AUR 2017 Research Paper Abstracts
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

THE ROMANCE of BIBLE CHRONOLOGY Rev
THE ROMANCE OF BIBLE CHRONOLOGY Rev. Martin Anstey, BA, MA An Exposition of the Meaning, and a Demonstration of the Truth, of Every Chronological Statement Contained in the Hebrew Text of the Old Testament Marshall Brothers, Ltd., London, Edinburgh and New York 1913. DEDICATION To my dear Friend Rev. G. Campbell Morgan, D.D. to whose inspiring Lectures on “The Divine Library in Human History” I trace the inception of these pages, and whose intimate knowledge and unrivalled exposition of the Written Word makes audible in human ears the Living Voice of the Living God, I dedicate this book. The Author October 3rd, 1913 FOREWORD BY REV. G. CAMPBELL MORGAN, D. D. It is with pleasure, and yet with reluctance, that I have consented to preface this book with any words of mine. The reluctance is due to the fact that the work is so lucidly done, that any setting forth of the method or purpose by way of introduction would be a work of supererogation. The pleasure results from the fact that the book is the outcome of our survey of the Historic move- ment in the redeeming activity of God as seen in the Old Testament, in the Westminster Bible School. While I was giving lectures on that subject, it was my good fortune to have the co—operation of Mr. Mar- tin Anstey, in a series of lectures on these dates. My work was that of sweeping over large areas, and largely ignoring dates. He gave his attention to these, and the result is the present volume, which is in- valuable to the Bible Teacher, on account of its completeness and detailed accuracy. -

The 100 Most Eminent Psychologists of the 20Th Century
Review of General Psychology Copyright 2002 by the Educational Publishing Foundation 2002, Vol. 6, No. 2, 139–152 1089-2680/02/$5.00 DOI: 10.1037//1089-2680.6.2.139 The 100 Most Eminent Psychologists of the 20th Century Steven J. Haggbloom Renee Warnick, Jason E. Warnick, Western Kentucky University Vinessa K. Jones, Gary L. Yarbrough, Tenea M. Russell, Chris M. Borecky, Reagan McGahhey, John L. Powell III, Jamie Beavers, and Emmanuelle Monte Arkansas State University A rank-ordered list was constructed that reports the first 99 of the 100 most eminent psychologists of the 20th century. Eminence was measured by scores on 3 quantitative variables and 3 qualitative variables. The quantitative variables were journal citation frequency, introductory psychology textbook citation frequency, and survey response frequency. The qualitative variables were National Academy of Sciences membership, election as American Psychological Association (APA) president or receipt of the APA Distinguished Scientific Contributions Award, and surname used as an eponym. The qualitative variables were quantified and combined with the other 3 quantitative variables to produce a composite score that was then used to construct a rank-ordered list of the most eminent psychologists of the 20th century. The discipline of psychology underwent a eve of the 21st century, the APA Monitor (“A remarkable transformation during the 20th cen- Century of Psychology,” 1999) published brief tury, a transformation that included a shift away biographical sketches of some of the more em- from the European-influenced philosophical inent contributors to that transformation. Mile- psychology of the late 19th century to the stones such as a new year, a new decade, or, in empirical, research-based, American-dominated this case, a new century seem inevitably to psychology of today (Simonton, 1992). -

