Article/25/10/19-0700- App1.Xlsx)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sample Procurement Plan
Sample Procurement Plan Public Disclosure Authorized I. General 1. Bank’s approval Date of the procurement Plan [Original: October 2016]: Revision 1 of Updated Procurement Plan, January 2017] 2. Date of General Procurement Notice: 15 July 2017 3. Period covered by this procurement plan: The procurement period of project covered from year January 2017 to December 2018 II. Goods and Works and non-consulting services. 1. Prior Review Threshold: Procurement Decisions subject to Prior Review Public Disclosure Authorized by the Bank as stated in Appendix 1 to the Guidelines for Procurement: Procurement Method Prior Review Comments Threshold US$ 1. ICB and LIB (Goods) Above US$ 500,000 All 2. NCB (Goods) Above US$ 780,000 All 3. ICB (Works) Above US$ 10 million All 4. NCB (Works) Above US$ 476,000 First contract 5. Consultation of the suppliers Above US$ 20,000 First contract (Works) 6. (Non-Consultant Services) Above US$ 10,000 First contract 6. Individual consultants Above US$ 19,200 All Public Disclosure Authorized [Add other methods if necessary] 2. Prequalification. Bidders for _Not applicable_ shall be prequalified in accordance with the provisions of paragraphs 2.9 and 2.10 of the Guidelines. 3. Proposed Procedures for CDD Components (as per paragraph. 3.17 of the Guidelines: 4. Reference to (if any) Project Operational/Procurement Manual: Project Implementation Manual for World Bank Loan Project under preparation. Public Disclosure Authorized 5. Any Other Special Procurement Arrangements: 5 ICB works packages will be financed under Project preparation advance. 6. Summary of the Procurement Packages planned during the first 18 months PADAP August 22, 2017 after project effectiveness 1 2 3 4 5 6 7 Ref. -

1 COAG No. 72068718CA00001
COAG No. 72068718CA00001 1 TABLE OF CONTENT I- EXECUTIVE SUMMARY .................................................................................................................................................. 6 II- INTRODUCTION ....................................................................................................................................................... 10 III- MAIN ACHIEVEMENTS DURING QUARTER 1 ........................................................................................................... 10 III.1. IR 1: Enhanced coordination among the public, nonprofit, and commercial sectors for reliable supply and distribution of quality health products ........................................................................................................................... 10 III.2. IR2: Strengthened capacity of the GOM to sustainably provide quality health products to the Malagasy people 15 III.3. IR 3: Expanded engagement of the commercial health sector to serve new health product markets, according to health needs and consumer demand ........................................................................................................ 36 III.4. IR 4: Improved sustainability of social marketing to deliver affordable, accessible health products to the Malagasy people ............................................................................................................................................................. 48 III.5. IR5: Increased demand for and use of health products among the Malagasy people -

Socio-Economic, Land Use and Value Chain Perspectives on Vanilla Farming in the SAVA Region (North-Eastern Madagascar): the Dive
Department of Agricultural Economics and Rural Development Socio-economic, land use and value chain Georg-August Universität Göttingen perspectives on vanilla farming in the SAVA Region (north-eastern Madagascar): The Diversity Turn Baseline Study (DTBS) Discussion Paper 1806 Hendrik Hänke, Jan Barkmann, Lloyd Blum, Yvonne Franke, Dominic A. Martin, Janna Niens, Kristina Osen, Viviana Uruena, S. Annette Witherspoon, Annemarie Wurz Department of Agricultural Economics and Rural Development University of Goettingen D 37073 Göttingen ISSN 1865-2697 Diversity turn in land use science, the importance of social diversity for sustainable land use innovations using the example of vanilla farming in Madagascar. WP1: Project Management, Coordination, Theoretical Advancement Prof. Dr. Andrea D. Bührmann1), Dr. Yvonne Franke1), Prof. Dr. Rainer Marggraf2), Dr. Hendrik Hänke2) 1) Göttingen Diversity Research Institute, Faculty of Social Sciences, University of Goettingen 2) Research Unit Environmental-and Resource Economics, Department of Agricultural Economics and Rural Development, University of Goettingen WP2: PhD program "Diversity Turn in Sustainability Science" Prof. Dr. Andrea D. Bührmann, Dr. Yvonne Franke Göttingen Diversity Research Institute, Faculty of Social Sciences, University of Goettingen WP3: Social Diversity and Power Relations Prof. Dr. Andrea D. Bührmann1), Annette Witherspoon1), Raozivelo Ony Solomampionona2) 1) Göttingen Diversity Research Institute, Faculty of Social Sciences University of Goettingen 2) Department of Sociology, -

