The Evolutionary Dynamics of Norovirus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hip Hop America Pdf, Epub, Ebook
HIP HOP AMERICA PDF, EPUB, EBOOK Nelson George | 256 pages | 31 May 2005 | Penguin Putnam Inc | 9780143035152 | English | New York, NY, United States Hip HOP America PDF Book Kool Herc -- lay the foundation of the hip-hop movement. Stylistically, southern rap relies on exuberant production and direct lyrics typically about the southern lifestyle, trends, attitudes. Hill's brilliant songwriting flourished from song to song, whether she was grappling with spirituality "Final Hour," "Forgive Them, Father" or stroking sexuality without exploiting it "Nothing Even Matters". According to a TIME magazine article, Wrangler was set to launch a collection called "Wrapid Transit," and Van Doren Rubber was putting out a special version of its Vans wrestling shoe designed especially for breaking [source: Koepp ]. Another key element that's helping spread the hip-hop word is the Internet. Late Edition East Coast. Most hip-hop historians speak of four elements of hip-hop: tagging graffiti , b-boying break dancing , emceeing MCing and rapping. Taking Hip-Hop Seriously. Related Content " ". Regardless, the Bay Area has enjoyed a measurable amount of success with their brainchild. And then, in the mid to late s, there was a resurgence in the popularity of breaking in the United States, and it has stayed within sight ever since. Depending on how old you are, when someone says "hip-hop dance," you could picture the boogaloo, locking, popping, freestyle, uprocking, floor- or downrocking, grinding, the running man, gangsta walking, krumping, the Harlem shake or chicken noodle soup. Another thing to clear up is this: If you think hip-hop and rap are synonymous, you're a little off the mark. -

Hip Hop Dance: Performance, Style, and Competition
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Oregon Scholars' Bank HIP HOP DANCE: PERFORMANCE, STYLE, AND COMPETITION by CHRISTOPHER COLE GORNEY A THESIS Presented to the Department ofDance and the Graduate School ofthe University ofOregon in partial fulfillment ofthe requirements for the degree of Master ofFine Arts June 2009 -------------_._.. _--------_...._- 11 "Hip Hop Dance: Performance, Style, and Competition," a thesis prepared by Christopher Cole Gorney in partial fulfillment ofthe requirements for the Master ofFine Arts degree in the Department ofDance. This thesis has been approved and accepted by: Jenife .ning Committee Date Committee in Charge: Jenifer Craig Ph.D., Chair Steven Chatfield Ph.D. Christian Cherry MM Accepted by: Dean ofthe Graduate School 111 An Abstract ofthe Thesis of Christopher Cole Gorney for the degree of Master ofFine Arts in the Department ofDance to be taken June 2009 Title: HIP HOP DANCE: PERFORMANCE, STYLE, AND COMPETITION Approved: ----- r_---- The purpose ofthis study was to identify and define the essential characteristics ofhip hop dance. Hip hop dance has taken many forms throughout its four decades ofexistence. This research shows that regardless ofthe form there are three prominent characteristics: performance, personal style, and competition. Although it is possible to isolate the study ofeach ofthese characteristics, they are inseparable when defining hip hop dance. There are several genre-specific performance formats in which hip hop dance is experienced. Personal style includes the individuality and creativity that is celebrated in the hip hop dancer. Competition is the inherent driving force that pushes hip hop dancers to extend the form's physical limitations. -

