Status Epilepticus Due to Cerebral Air Embolism After the Valsalva Maneuver CASE REPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Course Description
Instructor: Walter W Lancaster II Off Campus phone: 951-351-1445 x204 Dept phone: NA Cell phone: 951-312-2589 Department of Health and Exercise Science e-mail: [email protected] Spring Quarter, 2016 Alternate e-mail: [email protected] Off Campus Office: La Sierra Academy Office Hours: M-Th 8am – 4pm Consultations by appointment PEAC 106 Scuba Diving Walter Lancaster Location: Health and Exercise Science Classroom 1 (or other assigned instructional locaton) & Pool Tuesdays 6:30pm ~ 9:45pm I. COURSE DESCRIPTION: A. Bulletin Course Description: Course Description Basic SCUBA Diver is an entry-level course for people who have not been previously certified to SCUBA dive, and provides a comprehensive overview of basic concepts that are required to dive safely. Topics include diving equipment, diving physiology, dive planing, environmental considerations, and recognizing and managing risks associated with Open Water diving. Participants who successfully complete the classroom and pool work will qualify for an Open Water certification experience, which must be completed if the student wishes to become a certified diver. Successful completion of the Open Water experience will result in an industry recognized and accepted certification at the level of Basic SCUBA Diver through the National Assocaiton of Underwater Instructors (NAUI). All attendees must be age 16 or older. Students must be able to demonstrate a 10-minute swim/float in water too deep to stand in without the use of swim aids, complete a 200 meter/yard continuous surface swim and demonstrate an underwater (single breath) free dive for a horizontal minimum distance of 25 yards. B. Instructional Materials: Use of the recommended text and Comprehesive Resource Notebook is made available to all students as part of the comprehensive Lab Fee. -
Hyperbaric Oxygen Therapy in Dermatology
MILITARY DERMATOLOGY IN PARTNERSHIP WITH THE ASSOCIATION OF MILITARY DERMATOLOGISTS Hyperbaric Oxygen Therapy in Dermatology Jonathan P. Jeter, MD; Emily B. Wong, MD Overview of HOT PRACTICE POINTS Hyperbaric oxygen therapy involves sitting or lying in a • Hyperbaric oxygen therapy can be considered for special chamber that allows for controlled levels of oxygen the treatment of failing cutaneous grafts and flaps, (O2) at increased atmospheric pressure, which specifically chronic ulcerations caused by vasculitis or autoim- involves breathing near 100% O2 while inside a mono- mune disorders, and vascular compromise, including place or multiplace chamber5 that is pressurized to greater cutaneous ischemia caused by fillers. than sea level pressure (≥1.4 atmosphere absolute).2 • Hyperbaric oxygen therapy involves 1- to 2-hour treat- A monoplace chamber is designed to treat a single ments, 5 days a week, for as long as 1 month. person (Figure 1);copy a multiplace chamber (Figure 2) accom- 5,6 • Hyperbaric oxygen therapy is safe and well-tolerated, modates as many as 5 to 25 patients. The chambers with few contraindications. The sooner therapy is also accommodate hospital beds and medical attendants, started, the greater the potential for benefit. if needed. Hyperbaric O2 is inhaled through a mask, a tight-fitting hood, or an endotracheal tube, depending on notthe patient’s status.7 Treatment ranges from only 1 or Hyperbaric oxygen therapy (HOT) is a potentially useful technique for 2 iterations for acute conditions to 30 sessions or more for certain dermatologic conditions. We review its indications, dermato- chronic conditions. Individual sessions last 45 minutes to logic applications, and potential complications. -
What Chamber Operators Should Know About Ear Barotrauma (And How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018
