Congenital Heart Diseases 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

How to Recognize a Suspected Cardiac Defect in the Neonate
Neonatal Nursing Education Brief: How to Recognize a Suspected Cardiac Defect in the Neonate https://www.seattlechildrens.org/healthcare- professionals/education/continuing-medical-nursing-education/neonatal- nursing-education-briefs/ Cardiac defects are commonly seen and are the leading cause of death in the neonate. Prompt suspicion and recognition of congenital heart defects can improve outcomes. An ECHO is not needed to make a diagnosis. Cardiac defects, congenital heart defects, NICU, cardiac assessment How to Recognize a Suspected Cardiac Defect in the Neonate Purpose and Goal: CNEP # 2092 • Understand the signs of congenital heart defects in the neonate. • Learn to recognize and detect heart defects in the neonate. None of the planners, faculty or content specialists has any conflict of interest or will be presenting any off-label product use. This presentation has no commercial support or sponsorship, nor is it co-sponsored. Requirements for successful completion: • Successfully complete the post-test • Complete the evaluation form Date • December 2018 – December 2020 Learning Objectives • Describe the risk factors for congenital heart defects. • Describe the clinical features of suspected heart defects. • Identify 2 approaches for recognizing congenital heart defects. Introduction • Congenital heart defects may be seen at birth • They are the most common congenital defect • They are the leading cause of neonatal death • Many neonates present with symptoms at birth • Some may present after discharge • Early recognition of CHD -
Congenital Cardiovascular Defects
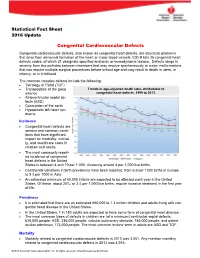
Statistical Fact Sheet 2016 Update Congenital Cardiovascular Defects Congenital cardiovascular defects, also known as congenital heart defects, are structural problems that arise from abnormal formation of the heart or major blood vessels. ICD-9 lists 25 congenital heart defects codes, of which 21 designate specified anatomic or hemodynamic lesions. Defects range in severity from tiny pinholes between chambers that may resolve spontaneously to major malformations that can require multiple surgical procedures before school age and may result in death in utero, in infancy, or in childhood. The common complex defects include the following: Tetralogy of Fallot (TOF) Transposition of the great Trends in age-adjusted death rates attributable to arteries congenital heart defects, 1999 to 2013. Atrioventricular septal de- fects (ASD) Coarctation of the aorta Hypoplastic left heart syn- drome Incidence Congenital heart defects are serious and common condi- tions that have significant impact on morbidity, mortali- ty, and healthcare costs in children and adults. The most commonly report- ed incidence of congenital heart defects in the United States is between 4 and 10 per 1,000, clustering around 8 per 1,000 live births. Continental variations in birth prevalence have been reported, from 6.9 per 1000 births in Europe to 9.3 per 1000 in Asia. An estimated minimum of 40,000 infants are expected to be affected each year in the United States. Of these, about 25%, or 2.4 per 1,000 live births, require invasive treatment in the first year of life. Prevalence It is estimated that there are an estimated 650,000 to 1.3 million children and adults living with con- genital heart disease in the United States. -

Usefulness Ofcontinuous Positive Airway Pressure in Differential
Arch Dis Child: first published as 10.1136/adc.53.6.456 on 1 June 1978. Downloaded from Archives of Disease in Childhood, 1978, 53, 456-460 Usefulness of continuous positive airway pressure in differential diagnosis of cardiac from pulmonary cyanosis in newborn infants P. SYAMASUNDAR RAO, BRENDA L. MARINO, AND ALEX F. ROBERTSON III From the Department of Pediatrics, Sections of Pediatric Cardiology and Neonatology, Medical College of Georgia, Augusta, Georgia, USA SUMMARY Differential diagnosis of cyanosis in the neonate is difficult and cardiac catheterisa- tion may be required for a correct diagnosis. It has been suggested that the response of Pao2 to continuous positive airway pressure (CPAP) with 100% oxygen may be useful. The purpose of this study was to test further this hypothesis by studying all neonates investigated for cyanosis with a Pao2 -50 torr in 0 8 to 1 .0 F1o2. Arterial blood samples were obtained in an F1o2 of 0 21-0 .4 and 0 8-1 .0, and in an F1O2 of 0 8-1 0 with 8-10 cm CPAP, and were analysed for Pao2, Paco2, and pH, bicarbonate being calculated. The final diagnoses were congenital heart disease (CHD) 21 cases, pulmonary parenchymal disease (PD) 10 cases, and persistent fetal circulation (PFC) 3 cases. No significant difference in pH, bicarbonate, or Paco2 was observed among the three groups or with CPAP. In the CHD and PFC infants CPAP produced no significant change in Pao2. In the PD babies Pao2 increased by an average of 33 torr (P<0 05). Despite thus attaining statistical significance 2 PD infants had no increase in Pao2 with CPAP. -

