Imla Latex Agglutination Learning Objectives the Student Will Follow Oral and Written Instructions and Manage Time in the Lab Efficiently
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Streptococci
STREPTOCOCCI Streptococci are Gram-positive, nonmotile, nonsporeforming, catalase-negative cocci that occur in pairs or chains. Older cultures may lose their Gram-positive character. Most streptococci are facultative anaerobes, and some are obligate (strict) anaerobes. Most require enriched media (blood agar). Streptococci are subdivided into groups by antibodies that recognize surface antigens (Fig. 11). These groups may include one or more species. Serologic grouping is based on antigenic differences in cell wall carbohydrates (groups A to V), in cell wall pili-associated protein, and in the polysaccharide capsule in group B streptococci. Rebecca Lancefield developed the serologic classification scheme in 1933. β-hemolytic strains possess group-specific cell wall antigens, most of which are carbohydrates. These antigens can be detected by immunologic assays and have been useful for the rapid identification of some important streptococcal pathogens. The most important groupable streptococci are A, B and D. Among the groupable streptococci, infectious disease (particularly pharyngitis) is caused by group A. Group A streptococci have a hyaluronic acid capsule. Streptococcus pneumoniae (a major cause of human pneumonia) and Streptococcus mutans and other so-called viridans streptococci (among the causes of dental caries) do not possess group antigen. Streptococcus pneumoniae has a polysaccharide capsule that acts as a virulence factor for the organism; more than 90 different serotypes are known, and these types differ in virulence. Fig. 1 Streptococci - clasiffication. Group A streptococci causes: Strep throat - a sore, red throat, sometimes with white spots on the tonsils Scarlet fever - an illness that follows strep throat. It causes a red rash on the body. -

Universidade Do Estado Do Rio De Janeiro Centro Biomédico Faculdade De Ciências Médicas
i Universidade do Estado do Rio de Janeiro Centro Biomédico Faculdade de Ciências Médicas Guilherme da Silva Lourenço Carvalho Formação de biofilme por espécies de Stretptococcus Rio de Janeiro 2012 ii Guilherme da Silva Lourenço Carvalho Formação de biofilme por espécies de Streptococcus Dissertação apresentada, como requisito parcial para obtenção do título de Mestre, ao Programa de Pós-graduação em Microbiologia, da Universidade do Estado do Rio de Janeiro. Área de concentração: Microbiologia Médica Humana. Orientadora: Profa. Dra. Vânia Lúcia Carreira Merquior Coorientadores: Prof. Dr. Rafael Silva Duarte Profa. Dra. Lúcia Teixeira Martins Rio de Janeiro 2012 iii CATALOGAÇÃO NA FONTE UERJ/REDE SIRIUS/BIBLIOTECA CB-A C331 Carvalho, Guilherme da Silva Lourenço. Formação de biofilme por espécies de Streptococcus. / Guilherme da Silva Lourenço Carvalho. - 2012. 79 f. Orientadora: Vânia Lúcia Carreira Merquior. Coorientadores: Rafael Silva Duarte. Lúcia Teixeira Martins. Dissertação (Mestrado) - Universidade do Estado do Rio de Janeiro, Faculdade de Ciências Médicas. Pós-graduação em Microbiologia. 1. Streptococcus. 2. Biofilmes. 3. Virulência. I. Merquior, Vânia Lúcia Carreira II. Duarte, Rafael Silva III. Martins, Lúcia Teixeira. IV. Universidade do Estado do Rio de Janeiro. Faculdade de Ciências Médicas. V. Título. CDU 576.951.214 Bibliotecária: Ana Rachel Fonseca de Oliveira CRB7/6382 Autorizo, apenas para fins acadêmicos e científicos, a reprodução total ou parcial desta dissertação, desde que citada a fonte. ________________________________________ _____________________ Assinatura Data iv Guilherme da Silva Lourenço Carvalho Formação de biofilme porespécies de Streptococcus Dissertação apresentada, como requisito parcial para obtenção do título de Mestre, ao Programa de Pós-graduação em Microbiologia, da Universidade do Estado do Rio de Janeiro. -

157Th Meeting of the National Park System Advisory Board November 4-5, 2015