Westminsterresearch Synth Sonics As
WestminsterResearch http://www.westminster.ac.uk/westminsterresearch Synth Sonics as Stylistic Signifiers in Sample-Based Hip-Hop: Synthetic Aesthetics from ‘Old-Skool’ to Trap Exarchos, M. This is an electronic version of a paper presented at the 2nd Annual Synthposium, Melbourne, Australia, 14 November 2016. The WestminsterResearch online digital archive at the University of Westminster aims to make the research output of the University available to a wider audience. Copyright and Moral Rights remain with the authors and/or copyright owners. Whilst further distribution of specific materials from within this archive is forbidden, you may freely distribute the URL of WestminsterResearch: ((http://westminsterresearch.wmin.ac.uk/). In case of abuse or copyright appearing without permission e-mail [email protected] 2nd Annual Synthposium Synthesisers: Meaning though Sonics Synth Sonics as Stylistic Signifiers in Sample-Based Hip-Hop: Synthetic Aesthetics from ‘Old-School’ to Trap Michail Exarchos (a.k.a. Stereo Mike), London College of Music, University of West London Intro-thesis The literature on synthesisers ranges from textbooks on usage and historiogra- phy1 to scholarly analysis of their technological development under musicological and sociotechnical perspectives2. Most of these approaches, in one form or another, ac- knowledge the impact of synthesisers on musical culture, either by celebrating their role in powering avant-garde eras of sonic experimentation and composition, or by mapping the relationship between manufacturing trends and stylistic divergences in popular mu- sic. The availability of affordable, portable and approachable synthesiser designs has been highlighted as a catalyst for their crossover from academic to popular spheres, while a number of authors have dealt with the transition from analogue to digital tech- nologies and their effect on the stylisation of performance and production approaches3. -

Abstracts 1001-1250
305 and contains several ORs, OBPs and IRs. These genes are candidates for this gene encodes a key regulator of secretory function in the Ae. aegypti being involved in the adaptation of An. gambiae to its human host and salivary gland. These studies highlight the need for further analysis of were sequenced in six anopheline species to identify those that show mosquito developmental genetics and may foster comparative studies of evidence of positive selection. salivary gland development in additional vector insect species. 1001 1003 DENGUE 2 INFECTION ALTERS MICRORNA EXPRESSION IN MEDUSA: A NOVEL GENE DRIVE SYSTEM FOR CONFINED AEDES AEGYPTI SUPPRESSION OF MOSQUITO POPULATIONS Corey Campbell, Ann Hess, Gregory D. Ebel John M. Marshall1, Bruce A. Hay2 Colorado State University, Fort Collins, CO, United States 1Imperial College London, London, United Kingdom, 2California Institute of Emerging studies show that important avenues in the post-transcriptional Technology, Pasadena, CA, United States regulation of gene expression occur via small RNA regulatory pathways. Following successful field trials of sterile GM mosquitoes designed to Non-coding RNAs (ncRNAs) are key features of these pathways, and control dengue fever, interest is now growing in the use of gene drive critical molecules involved in their biogenesis and function are conserved systems, such as X-shredders, capable of inducing a population crash as in plants, insects and mammals. To identify products of anti-viral RNA they spread. These systems hold much promise for wide-scale disease interference in vector mosquitoes, deep sequencing small RNA (sRNA) control; however issues arise from their potential to spread across libraries were prepared from DENV2-fed Ae. -

Hyphy Sparked a Social Movement
38876 esr_37 & 38 Sheet No. 28 Side A 07/13/2017 11:07:28 \\jciprod01\productn\E\ESR\37-38\ESR106.txt unknown Seq: 1 19-JUN-17 11:59 HYPHY SPARKED A SOCIAL MOVEMENT Andrea L.S. Moore California State University, Sacramento “When hip hop’s true influence as a cultural movement is finally under- stood. .people will recognize that the very same synergy at the heart of hip hop’s commercial success has also informed our generation’s ac- tivist and political theorists.” —Baraka Kitwana Hyphy (pronounced Hi-fee), is a genre of rap and lifestyle associated with Bay Area hip hop culture that emerged in early 2000 and by 2009 evolved into a counter-cultural social movement for marginalized youth. Hyphy was originally a part of Bay Area vernacular used in local neigh- borhoods as an actual hyperbole on the word hyper. It eventually came to mean an unbridled release of energy that could include excitement, frus- tration or uncontrolled anger. The synergy of anger mixed with raw and aggressive sounds in the musical beats created a powerful reflection of street life and party style rap.1 The aesthetic dimensions of Hyphy in- clude sideshows (car culture), slanguage (language), turfin’ (dancing), fashion, and the independent hustling/marketing of an artist. Each aes- thetic is heavily influenced by the everyday reality one experiences while living in urban spaces. The dynamism of Hyphy is carefree resistance; the sound, in combination with the everyday marginalized lived exper- iences. The Hyphy Movement emerged as a collective for activism as 38876 esr_37 & 38 Sheet No. -

