Acute Treatment of Pulmonary Embolism Part 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pleural Effusion and Ventilation/Perfusion Scan Interpretation for Acute Pulmonary Embolus
ventricular function by radionuclide angiography during exercise in normal subjects 33. Verani MS. Myocardial perfusion imaging versus two-dimensional echocardiography: and patients with chronic coronary heart disease. J Am Coll Cardiol 1983;1:1518- comparative value in the diagnosis of coronary artery disease. J NucÃCardiol 1529. 1994;1:399-414. 29. Adam WE. Tarkowska A, Bitter F, Stauch M, Geffers H. Equilibrium (gated) 34. Foster T, McNeill AJ, Salustri A, et al. Simultaneous dobutamine stress echocardiog radionuclide ventriculography. Cardiovasc Radial 1979;2:161-173. raphy and technetium-99m SPECT in patients with suspected coronary artery disease. 30. Hurwitz RA, TrêvesS, Kuroc A. Right ventricular and left ventricular ejection fraction J Am Coll Cardiol I993;21:1591-I596. in pediatrie patients with normal hearts: first pass radionuclide angiography. Am 35. Marwick TH, D'Hondt AM, Mairesse GH, Baudhuin T, Wijins W, Detry JM, Meiin Heart J 1984;107:726-732. 31. Freeman ML, Palac R, Mason J, et al. A comparison of dobutamine infusion and JA. Comparative ability of dobutamine and exercise stress in inducing myocardial ischemia in active patients. Br Heart J 1994:72:31-38. supine bicycle exercise for radionuclide cardiac stress testing. Clin NucÃMed 1984:9:251-255. 36. Senior R, Sridhara BS, Anagnostou E, Handler C, Raftery EB, Lahiri A. Synergistic 32. Cohen JL, Greene TO, Ottenweller J, Binebaum SZ, Wilchfort SD, Kim CS. value of simultaneous stress dobutamine sestamibi single-photon-emission computer Dobutamine digital echocardiography for detecting coronary artery disease. Am J ized tomography and echocardiography in the detection of coronary artery disease. -

Diagnosing Pulmonary Embolism M Riedel
309 Postgrad Med J: first published as 10.1136/pgmj.2003.007955 on 10 June 2004. Downloaded from REVIEW Diagnosing pulmonary embolism M Riedel ............................................................................................................................... Postgrad Med J 2004;80:309–319. doi: 10.1136/pgmj.2003.007955 Objective testing for pulmonary embolism is necessary, embolism have a low long term risk of subse- quent VTE.2 5–7 because clinical assessment alone is unreliable and the consequences of misdiagnosis are serious. No single test RISK FACTORS AND RISK has ideal properties (100% sensitivity and specificity, no STRATIFICATION risk, low cost). Pulmonary angiography is regarded as the The factors predisposing to VTE broadly fit Virchow’s triad of venous stasis, injury to the final arbiter but is ill suited for diagnosing a disease vein wall, and enhanced coagulability of the present in only a third of patients in whom it is suspected. blood (box 1). The identification of risk factors Some tests are good for confirmation and some for aids clinical diagnosis of VTE and guides decisions about repeat testing in borderline exclusion of embolism; others are able to do both but are cases. Primary ‘‘thrombophilic’’ abnormalities often non-diagnostic. For optimal efficiency, choice of the need to interact with acquired risk factors before initial test should be guided by clinical assessment of the thrombosis occurs; they are usually discovered after the thromboembolic event. Therefore, the likelihood of embolism and by patient characteristics that risk of VTE is best assessed by recognising the may influence test accuracy. Standardised clinical presence of known ‘‘clinical’’ risk factors. estimates can be used to give a pre-test probability to However, investigations for thrombophilic dis- orders at follow up should be considered in those assess, after appropriate objective testing, the post-test without another apparent explanation. -

Venous Air Embolism, Result- Retrospective Study of Patients with Venous Or Arterial Ing in Prompt Hemodynamic Improvement