NORTHEAST REGION Boston National Historical Park 157th Meeting Citizen advisors chartered by Congress to help the National Park Service care for special places saved by the American people so that all may experience our heritage. November 4-5, 2015 • Boston National Historical Park • Boston, Massachusetts Meeting of November 4-5, 2015 FEDERAL REGISTER MEETING NOTICE AGENDA MINUTES Meeting of May 6-7, 2015 REPORT OF THE SCIENCE COMMITTEE NATIONAL PARK SERVICE URBAN AGENDA REPORT ON THE NATIONAL PARK SERVICE COMPREHENSIVE ECONOMIC VALUATION STUDY OVERVIEW OF NATIONAL PARK SERVICE ACTIONS ON ADVISORY BOARD RECOMMENDATIONS • Planning for a Future National Park System • Strengthening NPS Science and Resource Stewardship • Recommending National Natural Landmarks • Recommending National Historic Landmarks • Asian American Pacific Islander, Latino and LGBT Heritage Initiatives • Expanding Collaboration in Education • Encouraging New Philanthropic Partnerships • Developing Leadership and Nurturing Innovation • Supporting the National Park Service Centennial Campaign REPORT OF THE NATIONAL HISTORIC LANDMARKS COMMITTEE PLANNING A BOARD SUMMARY REPORT MEETING SITE—Boston National Historical Park, Commandant’s House, Charlestown Navy Yard, Boston, MA 02139 617-242-5611 LODGING SITE—Hyatt Regency Cambridge, 575 Memorial Drive, Cambridge, MA 62139 617-492-1234 / Fax 617-491-6906 Travel to Boston, Massachusetts, on Tuesday, November 3, 2015 Hotel Check in 4:00 pm Check out 12:00 noon Hotel Restaurant: Zephyr on the Charles / Breakfast 6:30-11:00 am / Lunch 11:00 am - 5:00 pm / Dinner 5-11:00 pm Room Service: Breakfast 6:00 am - 11:00 am / Dinner 5:00 pm - 11:00 pm Wednesday NOVEMBER 4 NOTE—Meeting attire is business. The tour will involve some walking and climbing stairs. -

Biography of Rebecca Craighill Lancefield
NATIONAL ACADEMY OF SCIENCES R E B ECCA CRAIGHILL L ANCEFIELD 1895—1981 A Biographical Memoir by MACLYN MCCARTY Any opinions expressed in this memoir are those of the author(s) and do not necessarily reflect the views of the National Academy of Sciences. Biographical Memoir COPYRIGHT 1987 NATIONAL ACADEMY OF SCIENCES WASHINGTON D.C. REBECCA CRAIGHILL LANCEFIELD January 5, 1895-March 3, 1981 BY MACLYN McCARTY EBECCA CRAIGHILL LANCEFIELD was born on Janu- R ary 5, 1895, in Fort Wadsworth, New York, where her father, Col. William E. Craighill, was stationed as an officer in the U.S. Army Engineer Corps. As a member of an Army family, she lived in many different communities during her early years. After graduating from Wellesley College, how- ever, and spending one year teaching in a girls school in Ver- mont, she returned to New York City. Except for a year's sojourn at the University of Oregon, she spent the remainder of her life there. Her first move toward a career in science apparently came at Wellesley. Stimulated by her roommate's course in zoology, she dropped her notion of majoring in French and English and concentrated her efforts on biology. By the time she graduated in 1916, she was eager to begin graduate training. But she was forced to compromise: funds were short because of the death of her father, and her mother needed her help in supporting her five sisters. She saved enough from her earnings as a teacher during the following year to enable her to accept a scholarship with graduate tuition at Teachers' Col- lege of Columbia University. -
The Professor, the Institute And
ae PROFESSOR, iuees INSTITUTE, maint DNA BY RENE J. DUBOS $14.50 The Professor, the Institute, and DNA BY RENEJ.DUBOS OSWALD THEODOREAVERYislittle knownoutside of the scientific commu- nity. Yet, this extraordinary man, here brought vividly to life by a perceptive friend and sophisticated scientific colleague, was amonumentalforce in the developmentof medical research in the United States. Even amongscientists, Avery is known chiefly as the senior author of a paper published in 1944 that identified DNA as the purveyorof genetic information. Twothings makethis highly personalized biography a landmark volume. First, its technical chaptersclarify the philosophi- cal conceptsthatlie behind today’s understanding of the immunology of -bacterial infection. Second, nota single existing textbook has ever described the laborious methods by which the men in Avery’s laboratory discovered the genetic import of DNA. continued on back flap THE PROFESSOR, THE INSTITUTE, AND DNA OSWALD THEODORE AVERY THE PROFESSOR, THE INSTITUTE, AND DNA BY RENE J. DUBOS THE ROCKEFELLER UNIVERSITY PRESS NEW YORK 1976 .- Copyright© 1976 The Rockefeller University Press Library of Congress Catalogue Card Number 76-26812 ISBN 87470-022-1 Printed in the United States of America Second printing 1978 CONTENTS INTRODUCTION 3 CHAPTER ONE: The Professor and the Institute 5 A dynamic institution Workshops of science The Professor and the genius loci CHAPTER lWO: From the Bedside to the Laboratory 13 The rise of scientific medicine in the United States The Rockefeller Institute -