Endemic Chromoblastomycosis Caused Predominantly By
Endemic Chromoblastomycosis Caused Predominantly by Fonsecaea nubica, Madagascar1 Tahinamandranto Rasamoelina, Danièle Maubon, Malalaniaina Andrianarison, Irina Ranaivo, Fandresena Sendrasoa, Njary Rakotozandrindrainy, Fetra A. Rakotomalala, Sébastien Bailly, Benja Rakotonirina, Abel Andriantsimahavandy, Fahafahantsoa R. Rabenja, Mala Rakoto Andrianarivelo, Muriel Cornet, Lala S. Ramarozatovo Chromoblastomycosis is an implantation fungal infec- plant material from thorns or wood splinters or by soil tion. Twenty years ago, Madagascar was recognized as contamination of an existing wound (1,2). The causative the leading focus of this disease. We recruited patients agents are mainly Fonsecaea spp., Cladophialophora spp., in Madagascar who had chronic subcutaneous lesions and Rhinocladiella spp. However, rare cases caused by suggestive of dermatomycosis during March 2013– other genera, such as Phialophora spp. or Exophiala spp., June 2017. Chromoblastomycosis was diagnosed in 50 have been reported (1,3). As is the case for other implan- (33.8%) of 148 patients. The highest prevalence was in tation mycoses, chromoblastomycosis lesions are locat- northeastern (1.47 cases/100,000 persons) and southern ed mainly on the lower limbs, particularly on the dorsal (0.8 cases/100,000 persons) Madagascar. Patients with face of the feet, ankles, and legs (1,4–6). chromoblastomycosis were older (47.9 years) than those Infection is caused by a lack of protective clothing without (37.5 years) (p = 0.0005). Chromoblastomyco- or shoes for persons working in rural areas in which sis was 3 times more likely to consist of leg lesions (p = 0.003). Molecular analysis identifiedFonsecaea nubica spiny plants are common. Chromoblastomycosis is in 23 cases and Cladophialophora carrionii in 7 cases. -
World Bank Document
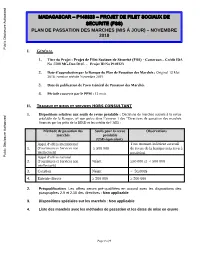
MADAGASCAR – P149323 – PROJET DE FILET SOCIAUX DE SECURITE (FSS) PLAN DE PASSATION DES MARCHES (MIS À JOUR) – NOVEMBRE 2018 Public Disclosure Authorized I. GÉNÉRAL 1. Titre du Projet : Projet de Filet Sociaux de Sécurité (FSS) - Cameroun – Crédit IDA No 5708 MG-Don D145 - Projet ID No P149323 2. Date d’approbation par la Banque du Plan de Passation des Marchés : Original 13 Mai 2016 ; version révisée Novembre 2018 3. Date de publication de l’avis Général de Passation des Marchés 4. Période couverte par le PPM : 12 mois Public Disclosure Authorized II. TRAVAUX ET BIENS ET SERVICES HORS CONSULTANT 1. Dispositions relatives aux seuils de revue préalable : Décisions de marchés soumis à la revue préalable de la Banque, tel que prévu dans l’annexe 1 des “Directives de passation des marchés financés par les prêts de la BIRD et les crédits de l’AID : Méthode de passation des Seuils pour la revue Observations marchés préalable (USD équivalent) Appel d’offres international Tout montant inférieur au seuil 1. (Fournitures et Services non ≥ 500 000 de revue de la banque sera revu à intellectuels) postériori Public Disclosure Authorized Appel d’offres national 2. (Fournitures et Services non Néant ≥50 000 et < 500 000 intellectuels) 3. Cotation Néant < 50,000$ 4. Entente directe ≥ 500 000 ≥ 500 000 2. Préqualification. Les offres seront pré-qualifiées en accord avec les dispositions des paragraphes 2.9 et 2.10 des directives : Non applicable 3. Dispositions spéciales sur les marchés : Non applicable 4. Liste des marchés avec les méthodes de passation et les dates de mise en œuvre Public Disclosure Authorized Page 1 of 9 II-1 TRAVAUX 1 2 3 4 5 6 7 8 9 Réf. -