Ⅵ REVIEW ARTICLE David C. Warltier, M.D., Ph.D., Editor Anesthesiology 2007; 106:164–77 Copyright © 2006, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Diagnosis and Treatment of Vascular Air Embolism Marek A. Mirski, M.D., Ph.D.,* Abhijit Vijay Lele, M.D.,† Lunei Fitzsimmons, M.D.,† Thomas J. K. Toung, M.D.‡ exogenously delivered gas) from the operative field or This article has been selected for the Anesthesiology CME Program. After reading the article, go to http://www. other communication with the environment into the asahq.org/journal-cme to take the test and apply for Cate- venous or arterial vasculature, producing systemic ef- gory 1 credit. Complete instructions may be found in the fects. The true incidence of VAE may be never known, CME section at the back of this issue. much depending on the sensitivity of detection methods used during the procedure. In addition, many cases of Vascular air embolism is a potentially life-threatening event VAE are subclinical, resulting in no untoward outcome, that is now encountered routinely in the operating room and and thus go unreported. Historically, VAE is most often other patient care areas. The circumstances under which phy- associated with sitting position craniotomies (posterior sicians and nurses may encounter air embolism are no longer fossa). Although this surgical technique is a high-risk limited to neurosurgical procedures conducted in the “sitting procedure for air embolism, other recently described position” and occur in such diverse areas as the interventional radiology suite or laparoscopic surgical center. Advances in circumstances during both medical and surgical thera- monitoring devices coupled with an understanding of the peutics have further increased concern about this ad- pathophysiology of vascular air embolism will enable the phy- verse event. -
An Interesting Case of Undiagnosed Pleural Effusion Case Report
Amit Panjwani, Thuraya Zaid [email protected] Pulmonary Medicine, Salmaniya Medical Complex, Manama, Bahrain. An interesting case of undiagnosed pleural effusion Case report Pleural effusions are commonly encountered in the Investigations revealed a haemoglobin level Cite as: Panjwani A, Zaid T. clinical practise of both respiratory and nonrespiratory of 16.4 g⋅dL−1, and total leukocyte count of An interesting case of specialists. An estimated 1–1.5 million new cases in 8870 cells⋅mm−3 with a differential count of 62% undiagnosed pleural effusion. the USA and 200 000–250 000 new cases of pleural neutrophils, 28% lymphocytes, 7% monocytes, 2% Breathe 2017; 13: e46–e52. effusions are reported from the UK each year [1]. eosinophils and 1% basophils. The platelet count Analysis of the relevant clinical history, physical was 160 000 cells⋅mm−3. Creatinine, electrolytes examination, chest radiography and diagnostic and liver function tests were normal. The ECG was thoracentesis is useful in identifying the cause of unremarkable and cardiac enzymes were within pleural effusion in majority of the cases [2]. In a few normal limits. Chest radiograph (figure 1) showed a cases, the aetiology may be unclear after the initial mild, right-sided pleural effusion, blunting of the left assessment. The list of diseases that may account for costophrenic angle, no shift of mediastinal position a persistent undiagnosed pleural effusion is long [3]. and no lung parenchymal opacities. We present an interesting case of undiagnosed pleural effusion that was encountered in our hospital. R Case presentation A 33-year-old male presented to our hospital with a history of sudden-onset, pleuritic, right-sided chest pain of 2 days’ duration. -

Diagnosis of Chronic Thromboembolic Pulmonary Hypertension After Acute Pulmonary Embolism
