December 2020 ISSN 1080-6040
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evolutionary Relationships and Systematics of the Alphaviruses ANN M
JOURNAL OF VIROLOGY, Nov. 2001, p. 10118–10131 Vol. 75, No. 21 0022-538X/01/$04.00ϩ0 DOI: 10.1128/JVI.75.21.10118–10131.2001 Copyright © 2001, American Society for Microbiology. All Rights Reserved. Evolutionary Relationships and Systematics of the Alphaviruses ANN M. POWERS,1,2† AARON C. BRAULT,1† YUKIO SHIRAKO,3‡ ELLEN G. STRAUSS,3 1 3 1 WENLI KANG, JAMES H. STRAUSS, AND SCOTT C. WEAVER * Department of Pathology and Center for Tropical Diseases, University of Texas Medical Branch, Galveston, Texas 77555-06091; Division of Vector-Borne Infectious Diseases, Centers for Disease Control and Prevention, Fort Collins, Colorado2; and Division of Biology, California Institute of Technology, Pasadena, California 911253 Received 1 May 2001/Accepted 8 August 2001 Partial E1 envelope glycoprotein gene sequences and complete structural polyprotein sequences were used to compare divergence and construct phylogenetic trees for the genus Alphavirus. Tree topologies indicated that the mosquito-borne alphaviruses could have arisen in either the Old or the New World, with at least two transoceanic introductions to account for their current distribution. The time frame for alphavirus diversifi- cation could not be estimated because maximum-likelihood analyses indicated that the nucleotide substitution rate varies considerably across sites within the genome. While most trees showed evolutionary relationships consistent with current antigenic complexes and species, several changes to the current classification are proposed. The recently identified fish alphaviruses salmon pancreas disease virus and sleeping disease virus appear to be variants or subtypes of a new alphavirus species. Southern elephant seal virus is also a new alphavirus distantly related to all of the others analyzed. -
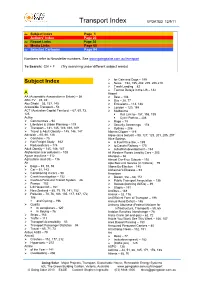
Transport Index UPDATED 12/9/11
Transport Index UPDATED 12/9/11 [ Subject Index Page 1 [ Authors’ Index Page 23 [ Report Links Page 30 [ Media Links Page 60 [ Selected Cartoons Page 94 Numbers refer to Newsletter numbers. See www.goingsolar.com.au/transport To Search: Ctrl + F (Try searching under different subject words) ¾ for Cats and Dogs – 199 Subject Index ¾ News – 192, 195, 202, 205, 206,210 ¾ Trash Landing – 82 ¾ Tarmac Delays in the US – 142 A Airport AA (Automobile Association in Britain) – 56 ¾ Best – 108 ABC-TV – 45, 49 ¾ Bus – 28, 77 Abu Dhabi – 53, 137, 145 ¾ Emissions – 113, 188 Accessible Transport – 53 ¾ London – 120, 188 ACT (Australian Capital Territory) – 67, 69, 73, ¾ Melbourne 125 Rail Link to– 157, 198, 199 Active Cycle Path to – 206 ¾ Communities – 94 ¾ Rage – 79 ¾ Lifestyles & Urban Planning – 119 ¾ Security Screenings – 178 ¾ Transport – 141, 145, 149, 168, 169 ¾ Sydney – 206 ¾ Travel & Adult Obesity – 145, 146, 147 Alberta Clipper – 119 Adelaide – 65, 66, 126 Algae (as a biofuel) – 98, 127, 129, 201, 205, 207 ¾ Carshare – 75 Alice Springs ¾ Rail Freight Study – 162 ¾ A Fuel Price like, – 199 ¾ Reduced cars – 174 ¾ to Darwin Railway – 170 Adult Obesity – 145, 146, 147 ¾ suburban development – 163 Afghanistan (car pollution) – 108 All Western Roads Lead to Cars – 203 Agave tequilana – 112 Allergies – 66 Agriculture (and Oil) – 116 Almost Car-Free Suburb – 192 Air Alps Bus Link Service (in Victoria) – 79 ¾ Bags – 89, 91, 93 Altona By-Election – 145 ¾ Car – 51, 143 Alzheimer’s Disease – 93 ¾ Conditioning in cars – 90 American ¾ Crash Investigation -

