Synthetic Materials with Redox-Triggers for Imaging and Drug Delivery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kinetics and Mechanism of Polythionate Oxidation to Sulfate at Low Ph by O2 and Fe3+
Geochimica et Cosmochimica Acta, Vol. 67, No. 23, pp. 4457–4469, 2003 Copyright © 2003 Elsevier Ltd Pergamon Printed in the USA. All rights reserved 0016-7037/03 $30.00 ϩ .00 doi:10.1016/S0016-7037(03)00388-0 3؉ Kinetics and mechanism of polythionate oxidation to sulfate at low pH by O2 and Fe 1, 2 1,2 GREGORY K. DRUSCHEL, *ROBERT J. HAMERS, and JILLIAN F. BANFIELD † 1Departments of Geology and Geophysics and 2Chemistry, University of Wisconsin-Madison, Madison, WI 53706 USA (Received October 16, 2002; accepted in revised form May 30, 2003) 2Ϫ Abstract—Polythionates (SxO6 ) are important in redox transformations involving many sulfur compounds. Here we investigate the oxidation kinetics and mechanisms of trithionate and tetrathionate oxidation between pH 0.4 and pH 2 in the presence of Fe3ϩ and/or oxygen. In these solutions, Fe3ϩ plus oxygen oxidizes tetrathionate and trithionate at least an order of magnitude faster than oxygen alone. Kinetic measurements, coupled with density functional calculations, suggest that the rate-limiting step for tetrathionate oxidation involves Fe3ϩ attachment, followed by electron density shifts that result in formation of a sulfite radical and 0 S3O3 derivatives. The overall reaction orders for trithionate and tetrathionate are fractional due to rearrange- ment reactions and side reactions between reactants and intermediate products. The pseudo-first order rate coefficients for tetrathionate range from 10Ϫ11 sϪ1 at 25°C to 10Ϫ8 sϪ1 at 70°C, compared to 2 ϫ 10Ϫ7 sϪ1 Ϯ at 35 °C for trithionate. The apparent activation energy (EA) for tetrathionate oxidation at pH 1.5 is 104.5 4.13 kJ/mol. -

Treatment of Spent Caustic from Sodium Dithionate Industry Effluent Using Electrochemical Membrane Cell
ISSN: 2319-8753 International Journal of Innovative Research in Science, Engineering and Technology (An ISO 3297: 2007 Certified Organization) Vol. 3, Issue 7, July 2014 Treatment of Spent Caustic from Sodium Dithionate Industry Effluent using Electrochemical Membrane Cell S.A.T.Shanmugapriya1, Lashmipriya2 Assistant Professor, Department of Chemistry, Alagappa Chettiar College of Engineering and Technology, Karaikudi, Tamilnadu, India1 P.G. Scholar, Alagappa Chettiar College of Engineering and Technology, Karaikudi, Tamilnadu, India2 ABSTRACT: In this paper treatment of caustic from Sodium dithionate industry effluent is presented. Sodium dithionate industry effluent very harmful to environment in many ways. Effluent can contaminate soil and ground water if landfilling is adopted. It will also decrease dissolved oxygen in water bodies and harmful to aquatic organisms. Effluent will affect the agricultural field, irrigation water source as well as drinking water. Incineration of residues from industry will leads to acid rain because they contain sulfur compounds. So the treatment before disposal of effluent is necessary . From the characterization study concluded that treatment is necessary for the effluent before disposal. Among various methods for industrial waste water treatment electrochemical membrane process was selected because of its attractiveness & economical method. The study was carried out using TSIA anode ( System I) and Pt/Ti anodes (System II) . In system I, experiment was carried out in a constant current density of 50 mA/cm2 at 4 hour duration. The variation of potential, pH, concentration of sodium thiosulfate, sodium formate and sodium hydroxide with respect to time were analysed. Since chemical and electrochemical reactions takes place in system I, recovered products from system I were caustic, sulfate and sulfur. -