Early View Review Diagnosis of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism Fredrikus A. Klok, Francis Couturaud, Marion Delcroix, Marc Humbert Please cite this article as: Klok FA, Couturaud F, Delcroix M, et al. Diagnosis of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Eur Respir J 2020; in press (https://doi.org/10.1183/13993003.00189-2020). This manuscript has recently been accepted for publication in the European Respiratory Journal. It is published here in its accepted form prior to copyediting and typesetting by our production team. After these production processes are complete and the authors have approved the resulting proofs, the article will move to the latest issue of the ERJ online. Copyright ©ERS 2020 Diagnosis of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism Fredrikus A. Klok, Francis Couturaud F2, Marion Delcroix M3, Marc Humbert4-6 1 Department of Thrombosis and Hemostasis, Leiden University Medical Center, Leiden, The Netherlands 2 Département de Médecine Interne et Pneumologie, Centre Hospitalo-Universitaire de Brest, Univ Brest, EA 3878, CIC INSERM1412, Brest, France 3 Department of Respiratory Diseases, University Hospitals and Respiratory Division, Department of Chronic Diseases, Metabolism & Aging, KU Leuven – University of Leuven, Leuven, Belgium 4 Université Paris-Saclay, Faculté de Médecine, Le Kremlin-Bicêtre, France 5 Service de Pneumologie et Soins Intensifs Respiratoires, Hôpital Bicêtre, AP-HP, Le Kremlin-Bicêtre, France 6 INSERM UMR S 999, Hôpital Marie Lannelongue, Le Plessis Robinson, France Corresponding author: Frederikus A. Klok, MD, FESC; Department of Thrombosis and Hemostasis, Leiden University Medical Center, Leiden, the Netherlands; Albinusdreef 2, 2300RC, Leiden, the Netherlands; Phone: +31- 715269111; E-mail: [email protected] Abstract Chronic thromboembolic pulmonary hypertension (CTEPH) is the most severe long-term complication of acute pulmonary embolism (PE). -
EXAMPLE Alteplase Thrombolytic Central Changes Noted
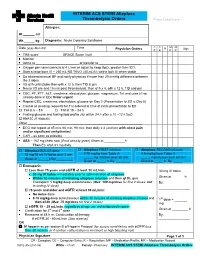
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

Pulmonary Embolism a Pulmonary Embolism Occurs When a Blood Clot Moves Through the Bloodstream and Becomes Lodged in a Blood Vessel in the Lungs
Pulmonary Embolism A pulmonary embolism occurs when a blood clot moves through the bloodstream and becomes lodged in a blood vessel in the lungs. This can make it hard for blood to pass through the lungs to get oxygen. Diagnosing a pulmonary embolism can be difficult because half of patients with a clot in the lungs have no symptoms. Others may experience shortness of breath, chest pain, dizziness, and possibly swelling in the legs. If you have a pulmonary embolism, you need medical treatment right away to prevent a blood clot from blocking blood flow to the lungs and heart. Your doctor can confirm the presence of a pulmonary embolism with CT angiography, or a ventilation perfusion (V/Q) lung scan. Treatment typically includes medications to thin the blood or placement of a filter to prevent the movement of additional blood clots to the lungs. Rarely, drugs are used to dissolve the clot or a catheter-based procedure is done to remove or treat the clot directly. What is a pulmonary embolism? Blood can change from a free flowing fluid to a semi-solid gel (called a blood clot or thrombus) in a process known as coagulation. Coagulation is a normal process and necessary to stop bleeding and retain blood within the body's vessels if they are cut or injured. However, in some situations blood can abnormally clot (called a thrombosis) within the vessels of the body. In a condition called deep vein thrombosis, clots form in the deep veins of the body, usually in the legs. A blood clot that breaks free and travels through a blood vessel is called an embolism. -

Pulmonary Embolism in the First Trimester of Pregnancy
Obstetrics & Gynecology International Journal Case Report Open Access Pulmonary embolism in the first trimester of pregnancy Summary Volume 11 Issue 1 - 2020 Pulmonary embolism in the first trimester of pregnancy without a known medical history Orfanoudaki Irene M is a very rare complication, which if it is misdiagnosed and left untreated leads to sudden Obstetric Gynecology, University of Crete, Greece pregnancy-related death. The sings and symptoms in this trimester are no specific. The causes for pulmonary embolism are multifactorial but in the first trimester of pregnancy, Correspondence: Orfanoudaki Irene M, Obstetric the most important causes are hereditary factors. Many times the pregnant woman ignores Gynecology, University of Crete, Greece, 22 Archiepiskopou her familiar