June 11, 2021 the Honorable Xavier Becerra Secretary Department of Health and Human Services 200 Independence Ave S.W. Washingto
June 11, 2021 The Honorable Xavier Becerra Secretary Department of Health and Human Services 200 Independence Ave S.W. Washington, D.C. 20201 The Honorable Francis Collins, M.D., Ph.D. Director National Institutes of Health 9000 Rockville Pike Rockville, MD 20892 Dear Secretary Becerra and Director Collins, Pursuant to 5 U.S.C. § 2954 we, as members of the United States Senate Committee on Homeland Security and Governmental Affairs, write to request documents regarding the National Institutes of Health’s (NIH) handling of the COVID-19 pandemic. The recent release of approximately 4,000 pages of NIH email communications and other documents from early 2020 has raised serious questions about NIH’s handling of COVID-19. Between June 1and June 4, 2021, the news media and public interest groups released approximately 4,000 pages of NIH emails and other documents these organizations received pursuant to Freedom of Information Act requests.1 These documents, though heavily redacted, have shed new light on NIH’s awareness of the virus’ origins in the early stages of the COVID- 19 pandemic. In a January 9, 2020 email, Dr. David Morens, Senior Scientific Advisor to Dr. Fauci, emailed Dr. Peter Daszak, President of EcoHealth Alliance, asking for “any inside info on this new coronavirus that isn’t yet in the public domain[.]”2 In a January 27, 2020 reply, Dr. Daszak emailed Dr. Morens, with the subject line: “Wuhan novel coronavirus – NIAID’s role in bat-origin Covs” and stated: 1 See Damian Paletta and Yasmeen Abutaleb, Anthony Fauci’s pandemic emails: -

South Korean National Identity on the Screen in 'Descendants of the Sun'
Volume 16 | Issue 11 | Number 3 | Article ID 5151 | Jun 01, 2018 The Asia-Pacific Journal | Japan Focus No Country for Blue Helmets: South Korean National Identity on the Screen in 'Descendants of the Sun' Patrick Flamm Summary However, the most interesting aspect of DotS is that the protagonists are deployed as This paper provides a contextualized reading of peacekeepers and medical volunteers to a the South Korean 2016 hit drama ‘Descendants fictional and distant post-war country. The of the Sun’, the most prominent pop cultural drama is thus noteworthy as the first major manifestation of the Republic of Korea’s rising Korean drama to prominently feature status as a global middle power. Through peacekeeping operations (PKO) and South linking the fictional peacekeeping mission to a Korea as a global foreign policy actor in a confidently nationalist conception of South distant land. Because of the drama’s great Korean identity, the drama normalizes troop success in Korea and other parts of East Asia, deployments by circumventing traditional and its immediate entry into political discourse narratives for legitimation. This argument rests as illustrated by Park’s comment, a closer look on observations concerning the omission of any at this pop cultural artefact is warranted. In historical and UN context for the deployment, this article, I follow an increasing body of the Othering of the United States as main critical research in the field of International antagonist, and the unchallenged sense of Relations on the link between world politics righteousness and morality displayed by the and popular culture2 in the wake of the so- main protagonists in an otherwise passive local called “aesthetic turn”, where popular texts are setting. -