Deracemization of Sodium Chlorate with Or Without the Influence of Sodium Dithionate Manon Schindler
Deracemization of sodium chlorate with or without the influence of sodium dithionate Manon Schindler To cite this version: Manon Schindler. Deracemization of sodium chlorate with or without the influence of sodium dithionate. Cristallography. Normandie Université, 2020. English. NNT : 2020NORMR004. tel- 02521046v2 HAL Id: tel-02521046 https://tel.archives-ouvertes.fr/tel-02521046v2 Submitted on 15 May 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. THÈSE Pour obtenir le diplôme de doctorat Spécialité Physique Préparée au sein de l’Université de Rouen Normandie Deracémisation du chlorate de sodium avec et sans l’influence du dithionate de sodium Présentée et soutenue par Manon SCHINDLER Thèse soutenue publiquement le 13 mars 2020 devant le jury composé de Mme. Elizabeth HILLARD Dr. Hab. Université de Bordeaux Rapporteur M. Elias VLIEG Pr. Université Radboud de Nimègue Rapporteur Mme. Sylvie MALO Pr. Université de Caen Normandie Présidente M. Woo Sik KIM Pr. Université Kyung Hee de Séoul Examinateur M. Gérard COQUEREL Pr. Université de Rouen Normandie Directeur de thèse Thèse dirigée par Gérard COQUEREL, professeur des universités au laboratoire Sciences et Méthodes Séparatives (EA3233 SMS) THÈSE Pour obtenir le diplôme de doctorat Spécialité Physique Préparée au sein de l’Université de Rouen Normandie Deracemization of sodium chlorate with or without the influence of sodium dithionate Présentée et soutenue par Manon SCHINDLER Thèse soutenue publiquement le 13 mars 2020 devant le jury composé de Mme. -

WO 2012/024294 Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date Λ 23 February 2012 (23.02.2012) WO 2012/024294 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every C22B 47/00 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, (21) International Application Number: CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, PCT/US201 1/047916 DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, 16 August 201 1 (16.08.201 1) KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (25) Filing Language: English NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 61/374,691 18 August 2010 (18.08.2010) US (84) Designated States (unless otherwise indicated, for every (71) Applicant (for all designated States except US): AMER¬ kind of regional protection available): ARIPO (BW, GH, ICAN MANGANESE INC. [CA/US]; 2533 North Car GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, son Street, Suite 3913, Carson City, NV 89706 (US). -

The Use of Glucose As Ecological Reducing Agent for Sulphur Dyes: Optimization of Experimental Conditions
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by European Scientific Journal (European Scientific Institute) European Scientific Journal June 2014 edition vol.10, No.18 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 THE USE OF GLUCOSE AS ECOLOGICAL REDUCING AGENT FOR SULPHUR DYES: OPTIMIZATION OF EXPERIMENTAL CONDITIONS Romdhani Zouhaier Dhouib Sofiène Sakli Faouzi Laboratory of Textile Research, ISET of Ksar, Hellal, Monastir, Tunisia Abstract At the present time, dyeing of textile material requires the use of various auxiliaries. These used agents have adverse effects on the environment. In general, for the dyeing with sulphur dyes, a reducing agent is used to transform the dye molecule to a water soluble leuco form that can diffuse into the fibre. In this study, three reducing agents were used : the sodium sulphide, sodium dithionite and glucose as an environmentally friendly reducer. To compare their effect on the reduction of the sullphur dyestuff, the redox potential, pH and the colour yield (K/S) were measured according to the concentration of reducing agent and caustic soda concentration. Results of leuco sulphur black B reduction by the different reducing agents were evaluated by measuring the colour yield (K/S) and the brightness variation after the washing process. The obtained results showed that glucose can offer some scientifically results similar to those done with sodium sulphide which can give for the reduction of sulphur dyestuff Keywords: Sulphur dye, Dyeing, Reduction, Reducing Agent, Glucose Introduction Cellulosic substrates especially cotton, rayon, and paper, are very hydrophilic and, therefore, require hydrophilic soluble dyes for their coloration from a dye bath. -
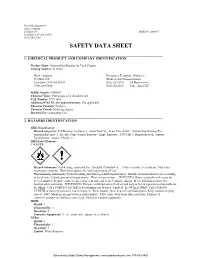
Safety Data Sheet
World Headquarters Hach Company P.O.Box 389 MSDS No: M00107 Loveland, CO USA 80539 (970) 669-3050 SAFETY DATA SHEET _____________________________________________________________________________ 1. CHEMICAL PRODUCT AND COMPANY IDENTIFICATION Product Name: Hydrosulfite Reagent for Total Copper Catalog Number: 2118869 Hach Company Emergency Telephone Numbers: P.O.Box 389 (Medical and Transportation) Loveland, CO USA 80539 (303) 623-5716 24 Hour Service (970) 669-3050 (515)232-2533 8am - 4pm CST MSDS Number: M00107 Chemical Name: Dithionous acid, disodium salt CAS Number: 7775-14-6 Additional CAS No. (for hydrated forms): Not applicable Chemical Formula: Na2S2O4 Chemical Family: Reducing Agent Intended Use: Laboratory Use _____________________________________________________________________________ 2. HAZARDS IDENTIFICATION GHS Classification: Hazard categories: Self Heating: Self-heat. 1 Acute Toxicity: Acute Tox. 4-Orl . Serious Eye Damage/Eye Irritation:Eye Irrit. 2 Specific Target Organ Toxicity - Single Exposure: STOT SE 3 Hazardous to the Aquatic Environment: Aquatic Chronic 3 GHS Label Elements: DANGER Hazard statements: Self-heating: maycatch fire. Harmful if swallowed. Causes serious eye irritation. May cause respiratory irritation. Harmful to aquatic life with long lasting effects. Precautionary statements: Avoid breathing dust/fume/gas/mist/vapours/spray. Handle environmental release according to local, state, federal, provincial requirements. Wear eye protection. IF IN EYES: Rinse cautiously with water for several minutes. Remove contact lenses, if present and easy to do. Continue rinsing. If eye irritation persists: Get medical advice/attention. IF INHALED: Remove victim/person to fresh air and keep at rest in a position comfortable for breathing. Call a POISON CENTER or doctor/physician if you feel unwell. IF SWALLOWED: Call a POISON CENTER or doctor/physician if you feel unwell. -

