Introduction 1.1 Post-Translational Modifications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Amino Acid Building Block Models – in Brief
Amino Acid Building Block Models – In Brief Key Teaching Points for Amino Acid Building Block Models© Overall Student Learning Objective: What Dictates How a Protein Folds? Amino acids are the building blocks of proteins. All amino acids have an identical core structure consisting of an alpha-carbon, carboxyl group, amino group and R-group (sidechain). A linear chain of amino acids is a polypeptide. The primary sequence of a protein is the linear sequence of amino acids in a polypeptide. Proteins are made up of amino acid monomers linked together by peptide bonds. Peptide bond formation between amino acids results in the release of water (dehydration synthesis or condensation reaction). The protein backbone is characterized by the “N-C-C-N-C-C. .” pattern. The “ends” of the protein can be identified by the N-terminus (amino group) end and the C-terminus (carboxyl group) end. For a more complete lesson guide, please visit: http://www.3dmoleculardesigns.com/3DMD-Files/AABB/ContentsandAssembly.pdf Amino Acid Core Structure Build an amino acid according to the diagram to the right: 1. Identify the alpha carbon, amino group, carboxyl group and R-group (sidechain representation) in the structure you have constructed. Two amino acids can be chemically linked by a reaction called “condensation” or “dehydration synthesis” to form a dipeptide bond linking the two amino acids. A chain of amino acid units (monomers) linked together by peptide bonds is called a polypeptide. General Dipeptide Structure Construct a model of a dipeptide using the amino acid models previously built. 2. What are the products of the condensation reaction (dehydration synthesis)? 3. -
Introduction to Proteins and Amino Acids Introduction
Introduction to Proteins and Amino Acids Introduction • Twenty percent of the human body is made up of proteins. Proteins are the large, complex molecules that are critical for normal functioning of cells. • They are essential for the structure, function, and regulation of the body’s tissues and organs. • Proteins are made up of smaller units called amino acids, which are building blocks of proteins. They are attached to one another by peptide bonds forming a long chain of proteins. Amino acid structure and its classification • An amino acid contains both a carboxylic group and an amino group. Amino acids that have an amino group bonded directly to the alpha-carbon are referred to as alpha amino acids. • Every alpha amino acid has a carbon atom, called an alpha carbon, Cα ; bonded to a carboxylic acid, –COOH group; an amino, –NH2 group; a hydrogen atom; and an R group that is unique for every amino acid. Classification of amino acids • There are 20 amino acids. Based on the nature of their ‘R’ group, they are classified based on their polarity as: Classification based on essentiality: Essential amino acids are the amino acids which you need through your diet because your body cannot make them. Whereas non essential amino acids are the amino acids which are not an essential part of your diet because they can be synthesized by your body. Essential Non essential Histidine Alanine Isoleucine Arginine Leucine Aspargine Methionine Aspartate Phenyl alanine Cystine Threonine Glutamic acid Tryptophan Glycine Valine Ornithine Proline Serine Tyrosine Peptide bonds • Amino acids are linked together by ‘amide groups’ called peptide bonds. -

Peptides & Proteins
Peptides & Proteins (thanks to Hans Börner) 1 Proteins & Peptides Proteuos: Proteus (Gr. mythological figure who could change form) proteuo: „"first, ref. the basic constituents of all living cells” peptos: „Cooked referring to digestion” Proteins essential for: Structure, metabolism & cell functions 2 Bacterium Proteins (15 weight%) 50% (without water) • Construction materials Collagen Spider silk proteins 3 Proteins Structural proteins structural role & mechanical support "cell skeleton“: complex network of protein filaments. muscle contraction results from action of large protein assemblies Myosin und Myogen. Other organic material (hair and bone) are also based on proteins. Collagen is found in all multi cellular animals, occurring in almost every tissue. • It is the most abundant vertebrate protein • approximately a quarter of mammalian protein is collagen 4 Proteins Storage Various ions, small molecules and other metabolites are stored by complexation with proteins • hemoglobin stores oxygen (free O2 in the blood would be toxic) • iron is stored by ferritin Transport Proteins are involved in the transportation of particles ranging from electrons to macromolecules. • Iron is transported by transferrin • Oxygen via hemoglobin. • Some proteins form pores in cellular membranes through which ions pass; the transport of proteins themselves across membranes also depends on other proteins. Beside: Regulation, enzymes, defense, functional properties 5 Our universal container system: Albumines 6 zones: IA, IB, IIA, IIB, IIIA, IIIB; IIB and -