Hip Hop America Pdf, Epub, Ebook
HIP HOP AMERICA PDF, EPUB, EBOOK Nelson George | 256 pages | 31 May 2005 | Penguin Putnam Inc | 9780143035152 | English | New York, NY, United States Hip HOP America PDF Book Kool Herc -- lay the foundation of the hip-hop movement. Stylistically, southern rap relies on exuberant production and direct lyrics typically about the southern lifestyle, trends, attitudes. Hill's brilliant songwriting flourished from song to song, whether she was grappling with spirituality "Final Hour," "Forgive Them, Father" or stroking sexuality without exploiting it "Nothing Even Matters". According to a TIME magazine article, Wrangler was set to launch a collection called "Wrapid Transit," and Van Doren Rubber was putting out a special version of its Vans wrestling shoe designed especially for breaking [source: Koepp ]. Another key element that's helping spread the hip-hop word is the Internet. Late Edition East Coast. Most hip-hop historians speak of four elements of hip-hop: tagging graffiti , b-boying break dancing , emceeing MCing and rapping. Taking Hip-Hop Seriously. Related Content " ". Regardless, the Bay Area has enjoyed a measurable amount of success with their brainchild. And then, in the mid to late s, there was a resurgence in the popularity of breaking in the United States, and it has stayed within sight ever since. Depending on how old you are, when someone says "hip-hop dance," you could picture the boogaloo, locking, popping, freestyle, uprocking, floor- or downrocking, grinding, the running man, gangsta walking, krumping, the Harlem shake or chicken noodle soup. Another thing to clear up is this: If you think hip-hop and rap are synonymous, you're a little off the mark. -
BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
BMJ Open: first published as 10.1136/bmjopen-2021-050346 on 22 April 2021. Downloaded from BMJ Open is committed to open peer review. As part of this commitment we make the peer review history of every article we publish publicly available. When an article is published we post the peer reviewers’ comments and the authors’ responses online. We also post the versions of the paper that were used during peer review. These are the versions that the peer review comments apply to. The versions of the paper that follow are the versions that were submitted during the peer review process. They are not the versions of record or the final published versions. They should not be cited or distributed as the published version of this manuscript. BMJ Open is an open access journal and the full, final, typeset and author-corrected version of record of the manuscript is available on our site with no access controls, subscription charges or pay-per-view fees (http://bmjopen.bmj.com). If you have any questions on BMJ Open’s open peer review process please email [email protected] http://bmjopen.bmj.com/ on September 29, 2021 by guest. Protected copyright. BMJ Open BMJ Open: first published as 10.1136/bmjopen-2021-050346 on 22 April 2021. Downloaded from Impact of the Tier system on SARS-CoV-2 transmission in the UK between the first and second national lockdowns Journal: BMJ Open ManuscriptFor ID peerbmjopen-2021-050346 review only Article Type: Original research Date Submitted by the 17-Feb-2021 Author: Complete List of Authors: Laydon, Daniel; Imperial -

Diapositiva 1
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Diposit Digital de Documents de la UAB Annabel García León, Faculty of Biosciences, Microbiology degree Universitat Autònoma de Barcelona, 2013 EMERGING ARBOVIRAL DISEASES GLOBAL WARMING In the past 50 years, many vector-borne diseases have The accumulation of greenhouse gases (GHG) in the atmosphere by human activity altered emerged. Some of these diseases are produced for exotic the balance of radiation of the atmosphere, altering the TEMPERATURE at the Earth's surface pathogens that have been introduced into new regions and [1]. others are endemic species that have increased in incidence or have started to infect the human populations for first time Growth human Some longwaves ↑ Air Temperature (new pathogens). population Accumulation of radiation from the Near Surface Many of these vector-borne diseases are caused by greenhouse gases sun are absorbed ↑ Specific Humidity arbovirus. Arboviruses are virus transmitted by arthropods in the atmosphere and re-emitted to ↑ Ocean Heat Content vectors, such mosquitoes, ticks or sanflys. The virus is usually (burn fuels in the Earth by GHG ↑ Sea Level electricity generation, transmitted to the vector by a blood meal, after replicates in Increased per molecules ↑ Sea-Surface transport, industry, capita Temperature the vector salivary glands, where it will be transmitted to a agriculture and land consumption other animal upon feeding. Thus, the virus is amplified by use change, use of ↑ Temperature over of resources fluorinated gases in the oceans the vector and without it, the arbovirus can’t spread. (water, energy, industry) ↑ Temperature over In 1991, Robert Shope, presented the hypothesis that material, land, the land global warming might result in a worldwide increase of biodiversity) ↓ Snow Cover zoonotic infectious diseases. -