Telemedicine Services for Remote Reporting and Dissemination Technology in Sub-Saharan Africa
Theme 2019: International Cooperation as Key Principle in Space Activities Telemedicine services for remote reporting and dissemination technology in Sub-Saharan Africa Silvana Dellepiane - Moira Gerace Telemedicine services for remote reporting and dissemination technology in Sub-Saharan Africa 4. A CASE STUDY: C.A.R. 1. INTRODUCTION • • Substainable Goals Geopolitical vision • WHO Leadership priorities and UHC • Healthcare and conditions of children • The logic ICT context • Hospital of Maïgaro • Culture, Cooperation and Technology • Telemedicine: Needs and requirements 5. DIGITAL DIVIDE and TELEMEDICINE IN AFRICA 2. E-Health • ICT technology Dissemination • Medicine-at-a-distance • Satellite communications • Telemedicine practice 6. TELEMEDICINE: A PILOT STUDY IN C.A.R. • WHO digital health • The approach • Maximising digital health technology AFRO • The Project development Region • The Project architecture • The software development 3. DATA PROTECTION • The platform • Medical records • The experiment on site • GDPR Legal issues 7. CONCLUSIONS Telemedicine services for remote reporting and dissemination technology in Sub-Saharan Africa 1. INTRODUCTION • Substainable Goals • WHO Leadership priorities and UHC • The logic ICT context • Culture, Cooperation and Technology End of 2015: transition from UNITED NATIONS Millennium Development Goals (MDGs) (proposed in the late 90s) to Sustainable Development Goals (SDGs). SDG 3 – Ensure healthy lives and promote well-being for all at all ages As one of the Sustainable Development Goals (SDGs) set by the UN at the September 2015 global summit held in New York, SDG 3 – better health care and general well-being has always been a major challenge, especially in the developing world. Workers in various industries that are supposed to propel economic growth can only maximise their productivity if they are physically well and fit to comfortably handle their jobs’ magnitudes. -

Health IT-Enabled Care Coordination and Redesign in Tennessee
FINAL CONTRACT REPORT Using Health IT in Practice Redesign: Impact of Health IT on Workflow Health IT-Enabled Care Coordination and Redesign in Tennessee Agency for Healthcare Research and Quality Advancing Excellence in Health Care www.ahrq.gov HEALTH IT Final Contract Report Health IT-Enabled Care Coordination and Redesign in Tennessee Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. HHSA 290-2010-00024I Prepared by: RTI International Research Triangle Park, NC Authors: Jonathan S. Wald, M.D., M.P.H., RTI International Laurie L. Novak, Ph.D., M.H.S.A., Vanderbilt University Medical Center (VUMC), Nashville, TN Christopher L. Simpson, M.A., VUMC Jason M. Slagle, Ph.D., VUMC Alison K. Banger, M.P.H., RTI International Neeraja B. Peterson, M.D., M.S., VUMC AHRQ Publication No. 15-0048-EF June 2015 This document is in the public domain and may be used and reprinted without permission except those copyrighted materials that are clearly noted in the document. Further reproduction of those copyrighted materials is prohibited without the specific permission of copyright holders. Suggested Citation: Wald JS, Novak LL, Simpson CL, et al. Health IT-Enabled Care Coordination and Redesign in Tennessee. (Prepared by RTI International, under Contract No. 290-2010-00024I). AHRQ Publication No. 15-0048-EF. Rockville, MD: Agency for Healthcare Research and Quality. June 2015. None of the investigators has any affiliations or financial involvement that conflicts with the material presented in this report. This project was funded by the Agency for Healthcare Research and Quality (AHRQ), U.S. -

Ehealth to Support Cancer Survivors Support to Ehealth Ehealth to Support Cancer Survivors
eHealth to support survivors cancer eHealth to support cancer survivors Development, implementation and evaluation of an interactive portal The end Wilma Kui jpers Wilma Kui jpers eHEALTH TO SUPPORT CANCER SURVIVORS DEVELOPMENT, IMPLEMENTATION AND EVALUATION OF AN INTERACTIVE PORTAL Wilma Kui jpers Address of correspondence Wilma Kuijpers Zamenhof 20 1961 GL Heemskerk, the Netherlands [email protected] +31 (0)6 22 15 77 82 © Copyright 2015: Wilma Kuijpers, the Netherlands All rights reserved. No part of this thesis may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage or retrieval system, without permission in writing from the author, or, when appropriate, from the publishers of the publications. ISBN: 978-90-365-4031-5 Department Health Technology and Services Research, University of Twente, HSS 16-011, ISSN 1878-4968 Cover design and layout: Rachel van Esschoten, DivingDuck Design (www.divingduckdesign.nl) Printing: Gildeprint Drukkerijen, Enschede The studies in this thesis were financially supported by a grant from Alpe d’Huzes (KWF 2010- 4584) The printing of this thesis was supported by The Netherlands Cancer Institute and ChipSoft. eHEALTH TO SUPPORT CANCER SURVIVORS DEVELOPMENT, IMPLEMENTATION AND EVALUATION OF AN INTERACTIVE PORTAL PROEFSCHRIFT ter verkrijging van de graad van doctor aan de Universiteit Twente, op gezag van de rector magnificus, prof. dr. H. Brinksma, volgens besluit van het College voor Promoties in het openbaar te verdedigen op vrijdag 4 maart 2016 om 12.45 uur door Wilma Kuijpers geboren op 7 december 1984 te Beverwijk Dit proefschrift is goedgekeurd door de promotoren: Prof. -