Oswald Avery and The
Oswald Avery and the Irving Kushner, MD, and David Samols, PhD Dr. Kushner (AΩA, Washington University in St. Louis, time,infectiousdiseaseswerethemajorpublichealthconcern 1954) is professor emeritus of Medicine, and Dr. Samols andbacteriologywasthemostglamorousandpromisingfield is professor of Biochemistry at Case Western Reserve in the nascent biomedical science of the day. Opportunities University School of Medicine. for research at that time were very few, but Avery did find a position at the Hoagland laboratory, a privately-endowed stheyearshavepassed,thetremendouscontributions bacteriologylaboratoryinBrooklyn,whereheworkedforsix ofOswaldT.Avery(1877–1955)tobiomedicalscience years,performinglargelyunimaginativework. arefadingfromourcollectivememory.Amodestand self-effacingA man,Averywasoneoftheoutstandingbiologi- The Rockefeller Institute for Medical Research calscientistsofthefirsthalfofthetwentiethcentury,1feltby Attheendofthenineteenthcentury,JohnD.Rockefeller sometobethemostdeservingscientistnottohavereceived was seeking guidance about how to deploy his philanthro- theNobelPrize.Hislaboratorywasresponsibleforthreeland- pies most effectively. He was the richest man in the world, markcontributions: perhaps the richest man in history. Rockefeller’s principal 1. Thedemonstrationthatpolysaccharidesareantigenic philanthropicadviserwasaBaptistminister,FrederickTaylor 2. The discovery of C-reactive protein (CRP), which Gates,himselfaphysician’sson,whohadnoticedduringhis openedthedoortostudyoftheacutephaseresponse2 ministrythatphysicianswererarelyabletodealwithserious -
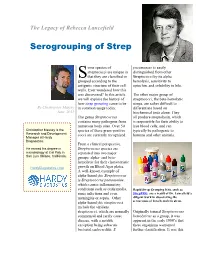
The Legacy of Rebecca Lancefield
The Legacy of Rebecca Lancefield Serogrouping of Strep ome species of pneumoniae is easily streptococci are unique in distinguished from other S that they are classified or Streptococci by its alpha grouped according to the hemolysis, sensitivity to antigenic structure of their cell optochin, and solubility in bile. walls. Ever wondered how this was discovered? In this article The other major group of we will explore the history of streptococci, the beta-hemolytic how strep grouping came to be streps, are rather difficult to By Christopher Massey in common usage today. differentiate based on June, 2015 biochemical tests alone. They The genus Streptococcus all produce streptolysin, which contains many pathogens from is responsible for their ability to numerous body sites. Over 50 lyse blood cells, and can Christopher Massey is the species of these gram-positive typically be pathogenic to Research and Development cocci are currently recognized. humans and other animals. Manager at Hardy Diagnostics. From a clinical perspective, He earned his degree in Streptococcus species are microbiology at Cal Poly in separated into two major San Luis Obispo, California. groups: alpha- and beta- hemolytic for their characteristic HardyDiagnostics.com growth on Blood Agar plates. A well-known example of alpha-hemolytic Streptococcus is Streptococcus pneumoniae, which causes inflammatory conditions such as otitis media, Rapid Strep Grouping Kits, such as sinus infections and even StrepPRO, are a result of Dr. Lancefield’s meningitis or sepsis. Other diligent work in discovering the alpha-hemolytic streptococci serogroups of beta hemolytic strep. include the viridans streptococci, which are normally Originally termed Streptococcus commensal and rarely cause hemolyticus as a group, it was disease, with a notable apparent in the early 1900’s that exception being subacute these organisms warranted bacterial endocarditis. -

The George Wright Forum
