CERVICAL CANCER “An NCD We Can Overcome”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hidden in the Mealie Meal Gender-Based Abuses and Women’S HIV Treatment in Zambia
December 2007 Volume 19, No. 18(A) Hidden in the Mealie Meal Gender-Based Abuses and Women’s HIV Treatment in Zambia I. Summary......................................................................................................................... 1 II. Key Recommendations to the Government of Zambia and Zambia National Assembly ..... 5 III. Methodology................................................................................................................. 7 IV. Background...................................................................................................................9 Gender and HIV/AIDS in Africa........................................................................................ 9 Access and Adherence to Treatment..............................................................................10 Obstacles to Accessing HIV/AIDS Treatment in Zambia..................................................12 Women in Zambia ......................................................................................................... 15 Domestic and Sexual Violence................................................................................. 15 Property Rights ........................................................................................................16 Social, Economic, and Political Indicators of the Status of Women ..........................17 Women’s Political Participation ...............................................................................18 Decision-Making within the Household and Negotiation -

He Provoked the Cadres Who Attacked
No 54 www.diggers.news Monday October 30, 2017 Police raid on UPND reigniting political tension - SACCORD KAMBWILI IS Mirriam Chabala SACCORD executive director Boniface Cheembe (r) says there is no difference between the Zambia Police Service and colonialists. On Friday, heavily armed police raided the UPND secretariat in search of offensive weapons. The hour-long search, however, did not yield any results. GOING INSANE But in an interview, Cheembe said police were creating an impression as if they were in a war with the opposition. ...he provoked the cadres who “We are concerned with what was effected by police on appears to be the continued the secretariat belonging to harassment of opposition the opposition United Party political parties in Zambia for National Development,” Cheembe said. attacked him - Mumbi Phiri owing to a recent raid that To page 6 By Zondiwe Mbewe chairman Kennedy cadres who poured PF deputy Secretary General Kamba colluded with Chibuku Shake- Mumbi Phiri has charged that Lands Minister Jean Shake on him at Sata’s Chishimba Kambwili is going Kapata to organise PF mausoleum. To page 5 insane and she does not want to be part of those who are responding to his political 5 injured in bus accident By Linda Jere rantings. Southern Province Police Commissioner Bonney Kapeso And Mumbi says PF cadres says five people were injured in an accident today involv- harassed Kambwili because ing five vehicles, among them a Mazhandu Family Bus. he was making running “No one has died, five people are injured and out of the commentaries in church when five only two people are seriously injured and are re- President Edgar Lungu was ferred to Mazabuka District Hospital. -

Post-Populism in Zambia: Michael Sata's Rise
This is the accepted version of the article which is published by Sage in International Political Science Review, Volume: 38 issue: 4, page(s): 456-472 available at: https://doi.org/10.1177/0192512117720809 Accepted version downloaded from SOAS Research Online: http://eprints.soas.ac.uk/24592/ Post-populism in Zambia: Michael Sata’s rise, demise and legacy Alastair Fraser SOAS University of London, UK Abstract Models explaining populism as a policy response to the interests of the urban poor struggle to understand the instability of populist mobilisations. A focus on political theatre is more helpful. This article extends the debate on populist performance, showing how populists typically do not produce rehearsed performances to passive audiences. In drawing ‘the people’ on stage they are forced to improvise. As a result, populist performances are rarely sustained. The article describes the Zambian Patriotic Front’s (PF) theatrical insurrection in 2006 and its evolution over the next decade. The PF’s populist aspect had faded by 2008 and gradually disappeared in parallel with its leader Michael Sata’s ill-health and eventual death in 2014. The party was nonetheless electorally successful. The article accounts for this evolution and describes a ‘post-populist’ legacy featuring hyper- partisanship, violence and authoritarianism. Intolerance was justified in the populist moment as a reflection of anger at inequality; it now floats free of any programme. Keywords Elections, populism, political theatre, Laclau, Zambia, Sata, Patriotic Front Introduction This article both contributes to the thin theoretic literature on ‘post-populism’ and develops an illustrative case. It discusses the explosive arrival of the Patriotic Front (PF) on the Zambian electoral scene in 2006 and the party’s subsequent evolution. -