Chemical Names and CAS Numbers Final
Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number C3H8O 1‐propanol C4H7BrO2 2‐bromobutyric acid 80‐58‐0 GeH3COOH 2‐germaacetic acid C4H10 2‐methylpropane 75‐28‐5 C3H8O 2‐propanol 67‐63‐0 C6H10O3 4‐acetylbutyric acid 448671 C4H7BrO2 4‐bromobutyric acid 2623‐87‐2 CH3CHO acetaldehyde CH3CONH2 acetamide C8H9NO2 acetaminophen 103‐90‐2 − C2H3O2 acetate ion − CH3COO acetate ion C2H4O2 acetic acid 64‐19‐7 CH3COOH acetic acid (CH3)2CO acetone CH3COCl acetyl chloride C2H2 acetylene 74‐86‐2 HCCH acetylene C9H8O4 acetylsalicylic acid 50‐78‐2 H2C(CH)CN acrylonitrile C3H7NO2 Ala C3H7NO2 alanine 56‐41‐7 NaAlSi3O3 albite AlSb aluminium antimonide 25152‐52‐7 AlAs aluminium arsenide 22831‐42‐1 AlBO2 aluminium borate 61279‐70‐7 AlBO aluminium boron oxide 12041‐48‐4 AlBr3 aluminium bromide 7727‐15‐3 AlBr3•6H2O aluminium bromide hexahydrate 2149397 AlCl4Cs aluminium caesium tetrachloride 17992‐03‐9 AlCl3 aluminium chloride (anhydrous) 7446‐70‐0 AlCl3•6H2O aluminium chloride hexahydrate 7784‐13‐6 AlClO aluminium chloride oxide 13596‐11‐7 AlB2 aluminium diboride 12041‐50‐8 AlF2 aluminium difluoride 13569‐23‐8 AlF2O aluminium difluoride oxide 38344‐66‐0 AlB12 aluminium dodecaboride 12041‐54‐2 Al2F6 aluminium fluoride 17949‐86‐9 AlF3 aluminium fluoride 7784‐18‐1 Al(CHO2)3 aluminium formate 7360‐53‐4 1 of 75 Chemical Abstract Chemical Formula Chemical Name Service (CAS) Number Al(OH)3 aluminium hydroxide 21645‐51‐2 Al2I6 aluminium iodide 18898‐35‐6 AlI3 aluminium iodide 7784‐23‐8 AlBr aluminium monobromide 22359‐97‐3 AlCl aluminium monochloride -