national park units A new method for setting preservation priorities Science vs. political interference in system planning What's a name worth? — The Yosemite trademark fight Why public financing is critical to parks Needed: Reliable funding for bison management Countering "ecomodernism" The George Wright Forum The GWS Journal of Parks, Protected Areas & Cultural Sites volume 33 number 1 • 2016 Mission The George Wright Society promotes protected area stewardship by bring ing practitioners together to share their expertise. Our Goal The Society strives to be the premier organization connecting people, plac es, knowledge, and ideas to foster excellence in natural and cultural resource management, research, protection, and interpretation in parks and equivalent reserves. Board of Directors Nathalie Gagnon, President • Ottawa, Ontario Jerry M. Mitchell, Vice President • Littleton, Colorado David J. Parsons, Secretary • Florence, Montana Ryan Sharp, Treasurer • Manhattan, Kansas Zarnaaz Bashir • Ashburn, Virginia David Graber • Three Rivers, California Barrett Kennedy • Baton Rouge, Louisiana Armando Quintero • San Rafael, California Chris Spence • Mill Valley, California Lynn Wilson • Cobble Hill, British Columbia Graduate Student Liaison to the Board Gina Depper • Clemson, South Carolina Executive Office David Harmon, Executive Director/ Co-editor, The George Wright Forum Emily Dekker-Fiala, Conference Coordinator Rebecca Conard, Co-editor, The George Wright Forum P. O. Box 65 • Hancock, Michigan 49930-0065 USA 1-906-487-9722 • [email protected] • www.georgewright.org O 2016 The George Wright Society. All rights reserved (No copyright is claimed for previously published material reprinted herein.) ISSN 0732-4715. Editorial and manuscript submission guidelines may be found at www.georgewright.org/forum. Text paper is made of 50% recycled fi bers. -
!["Mrs. L." : [Dr. Rebecca Lancefield] Judith N](https://docslib.b-cdn.net/cover/0261/mrs-l-dr-rebecca-lancefield-judith-n-5190261.webp)
"Mrs. L." : [Dr. Rebecca Lancefield] Judith N
Rockefeller University Digital Commons @ RU Rockefeller University Research Profiles Campus Publications Summer 1990 "Mrs. L." : [Dr. Rebecca Lancefield] Judith N. Schwartz Follow this and additional works at: http://digitalcommons.rockefeller.edu/research_profiles Part of the Life Sciences Commons Recommended Citation Schwartz, Judith N., ""Mrs. L." : [Dr. Rebecca Lancefield]" (1990). Rockefeller University Research Profiles. Book 35. http://digitalcommons.rockefeller.edu/research_profiles/35 This Article is brought to you for free and open access by the Campus Publications at Digital Commons @ RU. It has been accepted for inclusion in Rockefeller University Research Profiles by an authorized administrator of Digital Commons @ RU. For more information, please contact [email protected]. THE ROCKEFELLER UNIVERSITY RESEARCH PROJFILES Precipitin rack and hand lens used by Dr. Lancefield SUMMER 1990 "Mrs. L." Her laboratory was called "the Scotland Yard ofstrepto coccal mysteries." In it, for more than sixty years, Rebecca Lancefield stalked a devious, multifarious adversary: the streptococcal bacteria. For those with access to modern medical care and antibiotics, a touch of"strep" may not seem a particularly serious threat. In 1918, when Rebecca Lancefield first came to The Rockefeller Institute for Medical Research (later The Rockefeller University), the diseases caused by Rebecca Lancefield, streptococcal infection, among them rheumatic fever, 1895-1981 scarlet fever, and acute nephritis, were common and dangerous ailments. Millions of people, mostly children, developed crippling heart disease in the wake ofrheumatic fever. Millions in Mrica, Asia, and Latin America still do. When she began her research no one knew how many kinds ofstreptococci existed, which ones were dangerous to man, or how they did their damage. -

Streptococcus Laboratory General Methods