DISCO AS OPERATING SYSTEM, PART ONE Tan Lin
DISCO AS OPERATING SYSTEM, PART ONE Tan Lin When exactly did the era of the medium dissolve? Like most cultural phe- nomena, the dissolution of the medium and its attendant auras—painting, fi lm, music, photography, the novel—is hard to pinpoint. So it’s useful to turn from the PowerPoint lectures of art history, with their virtual-poetic implications, and look for sensory clues on the dance fl oor of the seventies, regarded as an operating system with a mirror ball, two turntables, Quaaludes, and a mixing board. The ad-hoc setup known as “seventies dance culture” or the “Disco Era”—beginning roughly in 1973 and ending in 1979—ushered in a post-medium era for the masses. In disco’s particular case, it led to a host of media formats and musics in the eighties and beyond: house, ambient, electronica, hip-hop, snap, trip-hop, dub, crunk, garage, hyphy, and techno. These mutations suggest how varied and unspecifi c dis- co as a genre became and how complicated its evolution and mainstreaming ultimately was. But then genre or medium was never the right way to think about disco. Asking what disco is is no less diffi cult than asking, What is music? But the question might be better rendered as, What sounds like music in an age of the dissolving medium? And one of the answers to this is “disco,” or, to use a more ambient search parameter, “the disco sound.” The post-medium era had numerous precursors both visual and aural.1 In his notes to the 1914 Box, Marcel Duchamp proposed bypassing the outmoded channel of retinal processing by making a “painting of frequency,”2 a project followed up by Duchamp’s program for “large sculptures in which the listener would be at the center. -
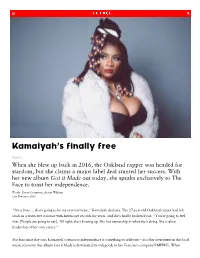
Kamaiyah's Finally Free
Kamaiyah’s finally free Music When she blew up back in 2016, the Oakland rapper was headed for stardom, but she claims a major label deal stunted her success. With her new album Got it Made out today, she speaks exclusively to The Face to toast her independence. Words: Taylor Crumpton, Austin Williams 21st February 2020 “I’m a boss … that’s going to be my new narrative,” Kamaiyah declares. The 27-year-old Oakland rapper had felt stuck in a restrictive contract with Interscope records for years, and she’s finally broken loose. “You’re going to feel that. [People are going to say], ‘All right, she’s bossing up. She has ownership in what she’s doing. She’s taken leadership of her own career.’” For fans since day one, Kamaiyah’s return to independence is something to celebrate – as is her investment in the local music economy (her album Got it Made is distributed by independent San Francisco company EMPIRE). When i h fi b k h h b k i 2016 i h h lf l d i A G d h h Gh Kamaiyah first broke through back in 2016 with her self-released mixtape A Good Night in the Ghetto – spearheaded by the bittersweet anthem How Does it Feel? – she was a breath of fresh air for Oakland, a warm- hearted, unpretentious new artist who had the potential to blow up and was proud to represent her city’s heritage. Known as “The Town”, in the ‘80s and ‘90s, Oakland rappers such as Too $hort, Mistah FAB and Mac Dre rapped about their lived experiences of the region’s pimp culture, impacts of the crack epidemic ushered by President Ronald Reagan’s political agenda, and the loss of close family and friends from the intracommunity violence. -
Week 10, June 3 First, a Bunch of Review, Starting at the End of Lecture 7
Week 10, June 3 First, a bunch of review, starting at the end of lecture 7. "Today": 1. Trap and Drill 2. Fashion 3. Dance 4. Storytelling revisited 5. SD At some point today: Pick one song we've heard, and make a connection to a theme in the history of Hip Hop as we've encountered it. themes like: the dozens, diss tracks, humor, vulgarity, political engagement, relationship to commerce, race, etc. What is the relationship? Why is it interesting? After 2004 • Full scale collapse of the music industry ◦ Napster, suit with RIAA, rise of legal streaming (Spotify) ◦ How did the collapse effect Hip Hop, which had, by now, become the dominant popular form? • Questions about Hip Hop over the last 10 years ◦ Have the demographics of music changed? ◦ What's the relationship, now, between Hip Hop and mainstream culture? ◦ Is the music more politicized now than 10 years ago? Adjustments in the Hip Hop market in the last 10 years • Mixtapes • Shifting relationship to street culture • The internet • Local scenes, local dance • Decline of radio (1996 Telecom Act) • Increased corporate relationships with high fashion, other mass commodidies Mixtapes • Originally, promotional tools for DJs • Became a useful career-building tool for many artists, providing black market revenue, street credibility and exposure • Also a primary venue for experimentation and dispute: a much faster moving medium than official albums, served theole r that live performance might serve in other genres • Relationship between the music business and mixtape scene has always been complicated. • Strictly speaking, they're illegal, but the industry usually turns a blind eye, and even uses them as promotional materials sometimes. -

