Clinical Assessment and Examination in Orthopedics, 2Nd Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Common Problems of the Shoulder, Examination and Omt
COMMON PROBLEMS OF THE SHOULDER, EXAMINATION AND OMT Richard Margaitis DO Assistant Professor Family Medicine/NMM/SM Florida Hospital October 19th 2015 Objectives • At the conclusion of this lecture, the attendee should be able to: Identify basic anatomic landmarks of the shoulder Identify typical patient symptoms/complaints Differentiate various medical diagnoses of the shoulder Perform & understand the indications of specific shoulder tests Identify various diagnostic and treatment modalities Perform various OMT techniques for shoulder dysfunctions Pre-Test Question #1 1) Which nerve is most commonly injured with a gleno- humeral shoulder dislocation? a) Axillary Nerve b) Suprascapular Nerve c) Musculo-cutaneous Nerve d) Radial Nerve c) Ulnar Nerve Answer: A) Axillary Nerve Pre-Test Question #2 2) How many ligaments make up the Coraco-clavicular Ligament? a) One b) Two c) Three d) Four c) Five Answer: B) Two The Conoid and Trapezoid Ligaments Pre-Test Question #3 3) Which of the following tests is used to evaluate for Bicipital Tendonitis? a) Jobe b) Apprehension c) Hawkins’ d) Apleys e) Speeds Answer: E) Speeds Pre-Test Question #4 4) How many muscles either attach or originate on the Scapula? a) 7 b) 10 c) 15 d) 17 e) 21 Answer: D) 17 Muscles attaching to or originating on the Scapula Serratus Anterior Supraspinatus Subscapularis Trapezius Teres Major Teres Minor Triceps Brachii (long head) Biceps Brachii (short & long heads) Rhomboid Major Rhomboid Minor Coracobrachialis Omohyoid (inferior belly) Latiissimus Dorsi Deltoid Levator -

Paper Abstracts
PAPER ABSTRACTS Paper #1 Full-Thickness Articular Cartilage Defects of the Trochlea: Long-Term Patient Outcomes at 4-6 Years . .Jon E Browne, Kansas City, MO, USA Paper #2 •Transplantation of Cartilage-Like Tissue Made by Tissue Engineering . .Mitsuo Ochi, Izumo-shi, JAPAN Paper #3 Semitendinosus Regrowth: The Physiologic Properties of the Lizard Tail Phenomenon . .Mark David Miller, Charlottesville, USA Paper #4 Failure Properties of the Fibular Collateral and Popliteofibular Ligaments, and Popliteus Musculotendinous Complex . .Tim Bollom, Gainesville, FL, USA Paper #5 The Effect of Growth Factor therapy for Over-Stretched Anterior Cruciate Ligament Injury With Partial Mid-Substance Laceration: An Experimental Study . .Eiji Kondo, Sapporo, JAPAN Paper #6 Physiological Fracture Prophylaxis of the Distal Radius Prior to Falling . .Anton Arndt, Huddinge, SWEDEN Paper #7 Animated 3D Motion of the Normal and Injured Wrist . .Michael J Sandow, Adelaide, AUSTRALIA Paper #8 Tissue Engineering for Knee Ligament Reconstruction . .F. van Eijk, Amsterdam, NETHERLANDS Paper #9 Changes in Gene Expression of Human Articular Chondrocytes in Cell Culture . .Gabriele Striessnig, Vienna, AUSTRIA Paper #10 Existence of Slow-Cycling Cells in Meniscus: Implication on Precursor Cells . .Eisaku Fujimoto, Hiroshima, JAPAN Paper #11 The Effects of Hyaluronic Acid in the Healing of Achilles Tendon Repair . .Sinan Karaoglu, Kayseri, TURKEY Paper #12 Superior topology of the Human Talus . .Adam M Butler, Randwick, AUSTRALIA Paper #13 Diagnosis and Arthroscopic Treatment of Superior Labrum Lesion Associated With Shoulder Anterior Instability: Slap Type V. .Benno Ejnisman, São Paulo, BRAZIL Paper #14 The Reliability of MR-Arthrography in Patients With Anterior Shoulder Instability . .Pol E Huysmans, Amstelveen, NETHERLANDS Paper #15 Significance of Postoperative Arthro MRI in Predicting 5 Year Results of Arthroscopically Treated Recurrent Shoulder Dislocations . -
Souvenir Programme, This Information Is Correct
1 SUBSPECIALTY INTEREST GROUP MEETINGS At time of printing this souvenir programme, this information is correct. Should there be any last minute changes, please refer to the signage outside each meeting room or enquire at the secretariat counter. SUBSPECIALTY INTEREST GROUP MEETING DATE TIME MEETINGS ROOM ASEAN OA Education Committee 21st May 2015 0830 - 1700hrs Kelantan Room Meeting Hand Subspecialty Interest Group 22nd May 2015 1030 - 1200hrs Pahang Room Foot & Ankle Subspecialty Interest Negeri Sembilan 22nd May 2015 1030 - 1200hrs Group Room Spine Subspecialty Interest Group 22nd May 2015 1130 - 1200hrs Johore Room Negeri Sembilan Paediatrics Subspecialty Interest Group 22nd May 2015 1400 - 1530hrs Room ASEAN OA Council Meeting 22nd May 2015 1400 - 1730hrs Kelantan Room Arthroplasty Subspecialty Interest 22nd May 2015 1600 - 1730hrs Pahang Room Group Negeri Sembilan Trauma Subspecialty Interest Group 22nd May 2015 1600 - 1730hrs Room Oncology Subspecialty Interest Group 23rd May 2015 1030 - 1200hrs Penang Room Sports Subspecialty Interest Group 23rd May 2015 1400 - 1530hrs Johore Room MOA Annual General Meeting 23rd May 2014 1600 - 1730hrs Johore Room 23rd May 2015 0800 - 1730hrs APOA Council Meeting Kelantan Room 24th May 2015 0800 - 1500hrs 2 INDEX PAGE NO. DESCRIPTION 2 Subspecialty Interest Group Meetings Malaysian Orthopaedic Association Office Bearers 4 45th Malaysian Orthopaedic Association Annual Scientific Meeting 2015 Organising Committee Welcome Message from President of Malaysian Orthopaedic Association and 5 Organising -