Pharmacy Policy Statement
PHARMACY POLICY STATEMENT Ohio Medicaid DRUG NAME Synagis (palivizumab) BILLING CODE 90378 (1 unit = 1 vial) BENEFIT TYPE Medical SITE OF SERVICE ALLOWED Office/Outpatient Hospital/Home COVERAGE REQUIREMENTS Prior Authorization Required (Preferred Product) QUANTITY LIMIT— 1 vial per month (max 5 during respiratory syncytial virus season) LIST OF DIAGNOSES CONSIDERED NOT Click Here MEDICALLY NECESSARY Synagis (palivizumab) is a preferred product and will only be considered for coverage under the medical/pharmacy benefit when the following criteria are met: Members must be clinically diagnosed with one of the following disease states and meet their individual criteria as stated. PREVENTION OF RESPIRATORY TRACT DISEASE CAUSED BY RESPIRATORY SYNCYTIAL VIRUS (RSV) For initial authorization: 1. Request must be made during the RSV season (November 1st through March 31st) AND initiation of injections should be timed with the onset of laboratory confirmed cases of RSV activity in the community, no earlier than November 1, 2017; AND 2. Member is < 12 months old at the beginning of the RSV season AND meet one of the following criteria (chart notes must be provided to support evidence): a) Member was born < 29 weeks, 0 days’ gestation; b) Member has Chronic Lung Disease (CLD) of prematurity (defined as gestational age <32 weeks, 0 days and a requirement for >21% oxygen for at least the first 28 days after birth); c) Member has hemodynamically significant Congenital Heart Disease (CHD) with one or more of the following: i) Acyanotic heart disease (e.g. atrial septal defect (ASD), ventricular septal defect (VSD), patent ductus arteriosus (PDA), etc.), AND member is receiving medication to control congestive heart failure (CHF) AND will require cardiac surgical procedures; ii) Moderate to severe pulmonary hypertension; iii) Cyanotic heart defect (e.g. -

Congenital Heart Disease Parent FAQ
Congenital Heart Disease Parent FAQ achd.stanfordchildrens.org | achd.stanfordhealthcare.org About Congenital Heart Disease What is congenital heart disease? Congenital heart disease, also called congenital heart defect (CHD), is a heart problem that a baby is born with. When the heart forms in the womb, it develops incorrectly and does not work properly, which changes how the blood flows through the heart. What causes congenital heart defects? In most cases, there is no clear cause. It can be linked to something out of the ordinary happening during gestation, including a viral infection or exposure to environmental factors. Or, it may be linked to a single gene defect or chromosome abnormalities. How common is CHD in the United States among children? Congenital heart defects are the most common birth defects in children in the United States. Approximately 1 in 100 babies are born with a heart defect. What are the most common types of congenital heart defects in children? In general, CHDs disrupt the flow of blood in the heart as it passes to the lungs or to the body. The most common congenital heart defects are abnormalities in the heart valves or a hole between the chambers of the heart (ventricles). Examples include ventricular septal defect (VSD), atrial septal defect (ASD), and bicuspid aortic valve. At the Betty Irene Moore Children’s Heart Center at Stanford Children’s Health, we are known across the nation and world for treating some of the most complex congenital heart defects with outstanding outcomes. Congenital Heart Disease Parent FAQ | 2 Is CHD preventable? In some cases, it could be preventable. -