World Bank Document
Sample Procurement Plan Public Disclosure Authorized I. General 1. Bank’s approval Date of the procurement Plan [Original: October 2016]: Revision 1 of Updated Procurement Plan, January 2017] 2. Date of General Procurement Notice: 15 July 2017 3. Period covered by this procurement plan: The procurement period of project covered from year January 2017 to December 2018 II. Goods and Works and non-consulting services. 1. Prior Review Threshold: Procurement Decisions subject to Prior Review by the Bank as Public Disclosure Authorized stated in Appendix 1 to the Guidelines for Procurement: Procurement Method Prior Review Threshold Comments US$ 1. ICB and LIB (Goods) Above US$ 500,000 All 2. NCB (Goods) Above US$ 780,000 All 3. ICB (Works) Above US$ 10 million All 4. NCB (Works) Above US$ 476,000 First contract 5. Consultation of the suppliers (Works) Above US$ 20,000 First contract 6. (Non-Consultant Services) Above US$ 10,000 First contract 6. Individual consultants Above US$ 19,200 All [Add other methods if necessary] Public Disclosure Authorized 2. Prequalification. Bidders for _Not applicable_ shall be prequalified in accordance with the provisions of paragraphs 2.9 and 2.10 of the Guidelines. 3. Proposed Procedures for CDD Components (as per paragraph. 3.17 of the Guidelines: 4. Reference to (if any) Project Operational/Procurement Manual: Project Implementation Manual for World Bank Loan Project under preparation. 5. Any Other Special Procurement Arrangements: 5 ICB works packages will be financed under Project preparation advance. Public Disclosure Authorized 6. Summary of the Procurement Packages planned during the first 18 months after project effectiveness PADAP August 22, 2017 1 2 3 4 5 6 7 Ref. -

World Bank Document
Plan de Passation de marchés I. Généralités 1. L'information sur le projet : Pays : Madagascar ; Public Disclosure Authorized Emprunteur : République de Madagascar ; Nom de projet : Projet Filets Sociaux de Sécurité – Financement Additionnel (P160 544) ; Numéro du Crédit : D1450-MG ; Agence d’exécution du Projet : Unité Programme National de Nutrition Communautaire. 2. Date d’approbation du Plan de passation de marchés par la Banque : - ; Révision : - ; 3. Date de notification du Plan Général de Passation de marchés : - ; Public Disclosure Authorized 4. Période couverte par le Plan de Passation de marchés : DOUZE (12) mois. II. Biens et Travaux et Services hors consultants 1. Seuil de Revue préalable : Les décisions de passation de marchés sujet aux revues préalables de la Banque comme indiqué dans le paragraphe 3.1 de l'Annexe II du Règlement de Passation des Marchés pour les Emprunteurs sollicitant le Financement de Projets d’Investissement (Juillet 2016) et sur la base de l'évaluation de la capacité de l'agence d’exécution : Public Disclosure Authorized Seuil de revue à Méthode de Passation de marchés Commentaires priori (USD) Les montants 1 Biens : AOI/AON/UN/ED 2 000 000 estimatifs des marchés prévus sont 2 Travaux : AOI/AON/ED 10 000 000 au-dessous des seuils. Services autres que consultants : Niveau de risque : 3 2 000 000 AOI/AON/UN/ED « SUBSTANTIEL » 2. Pré-qualification (selon les dispositions des paragraphes 6.19 à 6.24 de la Section VI du Règlement de Passation des Marchés pour les Emprunteurs sollicitant le Public Disclosure Authorized Financement de Projets d’Investissement (Juillet 2016)) : Non Applicable. -

Total Population in Antalaha, Maroantsetra, Andapa and Sambava Districts
MA005 Anaborano Tsarabaria Ifasy Ambinanin'andravory 0 16,418 Andravory 11,276 Ambodimanga 4,616 Ampanefena Amboriala Ambodisambalahy 19,962 Ramena 9,800 Tanambao Manambato 12,649 10,418 Daoud Ambohitrandriana 5,237 9,106 5,358 Antananarivo Antsirabe Antsahavaribe Belambo Nord 13,390 7,632 40,146 Bevonotra Anjialava 7,716 Antindra Marotolana 12,653 16,706 11,734 Anjangoveratra Amboangibe 16,539 Ambatoafo 12,940 Marogaona Bemanevika Anjialavabe 10,453 6,813 10,447 6,621 Analamaho Nosiarina Andrembona 4,789 4,959 Mangindrano 4,930 Antananivo Anjinjaomby Sambava Cu 8,488 41,672 Haut Ambohimitsinjo 5,942 2,063 6,327 Ambohimalaza Ambovonomby Doany Andrahanjo Ambodivoara 8,208 Ambararatabe 7,364 15,569 0 9,703 Andratamarina Nord Morafeno 6,885 4,196 10,482 Farahalana Anjozoromadosy Ambodiampana 21,232 Analila 6,013 Maroambihy 11,530 Marojala 7,505 Ambalamanasy II 11,941 14,847 Bealanana 14,515 Marovato 18,603 Ambatoriha Antsambaharo Betsakotsako 4,787 Est Ankazotokana 3,593 Andranotsara Belaoka 12,737 3,978 7,472Andranomena Belaoka Lokoho Lanjarivo Ambodiangezoka 5,862 Ambinanifaho Marovato 5,828 14,813 26,294 10,451 Ambatosia Matsohely 5,662 12,796 Marotolana 5,841 Andapa Andrakata Ambodiadabo M Ankiakabe 8,133 Ambalaromba 21,952 6,750 7,851 Bealampona Nord Ambararata 5,271 13,425 7,478 Antsambalahy Ampahana Sofia 8,597 19,424 3,144 Anoviara Ambodimanga I 12,033 9,326 Tanandava 8,065 Antsahanoro Sarahandrano 12,446 Ambodisikidy 5,574 7,188 Antananambo Antalaha Ambonivohitra Matsondakana Antsahamena 13,423 Andampy 34,994 42,264 4,793 -