Neonatal Orthopaedics
NEONATAL ORTHOPAEDICS NEONATAL ORTHOPAEDICS Second Edition N De Mazumder MBBS MS Ex-Professor and Head Department of Orthopaedics Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences Kolkata, West Bengal, India Visiting Surgeon Department of Orthopaedics Chittaranjan Sishu Sadan Kolkata, West Bengal, India Ex-President West Bengal Orthopaedic Association (A Chapter of Indian Orthopaedic Association) Kolkata, West Bengal, India Consultant Orthopaedic Surgeon Park Children’s Centre Kolkata, West Bengal, India Foreword AK Das ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD. New Delhi • London • Philadelphia • Panama (021)66485438 66485457 www.ketabpezeshki.com ® Jaypee Brothers Medical Publishers (P) Ltd. Headquarters Jaypee Brothers Medical Publishers (P) Ltd. 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offices J.P. Medical Ltd. Jaypee-Highlights Medical Publishers Inc. Jaypee Brothers Medical Publishers Ltd. 83, Victoria Street, London City of Knowledge, Bld. 237, Clayton The Bourse SW1H 0HW (UK) Panama City, Panama 111, South Independence Mall East Phone: +44-2031708910 Phone: +507-301-0496 Suite 835, Philadelphia, PA 19106, USA Fax: +02-03-0086180 Fax: +507-301-0499 Phone: +267-519-9789 Email: [email protected] Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd. Jaypee Brothers Medical Publishers (P) Ltd. 17/1-B, Babar Road, Block-B, Shaymali Shorakhute, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +00977-9841528578 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2013, Jaypee Brothers Medical Publishers All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher. -