Structure and Synthesis of Antifungal Disulfide
microorganisms Review Structure and Synthesis of Antifungal Disulfide β-Strand Proteins from Filamentous Fungi Györgyi Váradi 1,*, Gábor K. Tóth 1,2 and Gyula Batta 3 1 Department of Medical Chemistry, Faculty of Medicine, University of Szeged, H-6720 Szeged, Hungary; [email protected] 2 MTA-SZTE Biomimetic Systems Research Group, University of Szeged, H-6720 Szeged, Hungary 3 Department of Organic Chemistry, University of Debrecen, H-4032 Debrecen, Hungary; [email protected] * Correspondence: [email protected]; Tel.: +36-62-545-142; Fax: +36-62-545-971 Received: 20 November 2018; Accepted: 24 December 2018; Published: 27 December 2018 Abstract: The discovery and understanding of the mode of action of new antimicrobial agents is extremely urgent, since fungal infections cause 1.5 million deaths annually. Antifungal peptides and proteins represent a significant group of compounds that are able to kill pathogenic fungi. Based on phylogenetic analyses the ascomycetous, cysteine-rich antifungal proteins can be divided into three different groups: Penicillium chrysogenum antifungal protein (PAF), Neosartorya fischeri antifungal protein 2 (NFAP2) and “bubble-proteins” (BP) produced, for example, by P. brevicompactum. They all dominantly have β-strand secondary structures that are stabilized by several disulfide bonds. The PAF group (AFP antifungal protein from Aspergillus giganteus, PAF and PAFB from P. chrysogenum, Neosartorya fischeri antifungal protein (NFAP)) is the best characterized with their common β-barrel tertiary structure. These proteins and variants can efficiently be obtained either from fungi production or by recombinant expression. However, chemical synthesis may be a complementary aid for preparing unusual modifications, e.g., the incorporation of non-coded amino acids, fluorophores, or even unnatural disulfide bonds. -

The Ubiquitin-Proteasome System
Review The ubiquitin-proteasome system DIPANKAR NANDI*, PANKAJ TAHILIANI, ANUJITH KUMAR and DILIP CHANDU Department of Biochemistry, Indian Institute of Science, Bangalore 560 012, India *Corresponding author (Fax, 91-80-23600814; Email, [email protected]) The 2004 Nobel Prize in chemistry for the discovery of protein ubiquitination has led to the recognition of cellular proteolysis as a central area of research in biology. Eukaryotic proteins targeted for degradation by this pathway are first ‘tagged’ by multimers of a protein known as ubiquitin and are later proteolyzed by a giant enzyme known as the proteasome. This article recounts the key observations that led to the discovery of ubiquitin-proteasome system (UPS). In addition, different aspects of proteasome biology are highlighted. Finally, some key roles of the UPS in different areas of biology and the use of inhibitors of this pathway as possible drug targets are discussed. [Nandi D, Tahiliani P, Kumar A and Chandu D 2006 The ubiquitin-proteasome system; J. Biosci. 31 137–155] 1. Introduction biological processes, e.g. transcription, cell cycle, antigen processing, cellular defense, signalling etc. is now well In an incisive article, J Goldstein, the 1985 Nobel laureate established (Ciechanover and Iwai 2004; Varshavsky 2005). for the regulation of cholesterol metabolism (together with During the early days in the field of cytosolic protein M Brown) and Chair for the Jury for the Lasker awards, degradation, cell biologists were intrigued by the requirement laments the fact that it is hard to pick out truly original dis- of ATP in this process as it is well known that peptide bond coveries among the plethora of scientific publications hydrolysis does not require metabolic energy. -

