Glutathione S-Transferases in Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Bioinformatics Identification of Potential Genes and Pathways in Preeclampsia Based on Functional Gene Set Enrichment Analyses
EXPERIMENTAL AND THERAPEUTIC MEDICINE 18: 1837-1844, 2019 Bioinformatics identification of potential genes and pathways in preeclampsia based on functional gene set enrichment analyses XUE LI and YANNING FANG Department of Obstetrics, The First People's Hospital of Jining, Jining, Shandong 272000, P.R. China Received October 24, 2018; Accepted May 2, 2019 DOI: 10.3892/etm.2019.7749 Abstract. Preeclampsia is a complication of pregnancy the sample into four distinct groups based on different incu- characterized by new-onset hypertension and proteinuria of bation time. The top 3 candidates were Toll-like receptor 2 gestation, with serious consequences for mother and infant. (TLR2), glutathione S-transferase omega 1 (GSTO1) and Although a vast amount of research has been performed on mitogen-activated protein kinase 13 (MAPK13). TLR2 and the pathogenesis of preeclampsia, the underlying mechanisms associated pathways are known to be closely associated with of this multisystemic disease have remained to be fully eluci- preeclampsia, indirectly demonstrating the applicability of dated. Data were retrieved from Gene Expression Omnibus the analytic process applied. However, the role of GSTO1 and database GSE40182 dataset. After data preprocessing, differ- MAPK13 in preeclampsia has remained poorly investigated, entially expressed genes of placental cells cultured in vitro and elucidation thereof may be a worthwhile endeavor. The from preeclampsia and normal pregnancy were determined present study may provide a basis for exploring potential novel and subjected to Kyoto Encyclopedia of Genes and Genomes genes and pathways as therapeutic targets for preeclampsia. (KEGG) enrichment analysis to identify the associated path- ways. Furthermore, functional principal component analysis Introduction (FPCA) was used to calculate the corresponding F-value of each gene. -

Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’S Biological Network Based on Systematic Pharmacology
ORIGINAL RESEARCH published: 25 June 2021 doi: 10.3389/fphar.2021.601846 Exploring the Regulatory Mechanism of Hedysarum Multijugum Maxim.-Chuanxiong Rhizoma Compound on HIF-VEGF Pathway and Cerebral Ischemia-Reperfusion Injury’s Biological Network Based on Systematic Pharmacology Kailin Yang 1†, Liuting Zeng 1†, Anqi Ge 2†, Yi Chen 1†, Shanshan Wang 1†, Xiaofei Zhu 1,3† and Jinwen Ge 1,4* Edited by: 1 Takashi Sato, Key Laboratory of Hunan Province for Integrated Traditional Chinese and Western Medicine on Prevention and Treatment of 2 Tokyo University of Pharmacy and Life Cardio-Cerebral Diseases, Hunan University of Chinese Medicine, Changsha, China, Galactophore Department, The First 3 Sciences, Japan Hospital of Hunan University of Chinese Medicine, Changsha, China, School of Graduate, Central South University, Changsha, China, 4Shaoyang University, Shaoyang, China Reviewed by: Hui Zhao, Capital Medical University, China Background: Clinical research found that Hedysarum Multijugum Maxim.-Chuanxiong Maria Luisa Del Moral, fi University of Jaén, Spain Rhizoma Compound (HCC) has de nite curative effect on cerebral ischemic diseases, *Correspondence: such as ischemic stroke and cerebral ischemia-reperfusion injury (CIR). However, its Jinwen Ge mechanism for treating cerebral ischemia is still not fully explained. [email protected] †These authors share first authorship Methods: The traditional Chinese medicine related database were utilized to obtain the components of HCC. The Pharmmapper were used to predict HCC’s potential targets. Specialty section: The CIR genes were obtained from Genecards and OMIM and the protein-protein This article was submitted to interaction (PPI) data of HCC’s targets and IS genes were obtained from String Ethnopharmacology, a section of the journal database. -