LEARN.HYPERBARICMEDICINE.COM International ATMO Education What Chamber Operators Should Know About Ear Barotrauma (and How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018 INTRODUCTION Ear barotrauma (i.e. “ear block”, “ear squeeze”) is the most common complication of hyperbaric treatment. It occurs when the pressure in the hyperbaric chamber is greater than the pressure in the middle ear. It is prevented by patient assessment, patient education, and the appropriate actions of the chamber operator. The chamber operator has an important role in preventing ear barotrauma in hyperbaric patients. OBJECTIVES At the conclusion of this article, the reader will be able to: Describe the anatomy of the middle ear Explain the mechanism of ear barotrauma Describe 3 techniques to equalize middle ear pressure ANATOMY OF THE MIDDLE EAR The middle ear is an air space that separates the external ear canal from the inner ear. The eardrum, called the tympanic membrane (TM), vibrates when sound enters the ear canal. The vibration is transmitted to a series of bones in the middle ear. These bones transmit vibration to another membrane (the oval window) that separates the air‐filled middle ear from the fluid‐filled inner ear, where sound is sensed in the cochlea. The nasopharynx is the area behind the nose and above the palate. The Eustachian tubes open into this area. Because of the location of the Eustachian tube openings, the same things that cause nasal congestion (e.g. allergies, upper respiratory infection) can cause swelling around the opening of the Eustachian tubes, making it more difficult to equalize pressure in the middle ear. -

Venous Air Embolism, Result- Retrospective Study of Patients with Venous Or Arterial Ing in Prompt Hemodynamic Improvement
Ⅵ REVIEW ARTICLE David C. Warltier, M.D., Ph.D., Editor Anesthesiology 2007; 106:164–77 Copyright © 2006, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Diagnosis and Treatment of Vascular Air Embolism Marek A. Mirski, M.D., Ph.D.,* Abhijit Vijay Lele, M.D.,† Lunei Fitzsimmons, M.D.,† Thomas J. K. Toung, M.D.‡ exogenously delivered gas) from the operative field or This article has been selected for the Anesthesiology CME Program. After reading the article, go to http://www. other communication with the environment into the asahq.org/journal-cme to take the test and apply for Cate- venous or arterial vasculature, producing systemic ef- gory 1 credit. Complete instructions may be found in the fects. The true incidence of VAE may be never known, CME section at the back of this issue. much depending on the sensitivity of detection methods used during the procedure. In addition, many cases of Vascular air embolism is a potentially life-threatening event VAE are subclinical, resulting in no untoward outcome, that is now encountered routinely in the operating room and and thus go unreported. Historically, VAE is most often other patient care areas. The circumstances under which phy- associated with sitting position craniotomies (posterior sicians and nurses may encounter air embolism are no longer fossa). Although this surgical technique is a high-risk limited to neurosurgical procedures conducted in the “sitting procedure for air embolism, other recently described position” and occur in such diverse areas as the interventional radiology suite or laparoscopic surgical center. Advances in circumstances during both medical and surgical thera- monitoring devices coupled with an understanding of the peutics have further increased concern about this ad- pathophysiology of vascular air embolism will enable the phy- verse event. -

Pulmonary Embolism a Pulmonary Embolism Occurs When a Blood Clot Moves Through the Bloodstream and Becomes Lodged in a Blood Vessel in the Lungs
Pulmonary Embolism A pulmonary embolism occurs when a blood clot moves through the bloodstream and becomes lodged in a blood vessel in the lungs. This can make it hard for blood to pass through the lungs to get oxygen. Diagnosing a pulmonary embolism can be difficult because half of patients with a clot in the lungs have no symptoms. Others may experience shortness of breath, chest pain, dizziness, and possibly swelling in the legs. If you have a pulmonary embolism, you need medical treatment right away to prevent a blood clot from blocking blood flow to the lungs and heart. Your doctor can confirm the presence of a pulmonary embolism with CT angiography, or a ventilation perfusion (V/Q) lung scan. Treatment typically includes medications to thin the blood or placement of a filter to prevent the movement of additional blood clots to the lungs. Rarely, drugs are used to dissolve the clot or a catheter-based procedure is done to remove or treat the clot directly. What is a pulmonary embolism? Blood can change from a free flowing fluid to a semi-solid gel (called a blood clot or thrombus) in a process known as coagulation. Coagulation is a normal process and necessary to stop bleeding and retain blood within the body's vessels if they are cut or injured. However, in some situations blood can abnormally clot (called a thrombosis) within the vessels of the body. In a condition called deep vein thrombosis, clots form in the deep veins of the body, usually in the legs. A blood clot that breaks free and travels through a blood vessel is called an embolism. -