The Use of Glucose As Ecological Reducing Agent for Sulphur Dyes: Optimization of Experimental Conditions
European Scientific Journal June 2014 edition vol.10, No.18 ISSN: 1857 – 7881 (Print) e - ISSN 1857- 7431 THE USE OF GLUCOSE AS ECOLOGICAL REDUCING AGENT FOR SULPHUR DYES: OPTIMIZATION OF EXPERIMENTAL CONDITIONS Romdhani Zouhaier Dhouib Sofiène Sakli Faouzi Laboratory of Textile Research, ISET of Ksar, Hellal, Monastir, Tunisia Abstract At the present time, dyeing of textile material requires the use of various auxiliaries. These used agents have adverse effects on the environment. In general, for the dyeing with sulphur dyes, a reducing agent is used to transform the dye molecule to a water soluble leuco form that can diffuse into the fibre. In this study, three reducing agents were used : the sodium sulphide, sodium dithionite and glucose as an environmentally friendly reducer. To compare their effect on the reduction of the sullphur dyestuff, the redox potential, pH and the colour yield (K/S) were measured according to the concentration of reducing agent and caustic soda concentration. Results of leuco sulphur black B reduction by the different reducing agents were evaluated by measuring the colour yield (K/S) and the brightness variation after the washing process. The obtained results showed that glucose can offer some scientifically results similar to those done with sodium sulphide which can give for the reduction of sulphur dyestuff Keywords: Sulphur dye, Dyeing, Reduction, Reducing Agent, Glucose Introduction Cellulosic substrates especially cotton, rayon, and paper, are very hydrophilic and, therefore, require hydrophilic soluble dyes for their coloration from a dye bath. Current dyes designed for cellulosic polymers are direct, vat, sulfur, and reactive dyes. Sulphur dyes are one of the less costs of all dye classes used on cellulosic fibres and their blends (Senior & Clarke, 1986). -

Regolith Weathering and Sorption Influences Molybdenum, Vanadium, and Chromium Export Via Stream Water at Four Granitoid Critica
feart-06-00193 November 8, 2018 Time: 16:14 # 1 ORIGINAL RESEARCH published: 09 November 2018 doi: 10.3389/feart.2018.00193 Regolith Weathering and Sorption Influences Molybdenum, Vanadium, and Chromium Export via Stream Water at Four Granitoid Critical Zone Observatories Justin B. Richardson1,2* and Elizabeth K. King3 1 Department of Geosciences, University of Massachusetts Amherst, Amherst, MA, United States, 2 Earth and Atmospheric Sciences, College of Agriculture and Life Sciences, Cornell University, Ithaca, NY, United States, 3 Department of Earth, Ocean, and Atmospheric Sciences, University of British Columbia, Vancouver, BC, Canada Understanding the fate of oxyanions in the Critical Zone is important because of Edited by: their biological significance and the potential for their use as geochemical tracers in Julia Perdrial, University of Vermont, United States terrestrial environments and subsurface systems. This study assessed the partitioning Reviewed by: and transport of a suite of oxyanion metals (Mo, V, and Cr) in regolith profiles and stream Angelica Vazquez-Ortega, waters from four granitoid Critical Zone Observatories (CZOs) (Boulder Creek, Calhoun, Bowling Green State University, United States Luquillo, and Southern Sierra). For regolith profiles, we compared Mo, V, and Cr in Dragos George Zaharescu, total digestions and two extractions targeting oxyanions adsorbed to organic matter Georgia Institute of Technology, and amorphous oxides (H O C 0.1 M acetic acid) and secondary Fe oxides (citrate– United States 2 2 bicarbonate–dithionite). Total Mo, V, and Cr ranged from 0.4 to 2.5 mg kg−1, 16 to *Correspondence: −1 −1 Justin B. Richardson 208 mg kg , and 0.2 to 55 mg kg , respectively. -

January-February 2009 Volume 31 No
The News Magazine of the International Union of Pure and Applied Chemistry (IUPAC) CHEMISTRY International January-February 2009 Volume 31 No. 1 The IUPAC International Periodic Tables Chemical Identifier and IUPAC Celebrating Worldwide Excellence in Chemistry From the Editor CHEMISTRY International omething old, something new, something borrowed, something blue . Sthat recipe is for something else, yet it applies surprisingly well to the The News Magazine of the International Union of Pure and contents of this issue of Chemistry International. Applied Chemistry (IUPAC) Something old would be the description of IUPAC’s position with regard to the periodic table. The feature article by Jeffery Leigh (page 4) www.iupac.org/publications/ci reminds the reader that “IUPAC’s primary concern is with unequivo- Managing Editor: Fabienne Meyers cal and unambiguous commu- Production Editor: Chris Brouwer nication,” and in the context of Design: CB Communications a periodic table format, IUPAC’s recommendation is only for the All correspondence to be addressed to: groups numbering from 1 to 18, and Fabienne Meyers no more. Leigh demonstrates that IUPAC, c/o Department of Chemistry one table does not fit all uses, and Boston University the periodic table as we know it today is an icon often wrongly associ- Metcalf Center for Science and Engineering ated with IUPAC. 590 Commonwealth Ave. Something new would be the focus of Steve Heller and Alan Boston, MA 02215, USA McNaught’s article (page 7) on InChI, known as “in-chee.” The IUPAC International Chemical Identifier (InChI) continues to be developed and E-mail: [email protected] is becoming more widely used throughout the chemistry community. -