GSTM2 Monoclonal Antibody (M03), Clone 1E10
GSTM2 monoclonal antibody (M03), clone 1E10 Catalog # : H00002946-M03 規格 : [ 100 ug ] List All Specification Application Image Product Mouse monoclonal antibody raised against a partial recombinant Western Blot (Cell lysate) Description: GSTM2. Immunogen: GSTM2 (NP_000839, 90 a.a. ~ 189 a.a) partial recombinant protein with GST tag. MW of the GST tag alone is 26 KDa. Sequence: SEKEQIREDILENQFMDSRMQLAKLCYDPDFEKLKPEYLQALPEMLKLYS QFLGKQPWFLGDKITFVDFIAYDVLERNQVFEPSCLDAFPNLKDFISRFE enlarge Western Blot (Recombinant Host: Mouse protein) Reactivity: Human, Mouse Immunohistochemistry (Formalin/PFA-fixed paraffin- Isotype: IgG1 Kappa embedded sections) Quality Control Antibody Reactive Against Recombinant Protein. Testing: enlarge Immunofluorescence enlarge Western Blot detection against Immunogen (36.74 KDa) . Sandwich ELISA (Recombinant Storage Buffer: In 1x PBS, pH 7.4 protein) Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. Instruction: MSDS: Download enlarge Datasheet: Download ELISA Publication Reference 1. A DNA hypermethylation profile reveals new potential biomarkers for prostate cancer diagnosis and prognosis. Ashour N, Angulo JC, Andres G, Alelu R, Gonzalez-Corpas A, Toledo MV, Rodriguez- Barbero JM, Lopez JI, Sanchez-Chapado M, Ropero SProstate. 2014 Sep;74(12):1171- 82. doi: 10.1002/pros.22833. Epub 2014 Jun 24. Applications Western Blot (Cell lysate) Page 1 of 3 2016/5/21 GSTM2 monoclonal antibody (M03), clone 1E10. Western Blot analysis of GSTM2 expression in NIH/3T3 ( Cat # L018V1 ). Protocol Download Western Blot (Recombinant protein) Protocol Download Immunohistochemistry (Formalin/PFA-fixed paraffin-embedded sections) enlarge this image Immunoperoxidase of monoclonal antibody to GSTM2 on formalin-fixed paraffin-embedded human breast cancer. [antibody concentration 3 ug/ml] Protocol Download Immunofluorescence enlarge this image Immunofluorescence of monoclonal antibody to GSTM2 on HeLa cell . -