Proteolytic Cleavage—Mechanisms, Function
Review Cite This: Chem. Rev. 2018, 118, 1137−1168 pubs.acs.org/CR Proteolytic CleavageMechanisms, Function, and “Omic” Approaches for a Near-Ubiquitous Posttranslational Modification Theo Klein,†,⊥ Ulrich Eckhard,†,§ Antoine Dufour,†,¶ Nestor Solis,† and Christopher M. Overall*,†,‡ † ‡ Life Sciences Institute, Department of Oral Biological and Medical Sciences, and Department of Biochemistry and Molecular Biology, University of British Columbia, Vancouver, British Columbia V6T 1Z4, Canada ABSTRACT: Proteases enzymatically hydrolyze peptide bonds in substrate proteins, resulting in a widespread, irreversible posttranslational modification of the protein’s structure and biological function. Often regarded as a mere degradative mechanism in destruction of proteins or turnover in maintaining physiological homeostasis, recent research in the field of degradomics has led to the recognition of two main yet unexpected concepts. First, that targeted, limited proteolytic cleavage events by a wide repertoire of proteases are pivotal regulators of most, if not all, physiological and pathological processes. Second, an unexpected in vivo abundance of stable cleaved proteins revealed pervasive, functionally relevant protein processing in normal and diseased tissuefrom 40 to 70% of proteins also occur in vivo as distinct stable proteoforms with undocumented N- or C- termini, meaning these proteoforms are stable functional cleavage products, most with unknown functional implications. In this Review, we discuss the structural biology aspects and mechanisms -

Histone Methylation by Temozolomide; a Classic DNA Methylating Anticancer Drug
ANTICANCER RESEARCH 36: 3289-3300 (2016) Histone Methylation by Temozolomide; A Classic DNA Methylating Anticancer Drug TIELI WANG1, AMANDA J. PICKARD2 and JAMES M. GALLO2 1Department of Chemistry and Biochemistry, California State University Dominguez Hills, Carson, CA, U.S.A.; 2Department of Pharmacology and Systems Therapeutics, Icahn School of Medicine at Mount Sinai, New York, NY, U.S.A. Abstract. Background/Aim: The alkylating agent, adults (1). Despite advances in multimodal therapies of temozolomide (TMZ), is considered the standard-of-care for surgical extirpation, radiotherapy and chemotherapy, GBMs high-grade astrocytomas –known as glioblastoma multiforme remain a cancer of poor prognosis that can be attributed to (GBM)– an aggressive type of tumor with poor prognosis. The the aggressive nature of the tumors and the development of therapeutic benefit of TMZ is attributed to formation of DNA resistance to radiation and chemotherapy (2). Out of adducts involving the methylation of purine bases in DNA. We chemotherapeutic approaches to GBMs, temozolomide investigated the effects of TMZ on arginine and lysine amino (TMZ) is the main alkylating agent used, based on its ability acids, histone H3 peptides and histone H3 proteins. Materials to increase the median survival (3-6). and Methods: Chemical modification of amino acids, histone TMZ possesses favorable pharmacokinetic characteristics H3 peptide and protein by TMZ was performed in phosphate with high oral bioavailability and blood-brain barrier (BBB) buffer at physiological pH. -

Protine Structure
lecture nd 2 Protein structure Color Index: Important Doctor slides Additional notes ∎Objectives • Understand the peptide bonding between amino acids. • Explain the different levels of protein structure and the forces stabilizing these structures and what happens when the protein is denatured. • Define the α-helix and β-sheet as the most commonly encountered secondary structures in a protein molecule. • Correlate the protein structure with function with hemoglobin as an example. • Understand how the misfolding of proteins may lead to diseases like Alzheimer’s or prion disease. ∎What are the proteins ? They are •They are made up of required for hundreds of the structure, Play many or thousands function and critical roles regulation of They are a They do of smaller the body’s large in the most of the unit, called tissue and .work in the amino acids, organs تلعب دور complex of body cell which are حساس في molecules attached to جسم اﻻنسان one another in a long peptide bond ∎What are the proteins ? Proteins can be The sequence of described according amino acids to their large range determines : of functions in the There are mainly 20 1- each protein’s body: different types of unique three- • Antibody amino acids that can dimensional (3D) • Enzyme be combined to make structure • Messenger a protein. 2- its specific • Structural function. component • Transport/storage We choose 20 Amino acids The sequence of Amino Acid in the because of what’s found in DNA strand determines the 3D the DNA. structure of the protein 1.Primary structure • It is the linear sequence of amino acids in a protein **Primary • Covalent bonds in the primary structure of protein: structure proteins 1.Peptide bond are not functional 2.Disulfide bond (if any) (it is not always present) Which is the ”SS bond” , It links two residues of cysteine NEAR TO EACH OTHER as shown in the picture. -