Shoulder Injuries Diagnosis and Treatment
SHOULDER INJURIES DIAGNOSIS AND TREATMENT BONE AND JOINT HEALTH JASSIN M. JOURIA Dr. Jassin M. Jouria is a practicing Emergency Medicine physician, professor of academic medicine, and medical author. He graduated from Ross University School of Medicine and has completed his clinical clerkship training in various teaching hospitals throughout New York, including King’s County Hospital Center and Brookdale Medical Center, among others. Dr. Jouria has passed all USMLE medical board exams, and has served as a test prep tutor and instructor for Kaplan. He has developed several medical courses and curricula for a variety of educational institutions. Dr. Jouria has also served on multiple levels in the academic field including faculty member and Department Chair. Dr. Jouria continues to serve as a Subject Matter Expert for several continuing education organizations covering multiple basic medical sciences. He has also developed several continuing medical education courses covering various topics in clinical medicine. Recently, Dr. Jouria has been contracted by the University of Miami/Jackson Memorial Hospital’s Department of Surgery to develop an e- module training series for trauma patient management. Dr. Jouria is currently authoring an academic textbook on Human Anatomy & Physiology. ABSTRACT Over time, the potential for injury or just general wear and tear on bones and joints can impact a person’s quality of life. Even in younger individuals, repetitive activities, such as repeatedly throwing a baseball, can cause arthritic pain and joint tears that cause pain and limit a person’s body to function as it was designed. However, many treatment options, both surgical and non-surgical, are available to provide relief and to restore normal functioning. -

Thoracolumbar Spine
THORACOLUMBAR SPINE Code No. TITTLE Running Serial No. time (Description) Minutes 29028 Percutaneous Lumbar Discectomy, Current 15:00 TL.S practice 1 Designed to teach the operative technique of percutaneous lumbar discectomy & to point out the importance of correct positioning of the instrument in order to avoid neural injury & achieve better evacuation of the posteriorly lodged fragments. 22046 Anterior Approaches to the Lumbar Spine TL.S Demonstrates the anterior lumbar spine 2 anatomy & the anterior retroperitoneal, anterior transperitoneal & anterolateral flank surgical approaches. The anterior lumbar arthrodesis is shown through cadaveric dissection, graphics & models. 22044 Anterior Retroperitioneal Approach & TL.S Fusion of the Lumbar Spine. 3 Demonstrates anterior retroperitoneal approach which provides direct access to the spine, as well as the intervening discs between the diaphragm & the sacrum. The approach is utilized for traumatic, infectious, degenerative, congenital & developmental anomalies of the lumbar spine. 21029 Anterior Spinal Canal Decompression & TL.S Interbody Fusion for Treatment of 4 Herniated Thoracic Disks 21028 Arthroscopic Microdiscectomy TL.S 5 21030 Evaluation of the Scoliosis Patient 38:00 TL.S Demonstrates the proper method of 6 evaluating the adolescent scoliosis patient, using physical examination & radiological evaluation & emphasizing the use of the spinal & neurologic evaluation. 29029 Cotrel-Dubousset Instrumentation for TL.S single thoracic idiopathic scoliosis 7 Demonstrates the classic technique of Cotrel- Dubousset instrumentation for a flexible right thoracic idiopathic scoliosis. 22045 Laminotomy/I) disketomy Surgical TL.S Technique with the patient in kneeling 8 position 22047 Microscopic Lumbar Laminectomy 38:00 TL.S With vedio camera 9 20009 The Nulceotome procedure in Automated TL.S Percutaneous Lumbar discectomy 10 Discusses the indications & contraindications for percutaneous discectomy & provides a step by step illustration of the procedure. -

Examination of the Spine
Page 1 of 7 Examination of the Spine Neck and back pain are common presentations in primary care. Many cases of neck and back pain are due to benign functional or postural causes but a thorough history and examination is essential to assess the cause (see articles Low Back Pain and Sciatica, Thoracic Back Pain and Neck Pain), any associated psychological difficulties (eg depression, anxiety or somatisation disorder), and any functional impairment, including restrictions with work, leisure and domestic activities. General examination of the spine The examination should begin as soon as you first see the patient and continues with careful observation during the whole consultation. It is essential to observe the patient's gait and posture. Inconsistency between observed function and performance during specific tests may help to differentiate between physical and functional causes for the patient's symptoms. Inspection Examination of any localised spinal disorder requires inspection of the entire spine. The patient should therefore undress to their underwear. Look for any obvious swellings or surgical scars. Assess for deformity: scoliosis, kyphosis, loss of lumbar lordosis or hyperlordosis of the lumbar spine. Look for shoulder asymmetry and pelvic tilt. Observe the patient walking to assess for any abnormalities of gait. Palpation Palpate for tenderness over bone and soft tissues. Perform an abdominal examination to identify any masses, and consider a rectal examination (cauda equina syndrome may present with low back pain, pain in the legs and unilateral or bilateral lower limb motor and/or sensory abnormality, bowel and/or bladder dysfunction with saddle and perineal anaesthesia, urinary dysfunction and bowel disturbances, and rectal examination may reveal loss of anal tone and sensation). -