Ordines Militares Conference
ORDINES◆ MILITARES COLLOQUIA TORUNENSIA HISTORICA Yearbook for the Study of the Military Orders vol. XIX (2014) Uniwersytet Mikołaja Kopernika Towarzystwo Naukowe w Toruniu Toruń 2014 Editorial Board Roman Czaja, Editor in Chief, Nicolaus Copernicus University Toruń Jürgen Sarnowsky, Editor in Chief, University of Hamburg Jochen Burgtorf, California State University Sylvain Gouguenheim, École Normale Supérieure Lettres et Sciences Humaines de Lyon Hubert Houben, Università del Salento Lecce Alan V. Murray, University of Leeds Krzysztof Kwiatkowski, Assistant Editor, Nicolaus Copernicus University Toruń Reviewers: Udo Arnold, Rheinische Friedrich-Wilhelms-Universität Bonn (retired) Karl Borchardt, Monumenta Germaniae Historica, München Jochen Burgtorf, Department of History, California State University Wiesław Długokęcki, Institute of History, University of Gdańsk Marie-Luise Favreau-Lilie, Friedrich-Meinecke-Institut, Freie Universität Berlin Alan Forey, Durham University (retired) Mario Glauert, Brandenburgisches Landeshauptarchiv in Potsdam Sylvain Gouguenheim, Ecole Normale Supérieure Lettres et Sciences Humaines de Lyon Dieter Heckmann, Geheimes Staatsarchiv Preußischer Kulturbesitz, Berlin-Dahlem Ilgvars Misāns, Faculty of History and Philosophy, University of Latvia, Riga Maria Starnawska, Institute of History, Jan Długosz University in Częstochowa Sławomir Zonenberg, Institute of History and International Relationships, Kazimierz Wielki University in Bydgoszcz Janusz Tandecki, Institut of History and Archival Sciences, Nicolaus -
John Ashbery 125 Part Twelve the Voyages of John Matthias 133
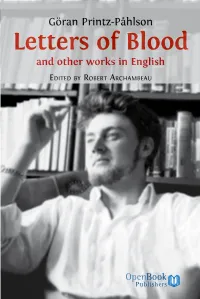
Göran Printz-Påhlson Letters of Blood and other works in English EDITED BY ROBERT ARCHAMBEAU To access digital resources including: blog posts videos online appendices and to purchase copies of this book in: hardback paperback ebook editions Go to: https://www.openbookpublishers.com/product/86 Open Book Publishers is a non-profit independent initiative. We rely on sales and donations to continue publishing high-quality academic works. Letters of Blood and other works in English Göran Printz-Påhlson Edited by Robert Archambeau https://www.openbookpublishers.com © 2011 Robert Archambeau; Foreword © 2011 Elinor Shaffer; ‘The Overall Wandering of Mirroring Mind’: Some Notes on Göran Printz-Påhlson © 2011 Lars-Håkan Svensson; Göran Printz-Påhlson’s original texts © 2011 Ulla Printz-Påhlson. Version 1.2. Minor edits made, May 2016. Some rights are reserved. This book is made available under the Creative Commons Attribution- Non-Commercial-No Derivative Works 2.0 UK: England & Wales License. This license allows for copying any part of the work for personal and non-commercial use, providing author attribution is clearly stated. Attribution should include the following information: Göran Printz-Påhlson, Robert Archambeau (ed.), Letters of Blood. Cambridge, UK: Open Book Publishers, 2011. http://dx.doi.org/10.11647/OBP.0017 In order to access detailed and updated information on the license, please visit https://www. openbookpublishers.com/product/86#copyright Further details about CC BY-NC-ND licenses are available at https://creativecommons.org/ licenses/by-nc-nd/2.0/ All the external links were active on 02/5/2016 unless otherwise stated and have been archived via the Internet Archive Wayback Machine at https://archive.org/web Digital material and resources associated with this volume can be found at https://www. -