Genomic Profiling of Short- and Long-Term Caloric Restriction Effects in the Liver of Aging Mice
Genomic profiling of short- and long-term caloric restriction effects in the liver of aging mice Shelley X. Cao, Joseph M. Dhahbi, Patricia L. Mote, and Stephen R. Spindler* Department of Biochemistry, University of California, Riverside, CA 92521 Edited by Bruce N. Ames, University of California, Berkeley, CA, and approved July 11, 2001 (received for review June 19, 2001) We present genome-wide microarray expression analysis of 11,000 aging and CR on gene expression. Control young (7-month-old; n ϭ genes in an aging potentially mitotic tissue, the liver. This organ has 3) and old (27-month-old; n ϭ 3) mice were fed 95 kcal of a a major impact on health and homeostasis during aging. The effects semipurified control diet (Harlan Teklad, Madison, WI; no. of life- and health-span-extending caloric restriction (CR) on gene TD94145) per week after weaning. Long-term CR (LT-CR) young expression among young and old mice and between long-term CR (7-month-old; n ϭ 3) and old (27-month-old; n ϭ 3) mice were fed (LT-CR) and short-term CR (ST-CR) were examined. This experimental 53 kcal of a semipurified CR diet (Harlan Teklad; no. TD94146) per design allowed us to accurately distinguish the effects of aging from week after weaning. Short-term CR (ST-CR) mice were 34-month- those of CR on gene expression. Aging was accompanied by changes old control mice that were switched to 80 kcal of CR diet for 2 in gene expression associated with increased inflammation, cellular weeks, followed by 53 kcal for 2 weeks (n ϭ 3). -
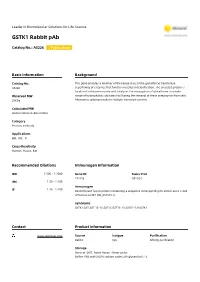
GSTK1 Rabbit Pab
Leader in Biomolecular Solutions for Life Science GSTK1 Rabbit pAb Catalog No.: A5226 1 Publications Basic Information Background Catalog No. This gene encodes a member of the kappa class of the glutathione transferase A5226 superfamily of enzymes that function in cellular detoxification. The encoded protein is localized to the peroxisome and catalyzes the conjugation of glutathione to a wide Observed MW range of hydrophobic substates facilitating the removal of these compounds from cells. 25KDa Alternative splicing results in multiple transcript variants. Calculated MW 20kDa/24kDa/25kDa/31kDa Category Primary antibody Applications WB, IHC, IF Cross-Reactivity Human, Mouse, Rat Recommended Dilutions Immunogen Information WB 1:500 - 1:2000 Gene ID Swiss Prot 373156 Q9Y2Q3 IHC 1:50 - 1:100 Immunogen 1:50 - 1:100 IF Recombinant fusion protein containing a sequence corresponding to amino acids 1-226 of human GSTK1 (NP_057001.1). Synonyms GSTK1;GST;GST 13-13;GST13;GST13-13;GSTK1-1;hGSTK1 Contact Product Information www.abclonal.com Source Isotype Purification Rabbit IgG Affinity purification Storage Store at -20℃. Avoid freeze / thaw cycles. Buffer: PBS with 0.02% sodium azide,50% glycerol,pH7.3. Validation Data Western blot analysis of extracts of various cell lines, using GSTK1 antibody (A5226) at 1:1000 dilution. Secondary antibody: HRP Goat Anti-Rabbit IgG (H+L) (AS014) at 1:10000 dilution. Lysates/proteins: 25ug per lane. Blocking buffer: 3% nonfat dry milk in TBST. Detection: ECL Basic Kit (RM00020). Exposure time: 60s. Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- Immunohistochemistry of paraffin- embedded human lung cancer using embedded human liver cancer using embedded human thyroid cancer using GSTK1 Rabbit pAb (A5226) at dilution of GSTK1 Rabbit pAb (A5226) at dilution of GSTK1 Rabbit pAb (A5226) at dilution of 1:25 (40x lens). -

Characterization of Visceral and Subcutaneous Adipose Tissue
J. Perinat. Med. 2016; 44(7): 813–835 Shali Mazaki-Tovi*, Adi L. Tarca, Edi Vaisbuch, Juan Pedro Kusanovic, Nandor Gabor Than, Tinnakorn Chaiworapongsa, Zhong Dong, Sonia S. Hassan and Roberto Romero* Characterization of visceral and subcutaneous adipose tissue transcriptome in pregnant women with and without spontaneous labor at term: implication of alternative splicing in the metabolic adaptations of adipose tissue to parturition DOI 10.1515/jpm-2015-0259 groups (unpaired analyses) and adipose tissue regions Received July 27, 2015. Accepted October 26, 2015. Previously (paired analyses). Selected genes were tested by quantita- published online March 19, 2016. tive reverse transcription-polymerase chain reaction. Abstract Results: Four hundred and eighty-two genes were differ- entially expressed between visceral and subcutaneous Objective: The aim of this study was to determine gene fat of pregnant women with spontaneous labor at term expression and splicing changes associated with par- (q-value < 0.1; fold change > 1.5). Biological processes turition and regions (visceral vs. subcutaneous) of the enriched in this comparison included tissue and vascu- adipose tissue of pregnant women. lature development as well as inflammatory and meta- Study design: The transcriptome of visceral and abdomi- bolic pathways. Differential splicing was found for 42 nal subcutaneous adipose tissue from pregnant women at genes [q-value < 0.1; differences in Finding Isoforms using term with (n = 15) and without (n = 25) spontaneous labor Robust Multichip Analysis scores > 2] between adipose was profiled with the Affymetrix GeneChip Human Exon tissue regions of women not in labor. Differential exon 1.0 ST array. Overall gene expression changes and the dif- usage associated with parturition was found for three ferential exon usage rate were compared between patient genes (LIMS1, HSPA5, and GSTK1) in subcutaneous tissues. -