Intra-Party Democracy in the Zambian Polity1
John Bwalya, Owen B. Sichone: REFRACTORY FRONTIER: INTRA-PARTY … REFRACTORY FRONTIER: INTRA-PARTY DEMOCRACY IN THE ZAMBIAN POLITY1 John Bwalya Owen B. Sichone Abstract: Despite the important role that intra-party democracy plays in democratic consolidation, particularly in third-wave democracies, it has not received as much attention as inter-party democracy. Based on the Zambian polity, this article uses the concept of selectocracy to explain why, to a large extent, intra-party democracy has remained a refractory frontier. Two traits of intra-party democracy are examined: leadership transitions at party president-level and the selection of political party members for key leadership positions. The present study of four political parties: United National Independence Party (UNIP), Movement for Multiparty Democracy (MMD), United Party for National Development (UPND) and Patriotic Front (PF) demonstrates that the iron law of oligarchy predominates leadership transitions and selection. Within this milieu, intertwined but fluid factors, inimical to democratic consolidation but underpinning selectocracy, are explained. Keywords: Intra-party Democracy, Leadership Transition, Ethnicity, Selectocracy, Third Wave Democracies Introduction Although there is a general consensus that political parties are essential to liberal democracy (Teorell 1999; Matlosa 2007; Randall 2007; Omotola 2010; Ennser-Jedenastik and Müller 2015), they often failed to live up to the expected democratic values such as sustaining intra-party democracy (Rakner and Svasånd 2013). As a result, some scholars have noted that parties may therefore not necessarily be good for democratic consolidation because they promote private economic interests, which are inimical to democracy and state building (Aaron 1 The authors gratefully acknowledge the comments from the editorial staff and anonymous reviewers. -

Zambia, a 'Christian Nation'
International Journal of Humanities and Social Science Vol. 6, No. 7; July 2016 Zambia, a ‘Christian nation’ in Post Movement for Multiparty Democracy (MMD) Era, 2011-2016 Austin M. Cheyeka Department of Religious Studies University of Zambia P. O. Box 32379, Lusaka Zambia Abstract The declaration of Zambia as a Christian nation in 1991 has become a field of research because of its many faces, the interpretations it has accrued which generate debate and things it has spawned; numerous Pentecostal churches and political parties with the ‘Christian’ name tag. What is more, it has given birth to organizations such as ‘Christian Nation Coalition’, ‘Christian Nation Foundation’ and most significant, a national chapel (House of Prayer for All Nations Tabernacle) yet to be constructed in the capital city next to State house where the declaration occurred. In this article I extend my research on the Christian nation rhetoric beyond Movement for Multiparty Democracy (MMD) era, by examining its status during the Patriotic Front rule from 2011 to 2016, before the August 11, 2016 general elections. In 2011 the party of the president who declared Zambia a Christian nation lost power to a new party of Mr. Michael Chilufya Sata, a staunch Catholic, who, after his demise, was succeeded by Edgar Chagwa Lungu of unknown religious or denominational affiliation. I argue in the article that while Sata hardly used the Christian nation rhetoric, Lungu made the most of it during his campaign thereby revitalizing the Christian nation fervor and prompting some Pentecostal big men and women to rally around him. My stark conclusion is that: Lung perceptively reconfigured the Christian nation rhetoric for political mileage. -

AC Vol 43 No 9
www.africa-confidential.com 3 May 2002 Vol 43 No 9 AFRICA CONFIDENTIAL NIGERIA II 2 NIGERIA I Khaki blues, business suits The generals’ election The military has helped tear the country apart but civilians still defer There are worries whether President Obasanjo’s army can to the soldiers and politicians hold together against growing It is a measure of Nigeria’s political class that in next year’s presidential election, the two most likely communal and religious clashes candidates – Olusegun Obasanjo and Muhammadu Buhari – are retired generals and former military ahead of next year’s polls. And, if leaders. And Nigeria’s wealthiest and most influential kingmaker, another retired general and military it does, its senior officers may want leader, Ibrahim Babangida, may well offer money to both sides. On 25 April, General Obasanjo, to take back power again. ‘persuaded’ by his supporters, declared he would seek a second term; on the same day, Gen. Buhari joined the biggest opposition group, the All People’s Party, on whose ticket he may stand for President. LIBERIA 3 Buhari and Obasanjo hold strong and contrary religious convictions: Obasanjo is a ‘born again’ Christian who has preached at the fundamentalist Winners’ Chapel; Buhari exudes asceticism, publicly Rebels without a plan supporting the extension of the Sharia criminal code (AC Vol 42 No 17). Obasanjo is Yoruba from Ogun Rebels threaten President Taylor State in the south-west; Buhari is Fulani from Katsina in the far north. and give him a pretext to ban Over this looming battle lurks the ghost of a late military leader, Gen. -