hereditary history and her hemostatic system is progressively activated for the Makariou Str, 71202, Heraklion, Crete, Greece, Tel +30 hemostatic challenge of pregnancy and delivery. The hemostatic changes produce enhance 6945268822, +302810268822, Email coagulation and formation of micro-thrombi or thrombi and prompt diagnosis is crucial to prevent and treat pulmonary embolism saving the lives of a pregnant woman and her fetus. Received: January 19, 2020 | Published: January 28, 2020 Keywords: pregnancy, pulmonary embolism, mortality, diagnosis, risk factors, arterial blood gases, electrocardiogram, ventilation perfusion scan, computed tomography pulmonary angiogram, magnetic resonanance, compression ultrasonography, echocardiogram, D-dimers, troponin, brain -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death -
Protocol-IV-Alteplase.Pdf
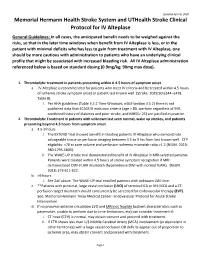
Updated April 6, 2020 Memorial Hermann Health Stroke System and UTHealth Stroke Clinical Protocol for IV Alteplase General Guidelines: In all cases, the anticipated benefit needs to be weighed against the risks, so that in the later time windows when benefit from IV Alteplase is less, or in the patient with minimal deficits who has less to gain from treatment with IV Alteplase, one should be more cautious with administration to patients who have an underlying clinical profile that might be associated with increased bleeding risk. All IV Alteplase administration referenced below is based on standard dosing (0.9mg/kg; 90mg max dose). 1. Thrombolytic treatment in patients presenting within 0-4.5 hours of symptom onset. a. IV Alteplase is recommended for patients who meet IV criteria and be treated within 4.5 hours of ischemic stroke symptom onset or patient last known well. (Stroke. 2019;50:e344–e418. Table 8). i. Per AHA guidelines (Table 3.5.2 Time Windows; e363-Section 3.5.2) there is not published data that ECASS III exclusion criteria (age > 80, warfarin regardless of INR, combined history of diabetes and prior stroke, and NIHSS> 25) are justified in practice. 2. Thrombolytic Treatment in patients with unknown last seen normal, wake up strokes, and patients presenting beyond 4.5 hours from symptom onset. a. 4.5-9 hours i. The EXTEND Trial showed benefit in treating patients IV Alteplase who demonstrate salvageable tissue on perfusion imaging between 4.5 to 9 hrs from last known well. CTP eligibility: <70 cc core volume and perfusion-ischemia mismatch ratio >1.2 (NEJM. -

Acute Pulmonary Embolism in Patients with and Without COVID-19
Journal of Clinical Medicine Article Acute Pulmonary Embolism in Patients with and without COVID-19 Antonin Trimaille 1,2 , Anaïs Curtiaud 1, Kensuke Matsushita 1,2 , Benjamin Marchandot 1 , Jean-Jacques Von Hunolstein 1 , Chisato Sato 1,2, Ian Leonard-Lorant 3, Laurent Sattler 4 , Lelia Grunebaum 4, Mickaël Ohana 3 , Patrick Ohlmann 1 , Laurence Jesel 1,2 and Olivier Morel 1,2,* 1 Division of Cardiovascular Medicine, Nouvel Hôpital Civil, Strasbourg University Hospital, 67000 Strasbourg, France; [email protected] (A.T.); [email protected] (A.C.); [email protected] (K.M.); [email protected] (B.M.); [email protected] (J.-J.V.H.); [email protected] (C.S.); [email protected] (P.O.); [email protected] (L.J.) 2 INSERM (French National Institute of Health and Medical Research), UMR 1260, Regenerative Nanomedicine, FMTS, 67000 Strasbourg, France 3 Radiology Department, Nouvel Hôpital Civil, Strasbourg University Hospital, 67000 Strasbourg, France; [email protected] (I.L.-L.); [email protected] (M.O.) 4 Haematology and Haemostasis Laboratory, Centre for Thrombosis and Haemostasis, Nouvel Hôpital Civil, Strasbourg University Hospital, 67000 Strasbourg, France; [email protected] (L.S.); [email protected] (L.G.) * Correspondence: [email protected] Abstract: Introduction. Acute pulmonary embolism (APE) is a frequent condition in patients with Citation: Trimaille, A.; Curtiaud, A.; COVID-19 and is associated with worse outcomes. Previous studies suggested an immunothrombosis Matsushita, K.; Marchandot, B.; instead of a thrombus embolism, but the precise mechanisms remain unknown.