Review Article Congenital Heart Diseases
KYAMC Journal Vol. 9, No.1, April 2018 Review Article Congenital heart diseases: A review of echocardiogram records Md. Saiful Islam1, Md. Moniruzzaman2 Abstract Congenital heart defect (CHD) means an anatomic malformation of the heart or great vessels which occurs during intrauterine development, irrespective of the age at presentation. They can disrupt the normal blood flow through the heart. The blood flow can slow down, go in the wrong direction or to the wrong place, or be blocked completely. Broadly congenital heart defects can be acyanotic and cyanotic. We have reviewed retrospectively from echocardiogram record nearly two years of period & collected total 404 patients with congenital heart defects. Among them 329 (81.43%) was acyanotic and 75 (18.57%) was cyanotic congenital defects with variety of diagnosis. Ventricular septal defect was the most common acyanotic heart defect and Tetralogy of Fallot was the most common cyanotic heart defect. There was no significant gender deference. Keywords: Acyanotic, Congenital heart disease, Cyanotic. Date of received: 11. 11. 2017 Date of acceptance: 05. 01. 2018 Introduction known. The majority of the defects can be explained by Congenital heart defects (CHD) are reported in almost 1% of multifactorial inheritance hypothesis which states that a live births, and about half of these children need medical or predisposed fetus, when exposed to a given environmental surgical management in infancy1. In the first decade, a further trigger, to which the fetus is sensitive during the critical period 25% require surgery to maintain or improve their life1. Only of cardiac morphogenesis may develop the disease5. A variety 10% survive to adolescence without specific treatment. -

Pulmonary-Atresia-Mapcas-Pavsdmapcas.Pdf
Normal Heart © 2012 The Children’s Heart Clinic NOTES: Children’s Heart Clinic, P.A., 2530 Chicago Avenue S, Ste 500, Minneapolis, MN 55404 West Metro: 612-813-8800 * East Metro: 651-220-8800 * Toll Free: 1-800-938-0301 * Fax: 612-813-8825 Children’s Minnesota, 2525 Chicago Avenue S, Minneapolis, MN 55404 West Metro: 612-813-6000 * East Metro: 651-220-6000 © 2012 The Children’s Heart Clinic Reviewed March 2019 Pulmonary Atresia, Ventricular Septal Defect and Major Aortopulmonary Collateral Arteries (PA/VSD/MAPCAs) Pulmonary atresia (PA), ventricular septal defect (VSD) and major aortopulmonary collateral arteries (MAPCAs) is a rare type of congenital heart defect, also referred to as Tetralogy of Fallot with PA/MAPCAs. Tetralogy of Fallot (TOF) is the most common cyanotic heart defect and occurs in 5-10% of all children with congenital heart disease. The classic description of TOF includes four cardiac abnormalities: overriding aorta, right ventricular hypertrophy (RVH), large perimembranous ventricular septal defect (VSD), and right ventricular outflow tract obstruction (RVOTO). About 20% of patients with TOF have PA at the infundibular or valvar level, which results in severe right ventricular outflow tract obstruction. PA means that the pulmonary valve is closed and not developed. When PA occurs, blood can not flow through the pulmonary arteries to the lungs. Instead, the child is dependent on a patent ductus arteriosus (PDA) or multiple systemic collateral vessels (MAPCAs) to deliver blood to the lungs for oxygenation. These MAPCAs usually arise from the de- scending aorta and subclavian arteries. Commonly, the pulmonary arteries are abnormal, with hypoplastic (small and underdeveloped) central and branch pulmonary arteries and/ or non-confluent central pulmonary arteries. -