Zambia 2013 Human Rights Report
ZAMBIA 2013 HUMAN RIGHTS REPORT EXECUTIVE SUMMARY Zambia is a constitutional republic governed by a democratically elected president and a unicameral national assembly. International and local observers considered national elections held in 2011 to be generally free and fair. Security forces reported to civilian authorities. Serious human rights abuses occurred during the year. The most important were abuses by security forces, including reports of unlawful killings, torture, and beatings; life-threatening prison conditions; and restrictions on freedom of speech, assembly, and association. Other serious human rights problems included arbitrary arrest, prolonged pretrial detention, arbitrary interference with privacy, government corruption, violence and discrimination against women, child abuse, trafficking in persons, discrimination against persons with disabilities and members of the lesbian, gay, bisexual, and transgender (LGBT) community, restrictions on labor rights, forced labor, and child labor. The government took limited steps to prosecute officials suspected of corruption or human rights abuses during the year; however, impunity remained a problem. Section 1. Respect for the Integrity of the Person, Including Freedom from: a. Arbitrary or Unlawful Deprivation of Life There were several reports that the government or its agents committed arbitrary or unlawful killings. After local police authorities were unable to apprehend three men suspected of several killings, the government directed the military to use deadly force against the suspects. On June 25, after a much-publicized investigation into the killings, army soldiers killed Mika, Fabian, and Stefan Mailoni in Mkushi District. The Human Rights Commission (HRC) criticized the killings. On June 14, soldiers belonging to the Zambia National Service shot and killed unarmed civilians Clement Muloongo and Pumulo Lungwangwa in Kampasa village during a scuffle over land rights. -

Speech Delivered by His Excellency Mr
Republic of Zambia SPEECH DELIVERED BY HIS EXCELLENCY MR. EDGAR CHAGWA LUNGU PRESIDENT OF THE REPUBLIC OF ZAMBIA, DURING THE CHURCH SERVICE IN HONOUR OF HIS EXCELLENCY THE LATE DR. LEVY PATRICK MWANAWASA, SC HELD AT THE CATHEDRAL OF THE HOLY CROSS, LUSAKA ON SUNDAY, 19TH AUGUST, 2018 • DR. MAUREEN MWANAWASA, THE FORMER FIRST LADY; • HIS EXCELLENCY MR. RUPIAH BWEZANI BANDA, THE FOURTH REPUBLICAN PRESIDENT; • FORMER VICE-PRESIDENTS PRESENT; • CURRENT AND FORMER MINISTERS; • LEADERS OF OPPOSITION POLITICAL PARTIES PRESENT; • MEMBERS OF THE PRESS; • MY BROTHERS AND SISTERS AND ALL PRESENT: I THANK THE LEVY MWANAWASA FOUNDATION AND THE MWANAWASA FAMILY FOR INVITING US ALL TO COME AND JOIN THEM IN HONOURING THE MEMORY OF OUR LATE PRESIDENT DR. LEVY PATRICK MWANAWASA, SC. SINCE HE PASSED ON TEN YEARS AGO. A DECADE MAY HAVE PASSED SINCE HIS PASSING ON BUT OUR THOUGHTS ARE STILL FRESH WITH SOME OF HIS IDEALS AND THE MANNER IN WHICH HE MANAGED THE AFFAIRS OF THE STATE. 1 | P a g e OUR PARTY THE PATRIOTIC FRONT, VIVIDLY REMEMBER AND WARMLY FEEL THE BROTHERLY HAND-SHAKE WHICH THE LATE PRESIDENT MWANAWASA EXTENDED TO OUR LATE PRESIDENT MICHAEL CHILUFYA SATA. WE EQUALLY REMEMBER THE ASSISTANCE PRESIDENT MWANAWASA RENDERED TO MR SATA TO ENSURE THAT HE RECEIVED THE MEDICAL ATTENTION AT THE TIME, HE WAS UNWELL. THIS WAS TRULY A SIGN OF A GREAT LEADER IN LATE PRESIDENT MWANAWASA WHOSE GESTURE TRANSCENDED POLITICS. TODAY, THE SEED OF NATIONAL BUILDING WHICH PRESIDENT MWANAWASA PLANTED IS SEEN BY OUR COLLABORATION WITH SOME OF THE MMD MEMBERS OF PARLIAMENT. MANY OF THE ZAMBIAN PEOPLE WILL STILL REMEMBER HIM FOR HIS SELFLESS DEMEANOUR. -