GRE Vocabulary
Table of Contents Introduction About Us What is Magoosh? Featured in Why Our Students Love Us How to Use Vocabulary Lists Timmy’s Vocabulary Lists Shirley’s Vocabulary Lists Timmy’s Triumph Takeway Making Words Stick: Memorizing GRE Vocabulary Come up with Clever (and Wacky) Associations Use It or Lose It Do Not Bite Off More Than You Can Chew Read to Be Surprised Takeaways Most Common GRE Words Top 10 GRE Words of 2012 Top 5 Basic GRE Words Common Words that Students Always Get Wrong Tricky “Easy” GRE Words with Multiple Meanings Commonly Confused Sets Interesting (and International) Word Origins Around the World French Words Eponyms Words with Strange Origins Themed Lists Vocab from Within People You Wouldn’t Want To Meet Religious Words Words from Political Scandals Money Matters: How Much Can You Spend? Money Matters: Can’t Spend it Fast Enough Money Matters: A Helping (or Thieving!) Hand Vocabulary from up on High Preposterous Prepositions Them’s Fighting Words gre.magoosh.com 1 Animal Mnemonics Webster’s Favorites “Occupy” Vocabulary Compound Words Halloween Vocabulary Talkative Words By the Letter A-Words C-Words Easily Confusable F-Words Vicious Pairs of V’s “X” words High-Difficulty Words Negation Words: Misleading Roots Difficult Words that the GRE Loves to Use Re- Doesn’t Always Mean Again GRE Vocabulary Books: Recommended Fiction and Non-Fiction The Best American Series The Classics Takeaway Vocabulary in Context: Articles from Magazines and Newspapers The Atlantic Monthly The New Yorker New York Times Book Review The New York Times Practice Questions Sentence Equivalence Text Completion Reading Comprehension GRE Vocabulary: Free Resources on the Internet gre.magoosh.com 2 Introduction This eBook is a compilation of the most popular Revised GRE vocabulary word list posts from the Magoosh GRE blog. -

Magooshgrevocabebook.Pdf
Updated 1/15/13 1 Table of Contents Introduction ............................................................................................................... 3 About Us ................................................................................................................... 4 What is Magoosh? ...................................................................................................... 4 Featured in ............................................................................................................. 4 Why Our Students Love Us ........................................................................................... 5 How to Use Vocabulary Lists ........................................................................................... 7 Timmy’s Vocabulary Lists ............................................................................................ 7 Shirley’s Vocabulary Lists ............................................................................................ 7 Timmy’s Triumph ...................................................................................................... 8 Takeway ................................................................................................................. 8 Making Words Stick: Memorizing GRE Vocabulary................................................................... 9 Come up with Clever (and Wacky) Associations .................................................................. 9 Use It or Lose It ....................................................................................................... -

Chapter 1: the Inter-Group and Present Scholarship……………………………………………………………………………………..57
YOUR BROTHERS, THE CHILDREN OF ISRAEL: ANCIENT NEAR EASTERN POLITICAL DISCCOURSE AND THE PROCESS OF BIBLICAL COMPOSITION A Dissertation Presented to the Faculty of the Graduate School of Cornell University In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy by Dustin Dale Nash January 2015 © 2015 Dustin Dale Nash YOUR BROTHERS, THE CHILDREN OF ISRAEL: ANCIENT NEAR EASTERN POLITICAL DISCOURSE AND THE PROCESS OF BIBLICAL COMPOSITION Dustin Dale Nash, Ph. D. Cornell University 2015 The Hebrew Bible contains seventeen isolated passages, scattered from Genesis to 2 brother”) to define an inter-group“) אח Samuel, that use the Hebrew term relationship between two or more Israelite tribes. For over a century, biblical scholars have interpreted this terminology as conceptually dependent on the birth narratives and genealogies of Gen 29-50, reiterated in stories and lists elsewhere in the biblical corpus. However, examination of the Bible’s depiction of the Israelite tribes as “brothers” outside these seventeen passages indicates that the static genealogical structure of the twelve-tribe system constitutes a late ideological framework that harmonizes dissonant descriptions of Israel as an association of “brother” tribes. Significantly, references to particular tribal groups as “brothers” in the Mari archives yields a new paradigm for understanding the origins of Israelite tribal “brotherhood” that sets aside this ideological structure. Additionally, it reveals the ways in which biblical scribes exploited particular terms and ideas as the fulcrums for editorial intervention in the Hebrew Bible’s composition. More specifically, close analysis of these Akkadian texts reveals the existence of an ancient Near Eastern political discourse of “brotherhood” that identified tribal groups as independent peer polities, bound together through obligations of reciprocal peaceful relations and supportive behavior. -