Transcatheter Device Closure of Atrial Septal Defect in Dextrocardia with Situs Inversus Totalis
Case Report Nepalese Heart Journal 2019; Vol 16(1), 51-53 Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis Kiran Prasad Acharya1, Chandra Mani Adhikari1, Aarjan Khanal2, Sachin Dhungel1, Amrit Bogati1, Manish Shrestha3, Deewakar Sharma1 1 Department of Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal 2 Department of Internal Medicine, Kathmandu Medical College, Kathmandu,Nepal 3 Department of Pediatric Cardiology, Shahid Gangalal National Heart Centre, Kathmandu, Nepal Corresponding Author: Chandra Mani Adhikari Department of Cardiology Shahid Gangalal National Heart Centre Kathmandu, Nepal Email: [email protected] Cite this article as: Acharya K P, Adhikari C M, Khanal A, et al. Transcatheter device closure of atrial septal defect in dextrocardia with situs inversus totalis. Nepalese Heart Journal 2019; Vol 16(1), 51-53 Received date: 17th February 2019 Accepted date: 16th April 2019 Abstract Only few cases of Device closure of atrial septal defect in dextrocardia with situs inversus totalis has been reported previously. We present a case of a 36 years old male, who had secundum type of atrial septal defect in dextrocardia with situs inversus totalis. ASD device closure was successfully done. However, we encountered few technical difficulties in this case which are discussed in this case review. Keywords: atrial septal defect; dextrocardia; transcatheter device closure, DOI: https://doi.org/10.3126/njh.v16i1.23901 Introduction There are only two case reported of closure of secundum An atrial septal defect (ASD) is an opening in the atrial ASD associated in patients with dextrocardia and situs inversus septum, excluding a patent foramen ovale.1 ASD is a common totalis. -

Track 5: Cardiology and the Imaging Revolution
TRACK 5: CARDIOLOGY AND THE IMAGING REVOLUTION Volume 10 • Number 1 Abstract no: 1 Summer 2013 Real time 3-D echocardiographic characteristics of left ventricle and left atrium in normal children Bao Phung Tran Cong, Nii Masaki, Miyakoshi Chihiro, Yoshimoto Jun, Kato Atsuko, Ibuki Keichiro, Kim Sunghae, Mitsushita Norie, Tanaka Yasuhiko and Ono Yasuo Cardiac Department, Shizuoka Children’s Hospital, Shizuoka, Japan Background: The accurate assessment of left atrial (LA) and/or left ventricular (LV) volume and contractility is crucial for the management of patients with congenital heart disease. The real time 3-dimensional echocardiography (RT3-DE) is reported to show better correlation with magnetic resonance imaging (MRI) in estimating LV and LA volume than conventional 2-dimensional echocardiography (2-DE). On the other hand, the volume measurement in RT3-DE is also reported to be significantly smaller than those in MRI, necessitating the establishment of normal values of RT3-DE itself. Aim: To identify the normal values of LV and LA volume measured by RT3-DE in Japanese children. Methods: Sixty four normal school students (age: median 9.6 years; range (5.5 - 14.5); male 26, female 38) were enrolled in this study. End-diastolic and end- systolic LV and LA volumes were analysed using M-mode in short-axis view, 2-D biplane method, and RT3-DE. We used IE-33 (PHILIPS) with matrix probe X7 and X4. Off-line assessment to calculate LA and LV volume was done using QLAB 8.1 (Philips). Results: Forty nine children (age: median 9.1 years, range (6 - 14); male 21, female 28) had adequate RT3-DE data sets and were analysed. -

Tetralogy of Fallot.” These Podcasts Are Designed to Give Medical Students an Overview of Key Topics in Pediatrics
PedsCases Podcast Scripts This is a text version of a podcast from Pedscases.com on “Tetralogy of Fallot.” These podcasts are designed to give medical students an overview of key topics in pediatrics. The audio versions are accessible on iTunes or at www.pedcases.com/podcasts. Tetralogy of Fallot Developed by Katie Girgulis, Dr. Andrew Mackie, and Dr. Karen Forbes for PedsCases.com. April 14, 2017 Introduction Hello, my name is Katie Girgulis and I am a medical student at the University of Alberta. This podcast was developed with the help of Dr. Andrew Mackie and Dr. Karen Forbes. Dr. Mackie is a pediatric cardiologist at the Stollery Children’s Hospital, and Dr. Forbes is a pediatrician and medical educator at the Stollery Children’s Hospital. This podcast is about the cardiac condition Tetralogy of Fallot (ToF). For teaching on the general approach to pediatric heart murmurs, please check out the ‘Evaluation of a Heart Murmur’ podcast on Pedscases.com. Slide 2 Learning Objectives By the end of this podcast, the learner will be able to: 1) Recognize the clinical presentations of ToF 2) Describe the four anatomical characteristics of ToF 3) Describe the pathophysiology of the murmur in ToF 4) Formulate initial steps when ToF is suspected 5) Delineate the treatment of hypercyanotic episodes 6) Summarize the definitive treatment for ToF Slide 3 Case – Baby Josh Let’s start with a clinical case: You are working with Dr. Smith, a family physician, during your family medicine rotation. Josh is a 4-month-old infant who is here for a well-baby check. -