Lusaka-Leader-Ii-Workshop-Report.Pdf
SPECIAL OLYMPICS LEADERSHIP ACADEMY LEADER II WORKSHOP LUSAKA, ZAMBIA Special Olympics Leadership Academy Leader II workshop for Africa leaders took place on September 11-14, 2017, in Lusaka, Zambia. The Academy is a leadership development program aimed at engaging and inspiring emerging leaders to become brave, visionary, dynamic leaders that drive the development and growth of Special Olympics in their country or state. PARTICIPANTS SPEAKERS FACILITATORS Esteemed guest speakers and panelists added a lot of value to The following facilitators the Academy through sharing their expertise and advice: conducted the sessions: 32 leaders Esther Lungu, First Lady of Zambia representing 17 • Annemarie Hill, SOI Honorable Given Lubinda, Minister of Justice, Zambia • Brandon Pleaner, CEB countries of Africa Janet Deutsch, US Embassy, Spokesperson, Zambia • Mabel Chileshe Luo Mung’Omba, Region. Luis Gallegos, Ecuador Ambassador to the United Nations, Geneva Belcomm Ltd, UPSTART Skills Bank Maureen Mwanawasa, Former First Lady of Zambia, Managing Partner at • Olga Yakimakho, SOI Levy Mwanawasa and Company • Denis Doolan, SOI Misan Eresanara, Africa Leadership Council, Chair, Nigeria • Charles Nyambe, SO Africa Rajinder Sembi, Past Council Chairperson & Constitutional Area Leader Global Leadership Team-Africa, Lions Clubs International I wish to thank you very much for the feedback. I really Just leaving Lusaka after a very successful African Leadership Academy. We had a great meeting with very powerful leaders “learned a number of good tips from the training and I am “ trying to implement some of those tips. from a very complex and challenging geopolitical region. The leadership of the Academy has been outstanding. -Leonard Chiza Nkosi -Ambassador Luis Gallegos Board Chairman, Special Olympics Malawi Ecuador- Kiera Ambassador Byland to the United Nations Thank you so much for the terrific workshop. -
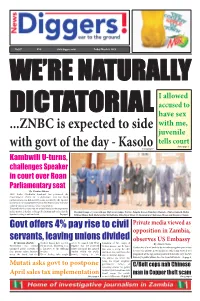
ZNBC Is Expected to Side with Govt of The
No387 K10 www.diggers.news Friday March 8, 2019 WE’RE NATURALLY I allowed accused to DICTATORIAL have sex with me, ...ZNBC is expected to side juvenile tells court Story page 3 with govt of the day - KasoloStory page 7 Kambwili U-turns, challenges Speaker in court over Roan Parliamentary seat By Zondiwe Mbewe NDC leader Chishimba Kambwili has petitioned the Constitutional Court for a declaration that his Roan parliamentary seat did not fall vacant as ruled by the Speaker of the National Assembly Dr Patrick Matibini because the latter violated various provisions of the Constitution. Kambwili who has cited the Attorney General as the respondent in this matter, is further seeking a declaration and order that the President Lungu (c) poses with new High Court judges: Evaristo Pengele, Koreen Etambuyu Mwenda - Zimba, Kenneth Mulife, Speaker’s ruling is null and void. To page 5 Wilfred Muma, Ruth Hachitapika Chibbabbuka, Abha Nayar Patel, SC, Bonaventure Chakwawa Mbewe and Kazimbe Chenda. Govt offers 4% pay rise to civil Private media viewed as opposition in Zambia, servants, leaving unions divided observes US Embassy By Mirriam Chabala workers’ unions have rejected not to be named, told News formation of two camps of By Stuart Lisulo Government has offeredthe proposal, describing it as Diggers! that the proposed workers unions - one for those Zambia has a lot of work to do in embracing divergent views unionised public servants a a disservice to the suffering salary increment has spurred that want to accept the offer because the private news media are still being viewed as a four percent salary increase workers. -