Whole Egg Consumption Increases Gene Expression Within the Glutathione Pathway in the Liver of Zucker Diabetic Fatty Rats
Food Science and Human Nutrition Publications Food Science and Human Nutrition 11-3-2020 Whole egg consumption increases gene expression within the glutathione pathway in the liver of Zucker Diabetic Fatty rats Joe L. Webb Iowa State University Amanda E. Bries Iowa State University, [email protected] Brooke Vogel Iowa State University Claudia Carrillo Iowa State University, [email protected] Lily Harvison Iowa State University, [email protected] See next page for additional authors Follow this and additional works at: https://lib.dr.iastate.edu/fshn_hs_pubs Part of the Dietetics and Clinical Nutrition Commons, Endocrinology, Diabetes, and Metabolism Commons, Exercise Science Commons, Food Chemistry Commons, Human and Clinical Nutrition Commons, and the Molecular, Genetic, and Biochemical Nutrition Commons The complete bibliographic information for this item can be found at https://lib.dr.iastate.edu/ fshn_hs_pubs/38. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Food Science and Human Nutrition at Iowa State University Digital Repository. It has been accepted for inclusion in Food Science and Human Nutrition Publications by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Whole egg consumption increases gene expression within the glutathione pathway in the liver of Zucker Diabetic Fatty rats Abstract Nutrigenomic evidence supports the idea that Type 2 Diabetes Mellitus (T2DM) arises due to the interactions between the transcriptome, individual genetic profiles, lifestyle, and diet. Since eggs are a nutrient dense food containing bioactive ingredients that modify gene expression, our goal was to examine the role of whole egg consumption on the transcriptome during T2DM. -

32-2407: GSTM2 Recombinant Protein Description Product Info
ABGENEX Pvt. Ltd., E-5, Infocity, KIIT Post Office, Tel : +91-674-2720712, +91-9437550560 Email : [email protected] Bhubaneswar, Odisha - 751024, INDIA 32-2407: GSTM2 Recombinant Protein Alternative Name : Glutathione S-transferase Mu 2,GST class-mu 2,GSTM2-2,GSTM2,GST4,GSTM,GTHMUS,MGC117303. Description Source : Escherichia Coli. GSTM2 Human Recombinant fused with a 20 amino acid His tag at N-terminus produced in E.Coli is a single, non-glycosylated, polypeptide chain containing 238 amino acids (1-218 a.a.) and having a molecular mass of 27.9kDa. The GSTM2 is purified by proprietary chromatographic techniques. Glutathione S-transferase Mu 2 (GSTM2) belongs to the glutathione s-transferase (GST) family of proteins. GSTM2 is a glutathione S-transferase that belongs to the mu class. There are 8 families of GST proteins, specifically: alpha, kappa, mu, omega, pi, sigma, theta and zeta, each of which is composed of proteins that have various functions throughout the cell. The mu class of enzymes functions in the detoxification of electrophilic compounds, including carcinogens, therapeutic drugs, environmental toxins and products of oxidative stress, by conjugation with glutathione. The genes encoding the mu class of enzymes are structured in a gene cluster on chromosome 1p13.3 and are proven to be highly polymorphic. These genetic variants can change an individual''s susceptibility to carcinogens and toxins as well as have an effect on the toxicity and efficacy of several drugs. Product Info Amount : 20 µg Purification : Greater than 95.0% as determined by SDS-PAGE. The GSTM2 solution (0.5 mg/ml) contains 20mM Tris-HCl buffer (pH8.0), 10% glycerol,0.1M NaCl Content : and 1mM DTT. -