Clinical Presentations of Critical Cardiac Defects in the Newborn: Decision Making and Initial Management
Review article DOI: 10.3345/kjp.2010.53.6.669 Korean J Pediatr 2010;53(6):669-679 Clinical presentations of critical cardiac defects in the newborn: Decision making and initial management Jae Young Lee, M.D. The risk of mortality and morbidity of patients with congenital heart defects (CHDs) is highest during neonatal period and increases Department of Pediatrics, College of Medicine, the when diagnosis and proper management are delayed. Neonates Catholic University of Korea, Seoul, Korea with critical CHDs may present with severe cyanosis, respiratory distress, shock, or collapse, all of which are also frequent clinical presentations of various respiratory problems or sepsis in the newborn. Early diagnosis and stabilization and timely referral to a tertiary cardiac center are crucial to improve the outcomes in Received: 7 May 2010, Accepted: 17 May 2010 neonates with CHDs. In this review, the clinical presentation of Corresponding author: Jae Young Lee, M.D. critical and potentially life-threatening CHDs is discussed along with Department of Pediatrics, College of Medicine, the Catholic University of Korea, 505, Banpo-dong, Seocho-gu, Seoul 137- brief case reviews to help understand the hemodynamics of these 701, Korea defects and ensure proper decision-making in critically ill patients. Tel: +82-2258-6189, Fax: +82-2-537-4544 E-mail: [email protected] Key Words: Congenital heart defect, Ductal-dependent lesions, Copyright © 2010 by The Korean Pediatric Society Cyanosis, Shock Introduction in these critically ill patients. In this review, clinical presentations of potentially life-threatening CHDs in neonates were discussed Congenital heart defects (CHDs) are the most common birth along with brief case reviews to help pediatricians understand the defects with an incidence of approximately 6-8 in 1,000 live births, hemodynamics of these defects and to facilitate correct decision- accounting for 6-10% of all infant deaths and 20-40% of all infant making in these patients. -

Growth, Development, and Quality of Life in Children with Congenital Heart Disease
Scientific Foundation SPIROSKI, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2020 Aug 20; 8(B):613-618. https://doi.org/10.3889/oamjms.2020.4047 eISSN: 1857-9655 Category: B - Clinical Sciences Section: Cardiology Growth, Development, and Quality of Life in Children with Congenital Heart Disease Sri Maya1*, Eka Gunawijaya2, N. P. Veny Kartika Yantie2, I. G. A. Trisna Windiani2 1Department of Child Health, Sondosia General Hospital, Bima, West Nusa Tenggara, Indonesia; 2Department of Child Health, Faculty of Medicine, Udayana University, Denpasar, Indonesia Abstract Edited by: Sinisa Stojanoski BACKGROUND: Despite the advances in medical and surgical care have improved the survival rates of children Citation: Maya S, Gunawijaya E, Yantie NPVK, Windiani IGAT. Growth, Development, and Quality of Life with congenital heart disease (CHD), they still remain risky for nutritional, cognitive problems, and quality of life. in Children with Congenital Heart Disease. Open Access Those impacts vary according to the severity of heart lesions and still manifested years after surgery. Maced J Med Sci. 2020 Aug 20; 8(B):613-618. https://doi.org/10.3889/oamjms.2020.4047 AIM: The objective of this study was to compare growth, development, and quality of life between cyanotic and Keywords: Congenital heart disease; Cognitive; Quality of life acyanotic CHD. *Correspondence: Sri Maya, Department of Child Health, Sondosia General Hospital, Bima, West Nusa Tenggara, METHODS: The study was performed on 52 patients aged 24–69 months old from June to January 2018 in Sanglah Indonesia. E-mail: [email protected] Pediatric Cardiology clinic used WHO Anthro software, The Mullen Scales of Early Learning and PedsQL Cardiac Received: 11-Nov-2019 Revised: 18-Jul-2020 module.