DISTRICT COMMUNE NOMBRE CANDIDATS ENTITE NOM ET PRENOM(S) CANDIDATS ANDAPA AMBALAMANASY II 1 INDEPENDANT RAMANANKEVITRA (Ramanan
NOMBRE DISTRICT COMMUNE ENTITE NOM ET PRENOM(S) CANDIDATS CANDIDATS INDEPENDANT RAMANANKEVITRA ANDAPA AMBALAMANASY II 1 RAMANANKEVITRA (Ramanankevitra) IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA AMBALAMANASY II 1 RANDRIAMINO Rajoelina) INDEPENDANT A.T.M (Ambodiangezoka ANDAPA AMBODIANGEZOKA 1 TOMBOZANANY Raziliarivony Jolin Mandroso no Tanjogno) IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA AMBODIANGEZOKA 1 RAHARIMANANA James Willy Rajoelina) INDEPENDANT RAZAFIMANDIANINA ANDAPA AMBODIANGEZOKA 1 RAZAFIMANDIANINA (Razafimandianina) ANDAPA AMBODIMANGA I 1 AHI (Hiaraka Isika) RAZAKA Philibert IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA AMBODIMANGA I 1 ZARASON Eric Rajoelina) ANDAPA AMBODIMANGA I 1 MMM (Malagasy Miara - Miainga) CLEMENT Théophile INDEPENDANT ANDAPA ANDAPA 1 ANDRIANAIVOMANAMANDIMBY BIEN AIME ANDRIANAIVOMANAMANDIMBY Bien Aimé (Andrianaivomanamandimby Bien Aime) INDEPENDANT MIMARA DOSY FRANCO ANDAPA ANDAPA 1 MIMARA Dosy Franco (Mimara Dosy Franco) INDEPENDANT MEVA JEAN CLAUDE (Meva Jean ANDAPA ANDAPA 1 MEVA Jean Claude Claude) IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA ANDAPA 1 TSIMIBO Achille Rajoelina) INDEPENDANT RAMAHAVITA HENRI BRUNO ANDAPA ANDAPA 1 RAMAHAVITA Henri Bruno (Ramahavita Henri Bruno) ANDAPA ANDRAKATA 1 LEADER FANILO (Leader Fanilo) LEONG Anita IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA ANDRAKATA 1 RAHELISON Alexandre Rajoelina) ANDAPA ANDRAKATA 1 INDEPENDANT F.H.F (STANISLAS Eniole) STANISLAS Eniole IRK (Isika Rehetra Miaraka Amin'ny Andry ANDAPA ANDRANOMENA 1 RANDRIAMANANTENA Fidelin Gitorix -

Consultation Régionale Pour La Spatialisation Et Priorisation Des Activités En Vue De L’Élaboration De La Stratégie Régionale REDD+
Consultation régionale pour la spatialisation et priorisation des activités en vue de l’élaboration de la Stratégie Régionale REDD+ RAPPORT DES ATELIERS DE CONSULTATION Par Décembre 2017 1 TABLE DES MATIERES 1. INTRODUCTION _______________________________________________ 11 2. METHODOLOGIE POUR LA CONDUITE DE LA SPATIALISATION, FAISABILITE, PRIORISATION ET PLANIFICATION DES ACTIVITES _________ 12 2.1. Approche méthodologique ________________________________________________________ 12 2.1.1. Spatialisation et faisabilité des activités _________________________________________ 12 2.1.2. Priorisation et planification des activités ________________________________________ 14 3. RESULTATS DES ATELIERS REGIONAUX __________________________ 15 3.1. Région Alaotra Mangoro __________________________________________________________ 15 3.1.1. Problématique de la Région ___________________________________________________ 15 3.1.2. Potentialités de la Région _____________________________________________________ 15 3.1.3. Principales contraintes _______________________________________________________ 15 3.1.4. Activités proposées __________________________________________________________ 16 3.1.5. Priorisation des activités ______________________________________________________ 16 3.2. Région Analanjirofo ______________________________________________________________ 18 3.2.1. Problématiques de la Région __________________________________________________ 18 3.2.2. Potentialités de la Région ____________________________________________________ 18 3.2.3. -