9 Glutathione S-Transferases
Enzyme Systems that Metabolise Drugs and Other Xenobiotics. Edited by Costas Ioannides Copyright # 2001 John Wiley & Sons Ltd ISBNs: 0-471-894-66-4 %Hardback); 0-470-84630-5 %Electronic) 9 Glutathione S-transferases Philip J. Sherratt and John D. Hayes University of Dundee, UK Introduction Glutathione S-transferase GST; EC 2.5.1.18) isoenzymes are ubiquitously distributed in nature, being found in organisms as diverse as microbes, insects, plants, ®sh, birds andmammals Hayes andPulford1995). The transferases possess various activities andparticipate in several differenttypes of reaction. Most of these enzymes can catalyse the conjugation of reduced glutathione GSH) with compounds that contain an electrophilic centre through the formation of a thioether bondbetween the sulphur atom of GSH and the substrate Chasseaud 1979; Mannervik 1985). In addition to conjugation reactions, a number of GST isoenzymes exhibit other GSH-dependent catalytic activities including the reduction of organic hydroperoxides Ketterer et al. 1990) andisomerisation of various unsaturatedcompoundsBenson et al. 1977; Jakoby andHabig 1980). These enzymes also have several non-catalytic functions that relate to the sequestering of carcinogens, intracellular transport of a wide spectrum of hydrophobic ligands, and modulation of signal transduction pathways Listowsky 1993; Adler et al. 1999; Cho et al. 2001). Glutathione S-transferases represent a complex grouping of proteins. Two entirely distinct superfamilies of enzyme have evolved that possess transferase activity Hayes andStrange 2000). The ®rst enzymes to be characterisedwere the cytosolic, or soluble, GSTs BoylandandChasseaud1969; Mannervik 1985). To dateat least 16 members of this superfamily have been identi®ed in humans Board et al. 1997, 2000; Hayes and Strange 2000). -

Human Induced Pluripotent Stem Cell–Derived Podocytes Mature Into Vascularized Glomeruli Upon Experimental Transplantation
BASIC RESEARCH www.jasn.org Human Induced Pluripotent Stem Cell–Derived Podocytes Mature into Vascularized Glomeruli upon Experimental Transplantation † Sazia Sharmin,* Atsuhiro Taguchi,* Yusuke Kaku,* Yasuhiro Yoshimura,* Tomoko Ohmori,* ‡ † ‡ Tetsushi Sakuma, Masashi Mukoyama, Takashi Yamamoto, Hidetake Kurihara,§ and | Ryuichi Nishinakamura* *Department of Kidney Development, Institute of Molecular Embryology and Genetics, and †Department of Nephrology, Faculty of Life Sciences, Kumamoto University, Kumamoto, Japan; ‡Department of Mathematical and Life Sciences, Graduate School of Science, Hiroshima University, Hiroshima, Japan; §Division of Anatomy, Juntendo University School of Medicine, Tokyo, Japan; and |Japan Science and Technology Agency, CREST, Kumamoto, Japan ABSTRACT Glomerular podocytes express proteins, such as nephrin, that constitute the slit diaphragm, thereby contributing to the filtration process in the kidney. Glomerular development has been analyzed mainly in mice, whereas analysis of human kidney development has been minimal because of limited access to embryonic kidneys. We previously reported the induction of three-dimensional primordial glomeruli from human induced pluripotent stem (iPS) cells. Here, using transcription activator–like effector nuclease-mediated homologous recombination, we generated human iPS cell lines that express green fluorescent protein (GFP) in the NPHS1 locus, which encodes nephrin, and we show that GFP expression facilitated accurate visualization of nephrin-positive podocyte formation in -

Resolution of Conflict Between Parental Genomes in a Hybrid Species
bioRxiv preprint doi: https://doi.org/10.1101/102970; this version posted January 25, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Title: Resolution of conflict between parental genomes in a hybrid species 2 3 4 5 6 7 8 9 10 11 Fabrice Eroukhmanoff1†, Richard I. Bailey1,2†, Tore O. Elgvin1, Jo S. Hermansen1, Anna R. 12 Runemark1, Cassandra N. Trier1, Glenn-Peter Sætre1 13 1Department of Biosciences, Centre for Evolutionary and Ecological Synthesis, University of 14 Oslo, Norway. 2Division of Animal Evolutionary Biology, Department of Zoology, Faculty of 15 Science, Charles University in Prague, Viničná 7, 128 44 Praha, Czech Republic. 16 17 Corresponding author: [email protected] 18 19 †These authors contributed equally to the manuscript 20 21 22 23 24 25 26 1 bioRxiv preprint doi: https://doi.org/10.1101/102970; this version posted January 25, 2017. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 27 Abstract: 28 The development of reproductive barriers against parent species is crucial during hybrid 29 speciation, and post-zygotic isolation can be important in this process. Genetic 30 incompatibilities that normally isolate the parent species can become sorted in hybrids to form 31 reproductive barriers towards either parent. However, the extent to which this sorting process 32 is systematically biased and therefore predictable in which loci are involved and which alleles 33 are favored is largely unknown.