Escharotomy Incisions 17
Emergency War Surgery Second United States Revision of The Emergency War Surgery NATO Handbook Thomas E. Bowen, M.D. Editor BG, MC, U.S. Army Ronald Bellamy, M.D. Co-Editor COL, MC, U.S. Army United States Department of Defense United States Government Printing Office Washington, D.C. 1988 Peer Review Status: Internally Peer Reviewed Creation Date: Unknown Last Revision Date: 1988 Contents Foreword Preface Prologue Acknowledgments Chapter I. General Considerations of Forward Surgery Part I. Types of Wounds and Injuries II. Missile-Caused Wounds III. Burn Injury IV. Cold Injury V. Blast Injuries VI. Chemical Injury VII. Mass Casualties in Thermonuclear Warfare VIII. Multiple Injuries Part II. Response of the Body to Wounding IX. Shock and Resuscitation X. Compensatory and Pathophysiological Responses to Trauma XI. Infection Part III. General Considerations of Wound Management XII. Sorting of Casualties XIII. Aeromedical Evacuation XIV. War Surgery Within the Division XV. Anesthesia and Analgesia XVI. Wounds and Injuries of the Soft Tissues XVII. Crush Injury XVIII. Vascular Injuries XIX. Wounds and Injuries of Bones and Joints XX. Wounds and Injuries of Peripheral Nerves XXI. Amputations Part IV. Regional Wounds and Injuries XXII. Craniocerebral Injury XXIII. Maxillofacial Wounds and Injuries XXIV. Wounds and Injuries of the Eye XXV. Laser Injury of the Eye XXVI. Wounds and Injuries of the Ear XXVII. Wounds and Injuries of the Neck XXVIII. Wounds and Injuries of the Chest XXIX. Wounds of the Abdomen XXX. Reoperative Abdominal Surgery XXXI. Wounds and Injuries of the Genitourinary Tract XXXII. Wounds and Injuries of the Hand XXXIII. Wounds and Injuries of the Spinal Column and Cord Appendixes A. -

Musculoskeletal Clinical Vignettes a Case Based Text
Leading the world to better health MUSCULOSKELETAL CLINICAL VIGNETTES A CASE BASED TEXT Department of Orthopaedic Surgery, RCSI Department of General Practice, RCSI Department of Rheumatology, Beaumont Hospital O’Byrne J, Downey R, Feeley R, Kelly M, Tiedt L, O’Byrne J, Murphy M, Stuart E, Kearns G. (2019) Musculoskeletal clinical vignettes: a case based text. Dublin, Ireland: RCSI. ISBN: 978-0-9926911-8-9 Image attribution: istock.com/mashuk CC Licence by NC-SA MUSCULOSKELETAL CLINICAL VIGNETTES Incorporating history, examination, investigations and management of commonly presenting musculoskeletal conditions 1131 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey Prof. John O'Byrne Mr. Iain Feeley Dr. Richie Downey Dr. Martin Kelly Mr. Iain Feeley Dr. Lauren Tiedt Dr. Martin Kelly Department of General Practice, RCSI Dr. Lauren Tiedt Dr. Mark Murphy Department of General Practice, RCSI Dr Ellen Stuart Dr. Mark Murphy Department of Rheumatology, Beaumont Hospital Dr Ellen Stuart Dr Grainne Kearns Department of Rheumatology, Beaumont Hospital Dr Grainne Kearns 2 2 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey TABLE OF CONTENTS Prof. John O'Byrne Mr. Iain Feeley Introduction ............................................................. 5 Dr. Richie Downey Dr. Martin Kelly General guidelines for musculoskeletal physical Mr. Iain Feeley examination of all joints .................................................. 6 Dr. Lauren Tiedt Dr. Martin Kelly Upper limb ............................................................. 10 Department of General Practice, RCSI Example of an upper limb joint examination ................. 11 Dr. Lauren Tiedt Shoulder osteoarthritis ................................................. 13 Dr. Mark Murphy Adhesive capsulitis (frozen shoulder) ............................ 16 Department of General Practice, RCSI Dr Ellen Stuart Shoulder rotator cuff pathology ................................... -