Pulmonary Embolism in the First Trimester of Pregnancy
Obstetrics & Gynecology International Journal Case Report Open Access Pulmonary embolism in the first trimester of pregnancy Summary Volume 11 Issue 1 - 2020 Pulmonary embolism in the first trimester of pregnancy without a known medical history Orfanoudaki Irene M is a very rare complication, which if it is misdiagnosed and left untreated leads to sudden Obstetric Gynecology, University of Crete, Greece pregnancy-related death. The sings and symptoms in this trimester are no specific. The causes for pulmonary embolism are multifactorial but in the first trimester of pregnancy, Correspondence: Orfanoudaki Irene M, Obstetric the most important causes are hereditary factors. Many times the pregnant woman ignores Gynecology, University of Crete, Greece, 22 Archiepiskopou her familiar hereditary history and her hemostatic system is progressively activated for the Makariou Str, 71202, Heraklion, Crete, Greece, Tel +30 hemostatic challenge of pregnancy and delivery. The hemostatic changes produce enhance 6945268822, +302810268822, Email coagulation and formation of micro-thrombi or thrombi and prompt diagnosis is crucial to prevent and treat pulmonary embolism saving the lives of a pregnant woman and her fetus. Received: January 19, 2020 | Published: January 28, 2020 Keywords: pregnancy, pulmonary embolism, mortality, diagnosis, risk factors, arterial blood gases, electrocardiogram, ventilation perfusion scan, computed tomography pulmonary angiogram, magnetic resonanance, compression ultrasonography, echocardiogram, D-dimers, troponin, brain -

Cerebral Air Embolism Following Removal of Central Venous Catheter
MILITARY MEDICINE, 174. 8:878. 2009 Cerebral Air Embolism Following Removal of Central Venous Catheter CPT Joel Brockmeyer, MC USA; CPT Todd Simon. MC USA; MAJ Jason Seery, MC USA; MAJ Eric Johnson, MC USA; COL Peter Armstrong, MC USA ABSTRACT Cerebral air embolism occurs very seldom as a complication of central venous catheterization. We report a 57-year-old female with cerebral air embolism secondary to removal of a central venous catheter (CVC). The patient was trealed with supportive measures and recovered well with minimal long-ienn injury. The preventit)n of airemboli.sm related to central venous catheterization is discussed. INTRODUCTION airway. No loss of pulse or changes in rhythm strip occurred Central venous catheters (CVCs) are used extensively in criti- during code procedures. Following the code and stabilization cally patients. They are cotnnionly placed tor heitiodynamic of the patient's airway, she was transferred to the Surgical iiioniioring. administration of medications, tran.svenous pac- Intensive Care Unit. ing, hemodialysis. and poor peripheral access. Complications Spiral computed tomography (CT) of the chest and com- can occur and are numerous. We describe a case of cerebral air puted tomography of the abdomen and pelvis were undertaken embolism in a ?7-year-old female as a complication ot central with enterai and intravenous contrast. No pulmonary embo- venous catheterization and the treatment course. Additionally, lism or air embolism was visualized on computed tomography we discuss methcxls to prevent air embolism related to central pulmonary angiography (CTPA) and no pathology wiis seen venous catheteri^ation. on CT of the abdomen and pelvis. -

Long-Term Outcome of Iatrogenic Gas Embolism Nicolas Genotelle Cendrine Chabbaut Anne Huon Alexis Tabah Je´Roˆme Aboab Sylvie Chevret Djillali Annane
