds either form at or are transported to Tse), and surface temperature (Tg) for the case with radiatively active high altitudes where the atmosphere is cold. Radiative- clouds and the case with radiatively inert clouds. dynamic feedbacks play a critical role in producing the conditions needed for a strong cloud greenhouse. Two During NH summer, the radiatively active cloud feedbacks have been identified: one involves atmos- case produces clouds that grow thick, warm the surface, pheric warming by clouds aloft at lower latitudes. and enhance sublimation relative to the simulation with These clouds are generally associated with the global radiatively inert clouds (Figure 1). This occurs because Hadley circulation. The second feedback involves clouds extend to high altitudes over the NPRC (Figure clouds that form over the North Polar Residual Cap 2) and radiate to space at a cold temperature, forcing the (NPRC) during summer. -

1 Symbols (2286)
1 Symbols (2286) USV Symbol Macro(s) Description 0009 \textHT <control> 000A \textLF <control> 000D \textCR <control> 0022 ” \textquotedbl QUOTATION MARK 0023 # \texthash NUMBER SIGN \textnumbersign 0024 $ \textdollar DOLLAR SIGN 0025 % \textpercent PERCENT SIGN 0026 & \textampersand AMPERSAND 0027 ’ \textquotesingle APOSTROPHE 0028 ( \textparenleft LEFT PARENTHESIS 0029 ) \textparenright RIGHT PARENTHESIS 002A * \textasteriskcentered ASTERISK 002B + \textMVPlus PLUS SIGN 002C , \textMVComma COMMA 002D - \textMVMinus HYPHEN-MINUS 002E . \textMVPeriod FULL STOP 002F / \textMVDivision SOLIDUS 0030 0 \textMVZero DIGIT ZERO 0031 1 \textMVOne DIGIT ONE 0032 2 \textMVTwo DIGIT TWO 0033 3 \textMVThree DIGIT THREE 0034 4 \textMVFour DIGIT FOUR 0035 5 \textMVFive DIGIT FIVE 0036 6 \textMVSix DIGIT SIX 0037 7 \textMVSeven DIGIT SEVEN 0038 8 \textMVEight DIGIT EIGHT 0039 9 \textMVNine DIGIT NINE 003C < \textless LESS-THAN SIGN 003D = \textequals EQUALS SIGN 003E > \textgreater GREATER-THAN SIGN 0040 @ \textMVAt COMMERCIAL AT 005C \ \textbackslash REVERSE SOLIDUS 005E ^ \textasciicircum CIRCUMFLEX ACCENT 005F _ \textunderscore LOW LINE 0060 ‘ \textasciigrave GRAVE ACCENT 0067 g \textg LATIN SMALL LETTER G 007B { \textbraceleft LEFT CURLY BRACKET 007C | \textbar VERTICAL LINE 007D } \textbraceright RIGHT CURLY BRACKET 007E ~ \textasciitilde TILDE 00A0 \nobreakspace NO-BREAK SPACE 00A1 ¡ \textexclamdown INVERTED EXCLAMATION MARK 00A2 ¢ \textcent CENT SIGN 00A3 £ \textsterling POUND SIGN 00A4 ¤ \textcurrency CURRENCY SIGN 00A5 ¥ \textyen YEN SIGN 00A6 -

Filled Full of Shot in a Blaze of Glory