Mcmaster Musculoskeletal Clinical Skills Manual 1E
McMaster Musculoskeletal Clinical Skills Manual Authors Samyuktha Adiga Dr. Raj Carmona, MBBS, FRCPC Illustrator Jenna Rebelo Editors Caitlin Lees Dr. Raj Carmona, MBBS, FRCPC In association with the Medical Education Interest Group Narendra Singh and Jacqueline Ho (co-chairs) FOREWORD AND ACKNOWLEDGEMENTS The McMaster Musculoskeletal Clinical Skills Manual was produced by members of the Medical Education Interest Group (co-chairs Jacqueline Ho and Narendra Singh), and Dr. Raj Carmona, Assistant Professor of Medicine at McMaster University. Samyuktha Adiga and Dr. Carmona wrote the manual. Illustrations were done by Jenna Rebelo. Editing was performed by Caitlin Lees and Dr. Carmona. The Manual, completed in August 2012, is a supplement to the McMaster MSK Examination Video Series created by Dr. Carmona, and closely follows the format and content of these videos. The videos are available on Medportal (McMaster students), and also publicly accessible at RheumTutor.com and fhs.mcmaster.ca/medicine/rheumatology. McMaster Musculoskeletal Clinical Skills Manual S. Adiga, J. Rebelo, C. Lees, R. Carmona McMaster Musculoskeletal Clinical Skills Manual TABLE OF CONTENTS General Guide 1 Hip Examination 3 Knee Examination 6 Ankle and Foot Examination 12 Examination of the Back 15 Shoulder Examination 19 Elbow Examination 24 Hand and Wrist Examination 26 Appendix: Neurological Assessment 29 1 GENERAL GUIDE (Please see videos for detailed demonstration of examinations) Always wash your hands and then introduce yourself to the patient. As with any other exam, ensure adequate exposure while respecting patient's modesty. Remember to assess gait whenever doing an examination of the back or any part of the lower limbs. Inspection follows the format: ● S welling ● E rythema ● A trophy ● D eformities ● S cars, skin changes, etc. -
Harbor Chiropractic, P.C
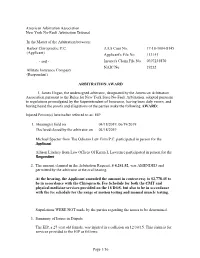
American Arbitration Association New York No-Fault Arbitration Tribunal In the Matter of the Arbitration between: Harbor Chiropractic, P.C. AAA Case No. 17-18-1084-8145 (Applicant) Applicant's File No. 113141 - and - Insurer's Claim File No. 0397235870 NAIC No. 19232 Allstate Insurance Company (Respondent) ARBITRATION AWARD I, James Hogan, the undersigned arbitrator, designated by the American Arbitration Association pursuant to the Rules for New York State No-Fault Arbitration, adopted pursuant to regulations promulgated by the Superintendent of Insurance, having been duly sworn, and having heard the proofs and allegations of the parties make the following AWARD: Injured Person(s) hereinafter referred to as: EIP 1. Hearing(s) held on 04/18/2019, 06/19/2019 Declared closed by the arbitrator on 04/18/2019 Michael Spector from The Odierno Law Firm P.C. participated in person for the Applicant Allison Lindsey from Law Offices Of Karen L Lawrence participated in person for the Respondent 2. The amount claimed in the Arbitration Request, $ 4,241.52, was AMENDED and permitted by the arbitrator at the oral hearing. At the hearing, the Applicant amended the amount in controversy to $2,778.45 to be in accordance with the Chiropractic Fee Schedule for both the CMT and physical medicine services provided on the 18 DOS, but also to be in accordance with the fee schedule for the range of motion testing and manual muscle testing. Stipulations WERE NOT made by the parties regarding the issues to be determined. 3. Summary of Issues in Dispute The EIP, a 27 year old female, was injured in a collision on 12/30/15. -

AIS-Pennhip-Manual.Pdf
Training Manual Table of Contents Chapter 1: Introduction and Overview ............................................................................................... 5 Brief History of PennHIP ........................................................................................................................................5 Current Status of CHD ...........................................................................................................................................5 Requirements for Improved Hip Screening ............................................................................................................6 PennHIP Strategies ................................................................................................................................................7 The AIS PennHIP Procedure .................................................................................................................................8 AIS PennHIP Certification ......................................................................................................................................8 Purchasing a Distractor ..........................................................................................................................................9 Antech Imaging Services........................................................................................................................................9 Summary ............................................................................................................................................................