MARSEILLE Name Surname H-Index Hindex 10 Years Total Publications
MARSEILLE Name Surname h-index hindex 10 years Total publications RAOULT Didier 77 55 1361 MALISSEN Bernard 62 31 277 VIVIER Eric 51 39 175 CAMBILLAU Christian 49 32 221 OLIVE Daniel 49 25 338 FOURNIER Pierre Edouard 42 38 248 HENRISSAT Bernard 38 36 129 DRANCOURT Michel 37 27 229 GORVEL Jean Pierre 37 23 141 TRAPE Jean François 37 20 162 BOURNE Yves 35 8 88 BROUQUI Philippe 33 22 236 CHIMINI Giovanna 33 22 91 LA SCOLA Bernard 31 27 134 MEGE Jean Louis 31 21 180 MOATTI Jean Paul 30 24 295 de LAMBALLERIE Xavier 29 27 168 PONTAROTTI Pierre 29 13 92 CANARD Bruno 28 28 129 de MICCO Philippe 28 20 226 TAMALET Catherine 28 16 191 BLIN Olivier 27 8 198 PAPAZIAN Laurent 27 17 136 CHARREL Remi 22 19 97 FENOLLAR Florence 22 21 99 PAROLA Philippe 22 21 173 ROLAIN Jean Marc 22 21 164 STEIN Andreas 22 11 53 EWBANK Jonathan 20 20 46 PARZY Daniel 20 16 100 ROGIER Christophe 20 18 130 BIAGINI Philippe 19 15 59 OBADIA Yolande 18 14 92 DAVOUST Bernard 15 15 81 GHIGO Eric 14 13 26 DALOD Marc 13 12 30 PIERRE Philippe 13 13 25 SIMON Fabrice 9 7 38 LESCAR Julien 6 6 11 DESNUES Christelle 5 5 12 SIGNOLI Michel 5 5 23 NICE Nom Prénom hindex total hindex 10ans Total publications DELLAMONICA Pierre 27 17 395 HOFMAN Paul 23 12 249 BARBRY Pascal 21 12 57 GLAICHENHAUS Nicolas 21 16 45 LEMICHEZ Emmanuel 16 11 43 MARSEILLE Scientific and Research Activities Short CV from the main investigators of the project with a h-index equal or higher to 20 Last 5 years period Summary of research activities Name: Raoult Surname: Didier Birth date: 1952 Email: [email protected] Affiliation: URMITE, UMR 6236, IRD-198, Marseille Position PU-PH, (MD, PhD, Professor) Scientific Activities PhD training: 38 International lectures for 5 years: 160 Editorial activities: Editor in chief Clinical Microbiology and Infection, Associated Editor Emerging Infectious Diseases, PloS Neglected tropical Diseases, Eur. -

A Delicate Balance
A Delicate Balance A Delicate Balance An effective government policy countering the COVID-19 pandemic relies on scientific advice. Still, there is a fine line to be tread to make the relationship between politics and science work well. Transparency is one key factor. By Christian Schwägerl n recent years, a phrase became popular among pathological narcissism led him to envy Fauci’s top American scientists: “When the going gets popularity among an anxious population, who Itough, go get Fauci.” The 79-year-old immunol- admired their new “explainer-in-chief.” Some peo- ogist was a kind of secret scientific weapon when ple even took to wearing t-shirts with Fauci’s face it came to dealing with politicians, and indeed the on them. It also became clear that Fauci wanted to public. Anthony Fauci is head of the NIAID, the Na- prioritize public health over short-term economic tional Institute of Allergy and Infectious Diseases. considerations, a policy Trump regarded as very Famous for his research but with no star persona, dangerous…to his re-election prospects. he can clearly explain complex scientific subjects, Dr. Fauci began to publicly express frustration sketch out their practical implications, and explain with a president who seemed quite unwilling to the consequences for politics and everyday life. learn, and who paid no heed to scientific facts, This is how, early in 2020, Dr. Fauci became the publicly recommending the drinking of bleach and public face of American science. With the corona- expressing faith in non-existent light therapies. “I virus spreading across the United States, President can’t jump in front of the microphone and push him Donald Trump eventually recognized the illness as down!” Fauci told Science magazine in March 2020. -

Report 29: the Impact of the COVID-19 Epidemic on All-Cause Attendances to Emergency Departments in Two Large London Hospitals: an Observational Study
1 July 2020 Imperial College COVID-19 response team Report 29: The impact of the COVID-19 epidemic on all-cause attendances to emergency departments in two large London hospitals: an observational study Michaela A C Vollmer, Sreejith Radhakrishnan, Mara D Kont, Seth Flaxman, Sam Bhatt, Ceire Costelloe, Kate Honeyford, Paul Aylin, Graham Cooke, Julian Redhead, Alison Sanders, Peter J White, Neil Ferguson, Katharina Hauck, Shevanthi Nayagam, Pablo N Perez-Guzman WHO Collaborating Centre for Infectious Disease Modelling MRC Centre for Global Infectious Disease Analysis Abdul Latif Jameel Institute for Disease and Emergency Analytics (J-IDEA) Division of Digestive Diseases, Department of Metabolism Digestion and Reproduction Imperial College London Imperial College Healthcare NHS Trust Imperial College London Department of Primary Care and Public Health Global Digital Health Unit Correspondence: [email protected] SUGGESTED CITATION Michaela A C Vollmer, Sreejith Radhakrishnan, Mara D Kont et al. The impact of the COVID-19 epidemic on all- cause attendances to emergency departments in two large London hospitals: an observational study. Imperial College London (30-05-2020), doi: https://doi.org/10.25561/80295. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License. DOI: https://doi.org/10.25561/80295 Page 1 of 22 1 July 2020 Imperial College COVID-19 response team Summary The health care system in England has been highly affected by the surge in demand due to patients afflicted by COVID-19. Yet the impact of the pandemic on the care seeking behaviour of patients and thus on Emergency department (ED) services is unknown, especially for non-COVID-19 related emergencies. -