Intensive Care Med DOI 10.1007/s00134-010-1821-9 ORIGINAL Jacques Bessereau Long-term outcome of iatrogenic gas embolism Nicolas Genotelle Cendrine Chabbaut Anne Huon Alexis Tabah Je´roˆme Aboab Sylvie Chevret Djillali Annane Received: 19 June 2009 Abstract Objective: To establish of 1-year mortality (OR = 4.39, 95% Accepted: 24 January 2010 the incidence and long-term progno- CI 1.46–12.20 and OR = 6.30, 1.71– sis of iatrogenic gas embolism. 23.21, respectively). Among ICU Ó Copyright jointly held by Springer and Methods: This was a prospective survivors, independent predictors of ESICM 2010 inception cohort. We included all 1-year mortality were age consecutive adults with proven iatro- (OR = 1.07, 1.01–1.14), Babinski genic gas embolism admitted to the sign (OR = 6.58, 1.14–38.20) and sole referral academic hyperbaric acute kidney failure (OR = 8.09, center in Paris. Treatment was stan- 1.28–51.21). Focal motor deficits dardized as one hyperbaric session at (OR = 12.78, 3.98–41.09) and 4 ATA for 15 min followed by two Babinski sign (OR = 6.76, 2.24– 45-min plateaus at 2.5 then 2 ATA. 20.33) on ICU admission, and dura- J. Bessereau Á N. Genotelle Á A. Huon Á Inspired fraction of oxygen was set at tion of mechanical ventilation of A. Tabah Á J. Aboab Á D. Annane ()) 100% during the entire dive. Primary 5 days or more (OR = 15.14, General Intensive Care Unit, Hyperbaric endpoint was 1-year mortality. All 2.92–78.52) were independent pre- Centre, Raymond Poincare´ Hospital patients had evaluation by a neurolo- dictors of long-term sequels. -

Pulmonary Embolism
Pulmonary Embolism Pulmonary Embolism (PE) is the blockage of one or more arteries in the lungs, ultimately eliminating the oxygen supply causing heart failure. This can take place when a blood clot from another area of the body, most often from the legs, breaks free, enters the blood stream and gets trapped in the lung's arteries. Once a clot is lodged in the artery of the lung, the tissue is then starved of fuel and may die (pulmonary infarct) or the blockage of blood flow may result in increased strain on the right side of the heart. It is estimated that approximately 600,000 patients suffer from pulmonary embolism each year in the US. Of these 600,000, 1/3 will die as a result. Deep Vein Thrombosis (DVT) is the most common precursor of pulmonary embolism. With early treatment of DVT, patients can reduce their chances of developing a life threatening pulmonary embolism to less than one percent. Early treatment with blood thinners is important to prevent a life-threatening pulmonary embolism, but does not treat the existing clot in the leg. Get more information on Deep Vein Thrombosis. Symptoms of PE Symptoms of pulmonary embolism can include shortness of breath; rapid pulse; sweating; sharp chest pain; bloody sputum (coughing up blood); and fainting. These symptoms are frequently nonspecific to pulmonary embolism and can mimic other cardiopulmonary events. Since pulmonary embolism can be life-threatening, if any of these symptoms are present please see your physician immediately. Treatments for PE Anticoagulation The first line of defense when treating pulmonary embolism is by using an anticoagulant. -

Middle Ear Barotrauma After Hyperbaric Oxygen Therapy - the Role of Insuflation Maneuvers
DOI: 10.5935/0946-5448.20120032 ORIGINAL ARTICLE International Tinnitus Journal. 2012;17(2):180-5. Middle ear barotrauma after hyperbaric oxygen therapy - the role of insuflation maneuvers Marco Antônio Rios Lima1 Luciano Farage2 Maria Cristina Lancia Cury3 Fayez Bahmad Jr.4 Abstract Objective: To analyze the association of insuflation maneuvers status before hyperbaric oxygen therapy with middle ear barotrauma. Materials and Methods: Fouty-one patients (82 ears) admitted to the Department of Hyperbaric Medicine from May 2011 to July 2012. Assessments occurred: before and after the first session, after sessions with symptoms. During the evaluations were performed: otoscopy with Valsalva and Toynbee maneuvers, video otoscopy and specific questionnaire. Middle ear barotrauma was graduated by the modified Edmond’s scale. Tubal insuflation was classified in Good, Median and Bad according to combined results of Valsalva and Toynbee maneuvers. Inclusion criteria: patients evaluated by an otolaryngologist before and after the first session, with no history of ear disease, who agreed to participate in the research (convenience sample). Results: Of the 82 ears included in the study, 32 (39%) had barotrauma after the first session. The rate of middle ear barotrauma according to tubal insuflation was: 17.9% (Good insuflation) 44.4% (Median insuflation) and 55.6% (Bad insuflation)P ( = 0.013). Conclusion: Positive Valsalva and Toynbee maneuvers before the first session, alone or associated were protective factors for middle ear barotrauma by ear after the first session. Keywords: barotrauma, hyperbaric oxygenation, middle ear ventilation. 1 Health Science School - University of Brasília - Brasília - DF - Brasil. E-mail: [email protected] 2 Health Science School - University of Brasília - Brasília - DF - Brasil. -