DILLON, BEAVERHEAD COUNTY. MONTANA.4W EDNESDAY, MAY ao. 18»*. VOLUME III. N U M B E R 3 8 A T UAH|>’S CAPITAL. COXLVITUS TO MLIT. 1 PLOT NIPPLO IN THL BI LL FILLED FULL OF SHOT DESPERATE, MINERS <¿rttu.l Arm., ItHke+n ■ ,¡U, ,^,'1. K.îr IN A BLAZE OF GLORY 1 1 ;uk fn to tiijt li« r in lies Mollies to furm* l i . H i A iif lltì.MIKt, iltAIit SKAGIT RIVER FLOOD nhiU' it Nitiioiutl tirciUil/ittlon. f f.» tu.,* I ,i * t u,. \t yeaicrday'» ! D u s M u i n k s . M a y ' 2b — A acbcoje U on B'Xhe, Uiho, Maj Í5 \\ u.h HSH.HHK. P* ST. — A inai »esalon U è Ai rand Army t-Dcampmebl tool Jo gxrpetuatc the ccmmouwcal « ino li, for duworigat fietidisbiie,,. v*a, Terrible Slaughter of Human Be eiecled the follov,¿ng 0 , in hL.i 10 Laid ii».' Como: Michael Gilmore Killed by Andrew utovemtht. A uiueUnp: uf 0 .e leaders m w \ .i-nnaUetl Iti tht avi» iW t,f oCme Ncurly tv vi y Town ni the County ings at Cnpple Cieek. m a n d e r , T. J, Cr«om e of S u i . Scnint ; tho S,m.I -••¡r,’ Ho. Et itti, His Pattiu'r. will bo hold iu Ue* SOOO to UiMB ai lUi, i tikiii vi R e Country waa Is Nnvv U aj..e' W ater. sice t.'omaiu,k-t, Ivtei M.iu.tiwi l’n,j ; a LjtiOhal Assoriailoo. -
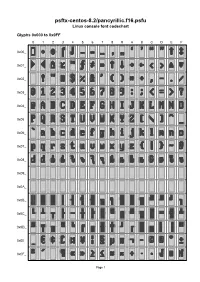
Psftx-Centos-8.2/Pancyrillic.F16.Psfu Linux Console Font Codechart
psftx-centos-8.2/pancyrillic.f16.psfu Linux console font codechart Glyphs 0x000 to 0x0FF 0 1 2 3 4 5 6 7 8 9 A B C D E F 0x00_ 0x01_ 0x02_ 0x03_ 0x04_ 0x05_ 0x06_ 0x07_ 0x08_ 0x09_ 0x0A_ 0x0B_ 0x0C_ 0x0D_ 0x0E_ 0x0F_ Page 1 Glyphs 0x100 to 0x1FF 0 1 2 3 4 5 6 7 8 9 A B C D E F 0x10_ 0x11_ 0x12_ 0x13_ 0x14_ 0x15_ 0x16_ 0x17_ 0x18_ 0x19_ 0x1A_ 0x1B_ 0x1C_ 0x1D_ 0x1E_ 0x1F_ Page 2 Font information 0x018 U+2191 UPWARDS ARROW Filename: psftx-centos-8.2/pancyrillic.f16.psfu 0x019 U+2193 DOWNWARDS ARROW PSF version: 1 0x01A U+2192 RIGHTWARDS ARROW Glyph size: 8 × 16 pixels Glyph count: 512 0x01B U+2190 LEFTWARDS ARROW Unicode font: Yes (mapping table present) 0x01C U+2039 SINGLE LEFT-POINTING ANGLE QUOTATION MARK Unicode mappings 0x01D U+2040 CHARACTER TIE 0x000 U+FFFD REPLACEMENT CHARACTER 0x01E U+25B2 BLACK UP-POINTING 0x001 U+2022 BULLET TRIANGLE 0x01F U+25BC BLACK DOWN-POINTING 0x002 U+25C6 BLACK DIAMOND, TRIANGLE U+2666 BLACK DIAMOND SUIT 0x020 U+0020 SPACE 0x003 U+2320 TOP HALF INTEGRAL 0x021 U+0021 EXCLAMATION MARK 0x004 U+2321 BOTTOM HALF INTEGRAL 0x022 U+0022 QUOTATION MARK 0x005 U+2013 EN DASH 0x023 U+0023 NUMBER SIGN 0x006 U+2014 EM DASH 0x024 U+0024 DOLLAR SIGN 0x007 U+2026 HORIZONTAL ELLIPSIS 0x025 U+0025 PERCENT SIGN 0x008 U+201A SINGLE LOW-9 QUOTATION MARK 0x026 U+0026 AMPERSAND 0x009 U+201E DOUBLE LOW-9 0x027 U+0027 APOSTROPHE QUOTATION MARK 0x00A U+2018 LEFT SINGLE QUOTATION 0x028 U+0028 LEFT PARENTHESIS MARK 0x029 U+0029 RIGHT PARENTHESIS 0x00B U+2019 RIGHT SINGLE QUOTATION MARK 0x02A U+002A ASTERISK 0x00C U+201C LEFT DOUBLE