{PDF} the Legends of Hip-Hop Pdf Free Download
THE LEGENDS OF HIP-HOP PDF, EPUB, EBOOK Justin Bua | 160 pages | 05 Dec 2011 | HarperCollins Publishers Inc | 9780061854972 | English | New York, United States Hip Hop Heads - Own - Thrillist London If you've ever wanted to know where your favorite southern rappers got their game from, if you've ever been curious about the coast-to-coast influence of Bun B and Pimp C, then Ridin' Dirty is for you. It's UGK's most commercially successful album to date it moved over , units and one of the best hip-hop albums ever recorded. It thoroughly captures the essence of the Texas duo through gems like the title track and "One Day" and "Murder. Top Tracks:. The two sides of his personality compete on this album: occasionally vulnerable, occasionally cantankerous. In fact, he pays homage to rap pioneers on "Old School. And you wonder why he's still the most imitated rapper of all time. No other album showcased this amalgamation of jazz, soul, and rap better than Tribe's third album, Midnight Marauders. Essential Tracks. Dre's funky bass lines and heavy synths, coupled with the lyrical showcase from the likes of Snoop and RBX, changed the sound of hip-hop and made The Chronic a household name in the genre. But most importantly, The Chronic was instrumental in the commercialization of gangsta rap by introducing the G-Funk style of hip-hop to the mainstream. Dre's groundbreaking solo debut also served as a podium for bourgeoning west coast rappers including Lady of Rage, Kurupt, Daz, and Snoop Dogg. -

Hybrid Gangs and the Hyphy Movement: Crossing the Color Line in Sacramento County
HYBRID GANGS AND THE HYPHY MOVEMENT: CROSSING THE COLOR LINE IN SACRAMENTO COUNTY Antoinette Noel Wood B.S., California State University, Sacramento, 2008 THESIS Submitted in partial satisfaction of the requirements for the degree of MASTER OF SCIENCE in CRIMINAL JUSTICE at CALIFORNIA STATE UNIVERSITY, SACRAMENTO SPRING 2011 © 2011 Antoinette Noel Wood ALL RIGHTS RESERVED ii HYBRID GANGS AND THE HYPHY MOVEMENT: CROSSING THE COLOR LINE IN SACRAMENTO COUNTY A Thesis by Antoinette Noel Wood Approved by: __________________________________, Committee Chair Dimitri Bogazianos, Ph.D. __________________________________, Second Reader Dan Okada, Ph.D. ____________________________ Date iii Student: Antoinette Noel Wood I certify that this student has met the requirements for format contained in the University format manual, and that this thesis is suitable for shelving in the Library and credit is to be awarded for the thesis. __________________________, Graduate Coordinator ________________ Yvette Farmer, Ph.D. Date Division of Criminal Justice [Thesis Abstract Form] iv [Every thesis or project mustracts for some creative works such as in art or creative writing may vary somewhat, check with your Dept. Advisor.] Abstract of HYBRID GANGS AND THE HYPHY MOVMENT: CROSSING THE COLOR LINE IN SACRAMENTO COUNTY by Antoinette Noel Wood [Use of the next optional as long as te content is supplied.]three headings is Statement of Problem Crips and Bloods-traditional gangs whose mere names conjure up fearful images of violence and destruction-are no longer at the forefront of the gang reality in Sacramento. Instead, influenced by the Bay Area-based rap music subculture of Hyphy, gangs calling themselves "Families," "Mobbs," and "Camps" are believed to be creating a new, hybridized gang culture. -