Hypercoagulability in Hereditary Hemorrhagic Telangiectasia With
Published online: 2019-09-26 Case Report Hypercoagulability in hereditary hemorrhagic telangiectasia with epilepsy Josef Finsterer, Ernst Sehnal1 Departments of Neurological and 1Cardiology and Intensive Care Medicine, General Hospital Rudolfstiftung, Vienna, Austria, Europe ABSTRACT Recent data indicate that in patients with hereditary hemorrhagic teleangiectasia (HHT), low iron levels due to inadequate replacement after hemorrhagic iron losses are associated with elevated factor‑VIII plasma levels and consecutively increased risk of venous thrombo‑embolism. Here, we report a patient with HHT, low iron levels, elevated factor‑VIII, and recurrent venous thrombo‑embolism. A 64‑year‑old multimorbid Serbian gipsy was diagnosed with HHT at age 62 years. He had a history of recurrent epistaxis, teleangiectasias on the lips, renal and pulmonary arterio‑venous malformations, and a family history positive for HHT. He had experienced recurrent venous thrombosis (mesenteric vein thrombosis, portal venous thrombosis, deep venous thrombosis), insufficiently treated with phenprocoumon during 16 months and gastro‑intestinal bleeding. Blood tests revealed sideropenia and elevated plasma levels of coagulation factor‑VIII. His history was positive for diabetes, arterial hypertension, hyperlipidemia, smoking, cerebral abscess, recurrent ischemic stroke, recurrent ileus, peripheral arterial occluding disease, polyneuropathy, mild renal insufficiency, and epilepsy. Following recent findings, hypercoagulability was attributed to the sideropenia‑induced elevation -
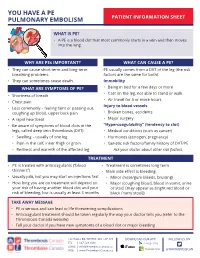
You Have a Pulmonary Embolism (PE)
YOU HAVE A PE PULMONARY EMBOLISM PATIENT INFORMATION SHEET WHAT IS PE? • A PE is a blood clot that most commonly starts in a vein and then moves into the lung. WHY ARE PEs IMPORTANT? WHAT CAN CAUSE A PE? • They can cause short term and long-term PE usually comes from a DVT of the leg (the risk breathing problems. factors are the same for both). • They can sometimes cause death. Immobility WHAT ARE SYMPTOMS OF PE? • Being in bed for a few days or more • Cast on the leg, not able to stand or walk • Shortness of breath • Air travel for 6 or more hours • Chest pain Injury to blood vessels • Less commonly – feeling faint or passing out, coughing up blood, upper back pain • Broken bones, accidents • A rapid heartbeat • Major surgery • Be aware of symptoms of blood clots in the “Hypercoagulability” (tendency to clot) legs, called deep vein thrombosis (DVT): • Medical conditions (such as cancer) • Swelling – usually of one leg • Hormones (estrogen, pregnancy) • Pain in the calf, inner thigh or groin • Genetic risk factors/family history of DVT/PE • Redness and warmth of the affected leg Ask your doctor about other risk factors. TREATMENT • PE is treated with anticoagulants (“blood • Treatment is sometimes long term thinners”) • Main side effect is bleeding: • Usually pills, but you may start on injections first • Minor (nose/gum bleeds, bruising) • How long you are on treatment will depend on • Major (coughing blood, blood in vomit, urine your risk of having another blood clot and your or stool [may appear as bright red blood or risk of bleeding, but is usually at least 3 months black / tarry stool]) TAKE AWAY MESSAGE • PE is serious and can lead to life threatening complications • Anticoagulant treatment should be taken regularly the way your doctor tells you (refer to the Thrombosis Canada website) • Tell your doctor if you have new symptoms of a blood clot or major bleeding 128 HALLS RD, WHITBY, ON, L1P 1Y8 DOWNLOAD OUR APP FOLLOW US ON TEL | 647-528-8586 EMAIL | [email protected] WEB | www.ThrombosisCanada.ca @THROMBOSISCAN.