United States Patent (19. 11) 4,059,533 Watson Et Al
United States Patent (19. 11) 4,059,533 Watson et al. 45 Nov. 22, 1977 (54) OXYGENSCAVENGING METHODS AND 3,399,725 9/1968 Pye ....................................... 166/275 ADDITIVES 3,852,201 12/1974 Jackson ................................. 252/8.5 (75 Inventors: Jimmie L. Watson; Leroy L. Carney, FOREIGN PATENT DOCUMENTS both of Duncan, Okla. 6,414,645 6/1965 Netherlands .......................... 252/8.5 (73) Assignee: Halliburton Company, Duncan, Okla. OTHER PUBLICATIONS (21) Appl. No.: 518,306 The Merck Index, Eighth Edition, Published 1968 by 22 Filed: Oct. 29, 1974 - Merck and Co., Inc., pp. 958 and 960. 51) Int. Cl.2 ....... e o os see s see a woo C09K 7/02; C09K 7/04; Primary Examiner-Herbert B. Guynn E21B 43/22; CO1B 17/66 Attorney, Agent, or Firm-Robert S. Nisbett; Thomas R. 52 U.S. C. ................................... 252/8.5A; 175/64; Weaver; John H. Tregoning 252/8.5 B; 252/8.55 B; 252/188 58) Field of Search .............. 252/8.5 A, 8.5 B, 8.5 C, 57 ABSTRACT 252/8.55 D, 188; 166/279, 310, 175/64; This invention relates to methods and additives for 423/515, 512 R, 265 scavenging oxygen dissolved and entrained in liquids (56) References Cited which are particularly suitable for removing dissolved and entrained oxygen from polymer-containing fluids U.S. PATENT DOCUMENTS used in drilling and completing well bores as well as 1,810,663 6/1931 Kritchevsky et al................ 252/188 water flood and other procedures carried out in the oil 1,810,665 6/1931 Kritchevsky et al. -

US 2002/0002128A1 Gernon Et Al
US 2002.0002128A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2002/0002128A1 Gernon et al. (43) Pub. Date: Jan. 3, 2002 (54) AQUEOUS SOLUTIONS CONTAINING Related U.S. Application Data DITHIONIC ACID AND/OR METAL DTHONATE (63) Non-provisional of provisional application No. 60/186,097, filed on Mar. 1, 2000. (76) Inventors: Michael D. Gernon, Upper Providence, Publication Classification PA (US); Sandra L. Bodar, 7 Coulommiers (FR) (51) Int. Cl." ....................................................... C11D 1100 (52) U.S. Cl. .............................................................. 510,363 Correspondence Address: Gilbert W. Rudman (57) ABSTRACT ATOFINA Chemicals, Inc., Patent Department This invention relates to Solutions of dithionic acid and/or 26th Floor dithionate Salts for use in metal finishing processes Such as 2000 Market Street those used for the cleaning, activating, electroplating, elec Philadelphia, PA 19103-3222 (US) troless plating, conversion coating and/or other pre-treat ment or post-treatment of a metallic Surface. In particular the (21) Appl. No.: 09/791,224 Solutions are a useful electrolyte for the electroplating of metallic coatings, especially, Sn, Cu, Ni, Zn and precious (22) Filed: Feb. 22, 2001 metals, onto metal or plastic Substrates and/or other Surfaces. US 2002/0002128A1 Jan. 3, 2002 AQUEOUS SOLUTIONS CONTAINING DITHIONIC 0014) Another embodiment is a surface cleaning solution ACID AND/OR METAL DITHIONATE composition for a Substrate, other than copper, which con tains metal or ammonium dithionate Salts. REFERENCE TO RELATED APPLICATION 0015. Another embodiment is an aqueous solution of 0001. This application claims the benefit of United States ammonium, IA metal and/or IIA metal dithionate Salts for Provisional Application Ser.