Enquête De Base Sur Le Travail Des Enfants Dans La Région SAVA De Madagascar
Enquête de base sur le travail des enfants dans la région SAVA de Madagascar Rapport simplifié Août 2020 Enquête de base sur le travail des enfants dans la région SAVA de Madagascar Rapport simplifié Août 2020 Copyright © Organisation internationale du Travail 2020 Première édition 31 Août 2020 Les publications du Bureau international du Travail jouissent de la protection du droit d’auteur en vertu du protocole no 2, annexe à la Convention universelle pour la protection du droit d’auteur. Toutefois, de courts passages pourront être reproduits sans autorisation, à la condition que leur source soit dûment mentionnée. Toute demande d’autorisation de reproduction ou de traduction devra être envoyée à Publications du BIT (Droits et licences), Bureau international du Travail, CH-1211 Genève 22, Suisse, ou par courriel à [email protected]. Ces demandes seront toujours les bienvenues. Bibliothèques, institutions et autres utilisateurs enregistrés auprès d’un organisme de gestion des droits de reproduction ne peuvent faire des copies qu’en accord avec les conditions et droits qui leur ont été octroyés. Consultez le site www.ifrro.org afin de trouver l’organisme responsable de la gestion des droits de reproduction dans votre pays. ISBN Print: 9789220328842 ISBN Web PDF: 9789220328835 Egalement disponible en Anglais : ‘’Baseline survey of child labour in the SAVA Region of Madagascar : Streamlined report”, ISBN Print : 9789220327951 – ISBN Web PDF : 9789220327944. Les désignations utilisées dans les publications du BIT, qui sont conformes à la pratique des Nations Unies, et la présentation des données qui y figurent n’impliquent de la part du Bureau international du Travail aucune prise de position quant au statut juridique de tel ou tel pays, zone ou territoire, ou de ses autorités, ni quant au tracé de ses frontières. -

World Bank Document
MADAGASCAR – P149323 – PROJET DE FILET SOCIAUX DE SECURITE (FSS) PLAN DE PASSATION DES MARCHES (MIS À JOUR) – NOVEMBRE 2018 Public Disclosure Authorized I. GÉNÉRAL 1. Titre du Projet : Projet de Filet Sociaux de Sécurité (FSS) - Cameroun – Crédit IDA No 5708 MG-Don D145 - Projet ID No P149323 2. Date d’approbation par la Banque du Plan de Passation des Marchés : Original 13 Mai 2016 ; version révisée Novembre 2018 3. Date de publication de l’avis Général de Passation des Marchés 4. Période couverte par le PPM : 12 mois Public Disclosure Authorized II. TRAVAUX ET BIENS ET SERVICES HORS CONSULTANT 1. Dispositions relatives aux seuils de revue préalable : Décisions de marchés soumis à la revue préalable de la Banque, tel que prévu dans l’annexe 1 des “Directives de passation des marchés financés par les prêts de la BIRD et les crédits de l’AID : Méthode de passation des Seuils pour la revue Observations marchés préalable (USD équivalent) Appel d’offres international Tout montant inférieur au seuil 1. (Fournitures et Services non ≥ 500 000 de revue de la banque sera revu à intellectuels) postériori Public Disclosure Authorized Appel d’offres national 2. (Fournitures et Services non Néant ≥50 000 et < 500 000 intellectuels) 3. Cotation Néant < 50,000$ 4. Entente directe ≥ 500 000 ≥ 500 000 2. Préqualification. Les offres seront pré-qualifiées en accord avec les dispositions des paragraphes 2.9 et 2.10 des directives : Non applicable 3. Dispositions spéciales sur les marchés : Non applicable 4. Liste des marchés avec les méthodes de passation et les dates de mise en œuvre Public Disclosure Authorized Page 1 of 9 II-1 TRAVAUX 1 2 3 4 5 6 7 8 9 Réf.