Zambia Relations the Leaders of Zambian Freedom Struggle, Such As
India - Zambia Relations The leaders of Zambian freedom struggle, such as Dr. Kenneth Kaunda, drew inspiration from India’s freedom struggle, particularly Mahatma Gandhi. Gandhi continues to inspire and invoke admiration in Zambia and among its leaders, even the younger generation. The warm relations have continued into this century. Over these last several decades, India has come to be seen as a reliable partner and friend and is described by Zambian leaders as an “all weather and time-tested friend”. The relationship continues to be driven by mutual respect and is based in a spirit of partnership for mutual benefit. Bilateral Visits: High level visits have been a feature of our historical bilateral relationship. During his presidency, Dr. Kenneth Kaunda, the first Republican President of Zambia, visited India more than ten times beginning in 1967. The Late President Mwanawasa paid a state visit to India in April 2003. President Michael Chilufya Sata, accompanied by First Lady Mrs. Christine Kaseba, paid a private visit to India in March 2012 and First President Dr. Kenneth Kaunda paid a private visit to India in June 2012. In 2013, Vice President Dr. Guy Scott led a high-power official and business delegation, comprising Ministers of Commerce, Trade & Industry, Gender and Child Development and Deputy Minister of Mining, to the 9th CII-EXIM Bank Conclave in New Delhi in March 2013 at which Zambia was a Focus Country. Deputy Health Minister Dr. Chitalu Chilufa represented Zambia at the India-Africa Health Forum, held in New Delhi on 24th April, 2015. Ms. Margaret M. Mwanakatwe, Minister of Commerce, Trade and Industry participated in the 4th India-Africa Business Forum meeting in New Delhi on 24th October 2015 on the sidelines of IAFS-III. -

Zambia Human Rights Report 2002
ZAMBIA HUMAN RIGHTS REPORT 2002 ZZZaaammmbbbiiiaaa HHHuuummmaaannn RRRiiiggghhhtttsss RRReeepppooorrrttt 222000000222 “When we have the courage to speak out-to break silence-we inspire the rest of the ‘moderates’ in our communities to speak up and voice their views.” SHARON SCHUSTER (New York City Photographer) Inter-African Network for Human Rights and Development (Afronet) 2 ZAMBIA HUMAN RIGHTS REPORT 2002 © 2003 Afronet All rights reserved ISBN 9982 - 32 - 003 - 3 Published by The Inter-African Network for Human Rights and Development (AFRONET) P.O Box 31145 Tel: +260 1 25 18 14 Lusaka, Zambia e-mail: [email protected] url: http://afronet.org.za 3 ZAMBIA HUMAN RIGHTS REPORT 2002 For information on the Report contact Afronet - Research and Fact Finding e-mail: [email protected] 4 ZAMBIA HUMAN RIGHTS REPORT 2002 CONTENTS Acronyms List of Boxes Providing Additional Information Foreword Introduction PART ONE CIVIL AND POLITICAL RIGHTS Chapter One The Rule of Law, Justice and the Judiciary Chapter Two Freedom of Expression and the Media Chapter Three Freedom of Assembly and Association Chapter Four The Right to Political Choice Chapter Five The Police, Torture, and the Victims PART TWO ECONOMIC SOCIAL AND CULTURAL RIGHTS Chapter Six Food, Poverty and the State Chapter Seven Getting Educated - (The Right to Education) Chapter Eight Health and the State PART THREE WOMEN AND THE STATE PART FOUR STATE INSTITUTIONS AND HUMAN RIGHTS PROTECTION PART FIVE SUMMARY OF CONCLUSIONS APPENDICES Appendix I List of International Instruments ratified