Hip Hop Dance: Performance, Style, and Competition
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of Oregon Scholars' Bank HIP HOP DANCE: PERFORMANCE, STYLE, AND COMPETITION by CHRISTOPHER COLE GORNEY A THESIS Presented to the Department ofDance and the Graduate School ofthe University ofOregon in partial fulfillment ofthe requirements for the degree of Master ofFine Arts June 2009 -------------_._.. _--------_...._- 11 "Hip Hop Dance: Performance, Style, and Competition," a thesis prepared by Christopher Cole Gorney in partial fulfillment ofthe requirements for the Master ofFine Arts degree in the Department ofDance. This thesis has been approved and accepted by: Jenife .ning Committee Date Committee in Charge: Jenifer Craig Ph.D., Chair Steven Chatfield Ph.D. Christian Cherry MM Accepted by: Dean ofthe Graduate School 111 An Abstract ofthe Thesis of Christopher Cole Gorney for the degree of Master ofFine Arts in the Department ofDance to be taken June 2009 Title: HIP HOP DANCE: PERFORMANCE, STYLE, AND COMPETITION Approved: ----- r_---- The purpose ofthis study was to identify and define the essential characteristics ofhip hop dance. Hip hop dance has taken many forms throughout its four decades ofexistence. This research shows that regardless ofthe form there are three prominent characteristics: performance, personal style, and competition. Although it is possible to isolate the study ofeach ofthese characteristics, they are inseparable when defining hip hop dance. There are several genre-specific performance formats in which hip hop dance is experienced. Personal style includes the individuality and creativity that is celebrated in the hip hop dancer. Competition is the inherent driving force that pushes hip hop dancers to extend the form's physical limitations. -

A Look Into Bunyavirales Genomes: Functions of Non-Structural (NS) Proteins
viruses Review A Look into Bunyavirales Genomes: Functions of Non-Structural (NS) Proteins Shanna S. Leventhal, Drew Wilson, Heinz Feldmann and David W. Hawman * Laboratory of Virology, Rocky Mountain Laboratories, Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Hamilton, MT 59840, USA; [email protected] (S.S.L.); [email protected] (D.W.); [email protected] (H.F.) * Correspondence: [email protected]; Tel.: +1-406-802-6120 Abstract: In 2016, the Bunyavirales order was established by the International Committee on Taxon- omy of Viruses (ICTV) to incorporate the increasing number of related viruses across 13 viral families. While diverse, four of the families (Peribunyaviridae, Nairoviridae, Hantaviridae, and Phenuiviridae) contain known human pathogens and share a similar tri-segmented, negative-sense RNA genomic organization. In addition to the nucleoprotein and envelope glycoproteins encoded by the small and medium segments, respectively, many of the viruses in these families also encode for non-structural (NS) NSs and NSm proteins. The NSs of Phenuiviridae is the most extensively studied as a host interferon antagonist, functioning through a variety of mechanisms seen throughout the other three families. In addition, functions impacting cellular apoptosis, chromatin organization, and transcrip- tional activities, to name a few, are possessed by NSs across the families. Peribunyaviridae, Nairoviridae, and Phenuiviridae also encode an NSm, although less extensively studied than NSs, that has roles in antagonizing immune responses, promoting viral assembly and infectivity, and even maintenance of infection in host mosquito vectors. Overall, the similar and divergent roles of NS proteins of these Citation: Leventhal, S.S.; Wilson, D.; human pathogenic Bunyavirales are of particular interest in understanding disease progression, viral Feldmann, H.; Hawman, D.W.