Journal of Hip Hop Studies
et al.: Journal of Hip Hop Studies June 2016 Published by VCU Scholars Compass, 2016 1 Journal of Hip Hop Studies, Vol. 3 [2016], Iss. 1, Art. 1 Editor in Chief: Daniel White Hodge, North Park University Senior Editorial Advisory Board: Anthony Pinn, Rice University James Paterson, Lehigh University Book Review Editor: Gabriel B. Tait, Arkansas State University Associate Editors: Cassandra Chaney, Louisiana State University Jeffrey L. Coleman, St. Mary’s College of Maryland Monica Miller, Lehigh University Associate & Copy Editor: Travis Harris, PhD Student, College of William and Mary Editorial Board: Dr. Rachelle Ankney, North Park University Dr. Jason J. Campbell, Nova Southeastern University Dr. Jim Dekker, Cornerstone University Ms. Martha Diaz, New York University Mr. Earle Fisher, Rhodes College/Abyssinian Baptist Church, United States Dr. Daymond Glenn, Warner Pacific College Dr. Deshonna Collier-Goubil, Biola University Dr. Kamasi Hill, Interdenominational Theological Center Dr. Andre E. Johnson, University of Memphis Dr. David Leonard, Washington State University Dr. Terry Lindsay, North Park University Ms. Velda Love, North Park University Dr. Anthony J. Nocella II, Hamline University Dr. Priya Parmar, SUNY Brooklyn, New York Dr. Soong-Chan Rah, North Park University Dr. Rupert Simms, North Park University Dr. Darron Smith, University of Tennessee Health Science Center Dr. Jules Thompson, University Minnesota, Twin Cities Dr. Mary Trujillo, North Park University Dr. Edgar Tyson, Fordham University Dr. Ebony A. Utley, California State University Long Beach, United States Dr. Don C. Sawyer III, Quinnipiac University https://scholarscompass.vcu.edu/jhhs/vol3/iss1/1 2 et al.: Journal of Hip Hop Studies . Sponsored By: North Park Universities Center for Youth Ministry Studies (http://www.northpark.edu/Centers/Center-for-Youth-Ministry-Studies) Save The Kids Foundation (http://savethekidsgroup.org/) Published by VCU Scholars Compass, 2016 3 Journal of Hip Hop Studies, Vol. -

The Politics of the Cipher: Hip-Hop, Antiphony and Multiculturalism Bharath Ganesh University College London
The politics of the cipher: hip-hop, antiphony and multiculturalism Bharath Ganesh University College London (UCL) Department of Geography Thesis submitted for the degree of Doctor of Philosophy September 2016 I, Bharath Ganesh, confirm that work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. Abstract This project explores the incipient forms of multiculture present in the musical publics assembled by hip-hop music and culture based on ethnography of a university student group, S4HH (Students for Hip-hop). I position the cipher (a circle of people rapping together) as the diagram of the ethics and politics of hip-hop listening. The primary aesthetic feature of the cipher is antiphony or call-and-response musicality. However, affect in hip-hop musical publics goes beyond aesthetics; it catalyses ethical and political responses. My methods add detail on the varied socialites of listening to the literature on hip-hop studies. I develop antiphony as a unique event that shatters identity and cultivates ethical subjectivities that are constituted in cycles of affect and response between self and other. This argument is based on writings on antiphony from Wole Soyinka, Toni Morrison, Henry Louis Gates Jr., and Paul Gilroy. This work helps operationalise the concepts ‘event’, ‘self’, ‘other’, ‘body’, and ‘community’ in the work of Emmanuel Levinas, Gilles Deleuze, and Jean-Luc Nancy for mapping the ethics and politics of antiphony in hip-hop listening. My study of antiphonal relations illuminates the ethics and politics of bodily response to the material distribution and circulation of affect in hip-hop spaces.