Structure and Formation of Microplasmin (Plasmin Autolysis/Disulfide-Exchange Reactions) HUA-LIN WU*, GUEY-YUEH SHI*, ROBERT C
Proc. Nati. Acad. Sci. USA Vol. 84, pp. 8793-8795, December 1987 Biochemistry Structure and formation of microplasmin (plasmin autolysis/disulfide-exchange reactions) HUA-LIN WU*, GUEY-YUEH SHI*, ROBERT C. WOHLt, AND MYRON L. BENDERt§ *Biochemistry Department, Medical College, National Cheng-Kung University, Tainan, Taiwan, Republic of China 70101; tDepartment of Biochemistry and Molecular Biology, University of Chicago, Chicago, IL 60637; and tDepartments of Chemistry and Biochemistry, Northwestern University, Evanston, IL 60208 Contributed by Myron L. Bender, August 18, 1987 ABSTRACT The structure of human microplasmin, pre- pared from plasmin in alkaline solution, has been studied. Microplasmin consists of two polypeptide chains connected by disulfide bonds. One polypeptide is the B chain of plasmin consisting of 230 amino acids, and the other peptide is the E COOH-terminal portion of the A chain of plasmin consisting of 0cq 31 amino acid residues. Microplasmin has a molecular weight N? of 28,635, calculated from its primary sequence. It is slightly more positively charged than plasminogen and is a more hydrophobic molecule. The proposed scheme for the formation ofmicroplasmin involves autolysis at specific peptide bonds and scrambling of especially sensitive disulfide bonds in alkaline 10 20 30 solution. Elution time (min) Plasmin, a trypsin-like serine protease, catalyzes the hydro- FIG. 1. HPLC chromatography of microplasmin. Microplasmin (100 ,ug) was denatured in 6 M guanidine hydrochloride and injected lytic cleavage of peptide bonds at the COOH sides of onto a ,Bondapak phenylalkyl column (0.4 x 30 cm) using a linear arginines and lysines in protein and peptide substrates (1). acetonitrile gradient. -

From Amino Acids to Proteins
From amino acids to proteins Peptide bond Energetics of folding Backbone conformation The peptide bond • Forward reaction is a dehydration, backward reaction is an hydrolysis • Note energetics • Two amino acids combine to form a dipeptide, three to form a tripeptide, several to form an oligopeptide, many to form a protein Protein sequence • >sp|P54209|ATC1_DUNBI CATION-TRANSPORTING ATPASE CA1 (EC 3.6.1.-) - Dunaliella bioculata. • MVSHASSGRPSSRDTGMVYLGLGMQDAYSSEVQEVAAFYHVDLDRGLSDRDVQQARIKYGRNQMEAE QSTPLWKLILKQFDDLLVKILLGAAIVDFIIAISEGESIQSGLIEPMVILLILVANATVGVVTERNAEKAIEQLKS YEADDATVLRNGQLQLIPSADIVPGDIVELAVGNKVPADTRVSHIYTTSLKIDQSLLTGESQAVEKHTEVVH NEQAVYQDKLNMLFSGTLVVAGRARGIVVGTGSNTAIGKIRDAMGVEEDVVTPLKAKLDEFGALLSKVIA GICVLVWVVNINRFNDPALGGWFQGAIHYFKIAVALAVAAIPEGLPAVVTTCLALGTRKMARHNAIVRTLP SVETLGCTTVICSDKTGTLTTNQMSVIKVAAVQSSSSQLAEFDVTGTTFSPEGMVLGPGGVVLRQPADTP CLAHAAQCAALCNDSQVFVAQKTGTLQRIGESTEIALRVFAEKIGLPSSIRPDRPISRSQFGTNNFWQEDV ERLALLEFSRDRKMMSVLVKGSDRQHNIWSKGAPEFVLRKCSHVLANNGEGAVPLTDNMRQAILSDMQ AFGSRQALRCLALAFKSVPTTTTKLDYSDESGLTFIGLLGMHDPPRPECRSALSTCHNAGIKVIMVTGDNK GTAEAVARQVGALSPSTALAGSDDEDNLGISYTGREFEEMGALGQAAATRNLVVLSRVEPMHKLRLVEL LKAQGHVVAMTGDGVNDAPALLRADIGIAMGSGTAVAKHAADMVLGDDNFATIVFAVAEGRVIFNNTKQF IRYMISSNIGEVVAIFLAALLGLPEVLTPVQLLWVNLVTDGLPATALGFNRADKDMMARGPRRVDDPIVNG WLFLRYLIIGMYVGIVTVYGFIWWYISFPEGGNMTWSQLTHFQACASQPGGAKDCEVFHSKHPTTISMSV LVVVEMFNALNNLSEDSSLLRIPPWDNKWLVGAIATSMALHFGILYTGASAMFGVTGLSFAEWTMVIKLSA PVILVDEIMKAWSRRRQRHPASSRGGPVSLMEIQVPLTSSSRDEAALKLK • FASTA format for presentation of amino acid sequence of a protein • Different -
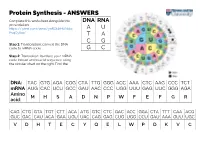
Protein Synthesis - ANSWERS
Protein Synthesis - ANSWERS Complete this worksheet alongside this DNA RNA presentation: https://prezi.com/view/ynRObkHUNckc A U PvqCyI5o/ T A C G Step 1: Transcription: convert the DNA code to mRNA code. G C Step 2: Translation: translate your mRNA code into an amino acid sequence using the circular chart on the right. Find the first letter of your triplet code in the centre and work your way out DNA: TAC GTG AGA CGG CTA TTG GGG ACC AAA CTC AAG CCC TCT mRNA AUG CAC UCU GCC GAU AAC CCC UGG UUU GAG UUC GGG AGA Amino M H S A D N P W F E F G R acid: CAG CTG GTA TGT CTT ACA ATG GTC CTC GAC ACC GGA CTA TTT CAA ACG GUC GAC CAU ACA GAA UGU UAC CAG GAG CUG UGG CCU GAU AAA GUU UGC V D H T E C Y Q E L W P D K V C Exam Questions – Try these relevant questions from past AQA and OCR exams. Answers are included in the answer document 1 Bread contains a mixture of polypeptides known as gluten. Gluten consists of two types of polypeptide: gliadins and glutenins. The table below contains statements about the structures of gluten polypeptides. In the boxes next to each statement, write the level of protein structure (primary, secondary, tertiary, or quaternary) to which the statement refers. [2 marks] Statement Level of protein structure Short α-helical sections are present in both polypeptides because of their high proline content secondary Intermolecular bonds form between glutenin and gliadin polypeptides quaternary Up to 45% of the amino acids in gliadins are glutamine primary Hydrophobic amino acids such as glutamine and proline are not found on the surface of gluten tertiary proteins 2 Human breast milk is produced and secreted by gland cells. -

The Crosstalk Between O-Glcnacylation and Phosphorylation in Insulin Signaling
THE CROSSTALK BETWEEN O-GLCNACYLATION AND PHOSPHORYLATION IN INSULIN SIGNALING by Ping Hu A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland December, 2015 © Ping Hu All Rights Reserved ABSTRACT Extensive crosstalk between phosphorylation and O-GlcNAcylation is involved in regulating insulin signaling. In addition, many of the key regulators of insulin signaling have been shown to be O-GlcNAcylated. In this study, we first explored the crosstalk between phosphorylation and O-GlcNAcylation globally, and then focused on an upstream signaling regulator key to insulin signaling, insulin receptor substrate 1, IRS1. Through regulating cellular O-GlcNAcylation levels in differentiated adipocyte 3T3-L1 cells by specific OGT and OGA inhibitors, we measured the affects of O-GlcNAcylation on the phosphorylation status of key molecules. We observed that O-GlcNAcylation regulates the flux through the two main divergent cellular pathways of insulin signaling, one regulating glucose metabolism and the other regulating cellular proliferation via MAP kinase. Decreased O-GlcNAcylation was associated with increased glucose utilization, and increased O-GlcNAcylation was associated with increased insulin-induced cellular proliferation pathways. Since IRS1 is early in the insulin signaling pathway and is both highly O-GlcNAcylated and highly phosphorylated, we focused on the crosstalk of those two PTMs on IRS1. The phosphorylation spectrum of IRS1 revealed by 2D electrophoretic analyses, partially explained why decreased O-GlcNAcylation facilitated glucose uptake. Two new O- GlcNAcylation sites were mapped through CID/ETD mass spectrometry. With help of protein truncation and site mutagenesis techniques, we propose a mechanism suggesting that the O-GlcNAcylation of Ser635, may be a negative regulator of the C-terminal O- GlcNAcylations on IRS1.