Getting Results for Hematology Patients Through Access to the Electronic Health Record
doi:10.5737/1181912x163154158 Getting results for hematology patients through access to the electronic health record by David Wiljer, Sima Bogomilsky, Pamela Catton, Cindy perceive in accessing the records and their information-seeking Murray, Janice Stewart and Mark Minden behaviours, including internet usage, rather than clinical characteris - Abstract tics or educational levels (Fowles et al., 2004; Ross et al., 2005). The range of benefits of providing patients with access to their Purpose: To conduct a needs assessment to identify patient and records is still somewhat undefined (Ross & Lin, 2003). Although most provider perceptions about providing patients with access to their studies identify the need for further research in this area, there is some electronic health record in order to develop an online system that is evidence of an increase in patient satisfaction and improved patient appropriate for all stakeholders. Methods: Malignant hematology compliance with self-care (Ross, 2004; Winkelman & Leonard, 2004). patients were surveyed and health care providers were interviewed to Research also suggests that making electronic health records accessible identify issues and validate concerns reported in the literature. Based to patients may empower them (Ralston, Revere, Robins, & Goldberg, on the analysed data, a prototype will be designed to examine the fea - 2004; Ueckert et al., 2003). A recent study from Britain indicated that sibility and efficacy of providing patients with access to their elec - patients find it useful to have access to their health records, but they tronic health record and tailored information. Results: 61% of want to be included in the process of developing the system for patient patients reported using the internet to find health information; 89% access (Pyper et al., 2004). -

Andrew University
Andrew University ANDREWS UNIVERSITY SEMINARY STUDIES The Journal of the Seventh-day Adventist Theological Seminary of Andrews University, Berrien Springs, Michigan 49104-1 5OO, U.S.A. E &tors: Jerry Moon and John W. Reeve Managing E&tor: Karen K. Abrahamson Copy Editors: Leona G. Running and Madeline Johnston Book Review Editor John W. Reeve Book Review Manager: Erhard Gallos CircuIation Manager Erhard Gallos Managing Board Denis Forth, Dean of the Seminary, Chair,Jerry Moon, Secretary; Lyndon G. Furst, Dean of the School of Graduate Studies; Ron Knott, Director, Andrews University Press; Richard Choi; Ken Mulzac; and John W. Reeve. Communications: Phone: (269) 47 1-6023 Fax: (269) 471-6202 Electronic Mail: [email protected] Web: http://www.auss.info A refereed journal, AiVDREWS UNIVERSITY SEMINARYSTUDIES provides a scholarly venue, within the context of biblical faith, for the presentation of research in the area of religious and biblical studies. AUSS publishes research articles, dissertation abstracts, and book reviews on the following topics: biblical archaeology and history of antiquity; Hebrew Bible; New Testament; church history of all periods; historical, biblical, and systematic and philosophical theology; ethics; history of reiigions; and missions. Selected research articles on ministry and Christian education may also be included. The opinions expressed in articles, book reviews, etc., are those of the authors and do not necessarily represent the views of the editors or of the Seventh-day Adventist Theological Seminary. Subscription Information: UNI~RS~SEMINARYSTLIDIESis published in the Spring and the Autumn. The subscription rates for 2008 are as follows: Institutions Individuals Students/Retirees *Air mail rates available upon request Price for Single Copy is $12.00 in U.S.A.