The reference used for compiling the methods in Section I is: Murray, P.R., Baron, E. J., Jorgensen, J.J., Pfaller, M.A., and Yolken, R.H. Manual of Clinical Microbiology, 8th ed. ASM Press: Washington, DC, 2003. The Streptococcus species identification methods in Section II were compiled by Dr. Lynn Shewmaker. Also thanks to input from several individuals, including Richard Facklam and Lucia Teixeira. Section I. 1. Accuprobe-Enterococcus Test………….………..4 2. Accuprobe-Pneumococcus Test …………..….….4 3. Acid formation in carbohydrate broth..................5 4. Arginine Hydrolysis……………………….……….6 5. Bacitracin Test……………………………………..7 6. Bile-esculin Test…………………………………...8 7. Bile solubility Test …………………………………9 8. CAMP Test…......................................................10 9. Catalase Test......................................................11 10. Clindamycin test………………………………….12 11. Esculin hydrolysis……………………………….. 13 12. Gas from MRS broth……………………………...14 13. Gram Stain………………………………………...15 14. Growth at 10 & 45C……………………………. 17 15. Hemolysis………………………………………….18 16. Hippurate hydrolysis…………………………… 19 17. Lancefield Group Antigen………………………..20 18. Leucine amino peptidase (LAP)…………………21 19. Litmus Milk Test…………………………………..22 20. Motility………………………………………………23 21. 6.5% NaCl Tolerace Test...................................24 22. Optochin…………………………………………….25 23. Pigmentation....................................................... 26 24. Pyridoxal Requirement Test (Vitamin B6)……….27 25. Pyrrolidonlarylamindase (PYR)............................28 26. -

Streptococcus Agalactiae
Université Pierre et Marie Curie (Paris 6) Ecole Doctorale: Complexité du Vivant Thèse présentée par Alexandre Miguel Santos Almeida pour obtenir le grade de Docteur Evolutionary insights into the host-specific adaptation and pathogenesis of group B Streptococcus Soutenance prévue le 31 mars 2017. Jury composé de: Prof. Philippe Lopez Université Paris VI Président Dr Immaculada Margarit GSK Vaccines Rapporteur Prof. Ivan Matic Université Paris V Rapporteur Dr Christine Citti CNRS, INRA Examinateur Dr Olivier Tenaillon CNRS, IAME, Université Paris VII Examinateur Dr Philippe Glaser Institut Pasteur Directeur de these Université Pierre et Marie Curie (Paris 6) Doctoral School: Complexité du Vivant Thesis presented by Alexandre Miguel Santos Almeida for the degree of Doctoral of Philosophy Evolutionary insights into the host-specific adaptation and pathogenesis of group B Streptococcus Defence planned for March 31, 2017. Jury composition: Prof. Philippe Lopez Université Paris VI President Dr Immaculada Margarit GSK Vaccines Reviewer Prof. Ivan Matic Université Paris V Reviewer Dr Christine Citti CNRS, INRA Examiner Dr Olivier Tenaillon CNRS, IAME, Université Paris VII Examiner Dr Philippe Glaser Institut Pasteur Thesis supervisor “There is grandeur in this view of life, with its several powers, having been originally breathed into a few forms or into one; and that, whilst this planet has gone cycling on according to the fixed law of gravity, from so simple a beginning endless forms most beautiful and most wonderful have been, and are being, evolved.” — Charles Darwin AcknoWledgements The collaborations and relationships developed With so many people during my PhD were crucial for accomplishing this Work. First of all I Would like to thank my supervisor Philippe Glaser for having given me the opportunity to Work in his team and for being an exemplary PhD mentor. -

Essential Microbiology
JWBK011-FM JWBK011-Hogg August 12, 2005 19:44 Char Count= 0 Essential Microbiology i JWBK011-FM JWBK011-Hogg August 12, 2005 19:44 Char Count= 0 ii JWBK011-FM JWBK011-Hogg August 12, 2005 19:44 Char Count= 0 Essential Microbiology Stuart Hogg The University of Glamorgan, UK iii JWBK011-FM JWBK011-Hogg August 12, 2005 19:44 Char Count= 0 Copyright C 2005 John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England Telephone (+44) 1243 779777 Email (for orders and customer service enquiries): [email protected] Visit our Home Page on www.wileyeurope.com or www.wiley.com Reprinted with corrections September 2005 All Rights Reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, scanning or otherwise, except under the terms of the Copyright, Designs and Patents Act 1988 or under the terms of a licence issued by the Copyright Licensing Agency Ltd, 90 Tottenham Court Road, London W1T 4LP, UK, without the permission in writing of the Publisher. Requests to the Publisher should be addressed to the Permissions Department, John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England, or emailed to [email protected], or faxed to (+44) 1243 770620. Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners.