Spine to Move Mobile Lumbar Spine 7) Cauda Equina Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Souvenir Programme, This Information Is Correct
1 SUBSPECIALTY INTEREST GROUP MEETINGS At time of printing this souvenir programme, this information is correct. Should there be any last minute changes, please refer to the signage outside each meeting room or enquire at the secretariat counter. SUBSPECIALTY INTEREST GROUP MEETING DATE TIME MEETINGS ROOM ASEAN OA Education Committee 21st May 2015 0830 - 1700hrs Kelantan Room Meeting Hand Subspecialty Interest Group 22nd May 2015 1030 - 1200hrs Pahang Room Foot & Ankle Subspecialty Interest Negeri Sembilan 22nd May 2015 1030 - 1200hrs Group Room Spine Subspecialty Interest Group 22nd May 2015 1130 - 1200hrs Johore Room Negeri Sembilan Paediatrics Subspecialty Interest Group 22nd May 2015 1400 - 1530hrs Room ASEAN OA Council Meeting 22nd May 2015 1400 - 1730hrs Kelantan Room Arthroplasty Subspecialty Interest 22nd May 2015 1600 - 1730hrs Pahang Room Group Negeri Sembilan Trauma Subspecialty Interest Group 22nd May 2015 1600 - 1730hrs Room Oncology Subspecialty Interest Group 23rd May 2015 1030 - 1200hrs Penang Room Sports Subspecialty Interest Group 23rd May 2015 1400 - 1530hrs Johore Room MOA Annual General Meeting 23rd May 2014 1600 - 1730hrs Johore Room 23rd May 2015 0800 - 1730hrs APOA Council Meeting Kelantan Room 24th May 2015 0800 - 1500hrs 2 INDEX PAGE NO. DESCRIPTION 2 Subspecialty Interest Group Meetings Malaysian Orthopaedic Association Office Bearers 4 45th Malaysian Orthopaedic Association Annual Scientific Meeting 2015 Organising Committee Welcome Message from President of Malaysian Orthopaedic Association and 5 Organising -

Neonatal Orthopaedics
NEONATAL ORTHOPAEDICS NEONATAL ORTHOPAEDICS Second Edition N De Mazumder MBBS MS Ex-Professor and Head Department of Orthopaedics Ramakrishna Mission Seva Pratishthan Vivekananda Institute of Medical Sciences Kolkata, West Bengal, India Visiting Surgeon Department of Orthopaedics Chittaranjan Sishu Sadan Kolkata, West Bengal, India Ex-President West Bengal Orthopaedic Association (A Chapter of Indian Orthopaedic Association) Kolkata, West Bengal, India Consultant Orthopaedic Surgeon Park Children’s Centre Kolkata, West Bengal, India Foreword AK Das ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD. New Delhi • London • Philadelphia • Panama (021)66485438 66485457 www.ketabpezeshki.com ® Jaypee Brothers Medical Publishers (P) Ltd. Headquarters Jaypee Brothers Medical Publishers (P) Ltd. 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offices J.P. Medical Ltd. Jaypee-Highlights Medical Publishers Inc. Jaypee Brothers Medical Publishers Ltd. 83, Victoria Street, London City of Knowledge, Bld. 237, Clayton The Bourse SW1H 0HW (UK) Panama City, Panama 111, South Independence Mall East Phone: +44-2031708910 Phone: +507-301-0496 Suite 835, Philadelphia, PA 19106, USA Fax: +02-03-0086180 Fax: +507-301-0499 Phone: +267-519-9789 Email: [email protected] Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd. Jaypee Brothers Medical Publishers (P) Ltd. 17/1-B, Babar Road, Block-B, Shaymali Shorakhute, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +00977-9841528578 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2013, Jaypee Brothers Medical Publishers All rights reserved. No part of this book may be reproduced in any form or by any means without the prior permission of the publisher. -
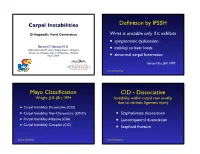
Carpal-Instability-Slide-Summary.Pdf
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

Disorders of the Knee
DisordersDisorders ofof thethe KneeKnee PainPain Swelling,Swelling, effusioneffusion oror hemarthrosishemarthrosis LimitedLimited jointjoint motionmotion Screw home mechanism – pain, stiffness, fluid, muscular weakness, locking InstabilityInstability – giving way, laxity DeformityDeformity References: 1. Canale ST. Campbell’s operative orthopaedics. 10th edition 2003 Mosby, Inc. 2. Netter FH. The Netter collection of Medical illustrations – musculoskeletal system, Part I & II. 1997 Novartis Pharmaceuticals Corporation. 3. Magee DJ. Orthopedic Physical assessment. 2nd edition 1992 W. B. Saunders Company. 4. Hoppenfeld S. Physical examination of the spine and extremities. 1976 Appleton-century-crofts. AnteriorAnterior CruciateCruciate LigamentLigament Tibial insertion – broad, irregular, diamond-shaped area located directly in front of the intercondylar eminence Femoral attachment Femoral attachment Figure 43-24 In addition to their – semicircular area on the posteromedial synergistic functions, cruciate aspect of the lateral condyle and collateral ligaments exercise 33 mm in length basic antagonistic function 11 mm in diameter during rotation. A, In external Anteromedial bundle — tight in flexion rotation it is collateral ligaments that tighten and inhibit excessive Posterolateral bundle — tight in extension rotation by becoming crossed in 90% type I collagen space. B, In neutral rotation none 10% type III collagen of the four ligaments is under unusual tension. C, In internal Middle geniculate artery rotation collateral ligaments Fat -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

Knee Pain in Children: Part I: Evaluation
Knee Pain in Children: Part I: Evaluation Michael Wolf, MD* *Pediatrics and Orthopedic Surgery, St Christopher’s Hospital for Children, Philadelphia, PA. Practice Gap Clinicians who evaluate knee pain must understand how the history and physical examination findings direct the diagnostic process and subsequent management. Objectives After reading this article, the reader should be able to: 1. Obtain an appropriate history and perform a thorough physical examination of a patient presenting with knee pain. 2. Employ an algorithm based on history and physical findings to direct further evaluation and management. HISTORY Obtaining a thorough patient history is crucial in identifying the cause of knee pain in a child (Table). For example, a history of significant swelling without trauma suggests bacterial infection, inflammatory conditions, or less likely, intra- articular derangement. A history of swelling after trauma is concerning for potential intra-articular derangement. A report of warmth or erythema merits consideration of bacterial in- fection or inflammatory conditions, and mechanical symptoms (eg, lock- ing, catching, instability) should prompt consideration of intra-articular derangement. Nighttime pain and systemic symptoms (eg, fever, sweats, night sweats, anorexia, malaise, fatigue, weight loss) are associated with bacterial infections, inflammatory conditions, benign and malignant musculoskeletal tumors, and other systemic malignancies. A history of rash or known systemic inflammatory conditions, such as systemic lupus erythematosus or inflammatory bowel disease, should raise suspicion for inflammatory arthritis. Ascertaining the location of the pain also can aid in determining the cause of knee pain. Anterior pain suggests patellofemoral syndrome or instability, quad- riceps or patellar tendinopathy, prepatellar bursitis, or apophysitis (patellar or tibial tubercle). -

Musculoskeletal Clinical Vignettes a Case Based Text
Leading the world to better health MUSCULOSKELETAL CLINICAL VIGNETTES A CASE BASED TEXT Department of Orthopaedic Surgery, RCSI Department of General Practice, RCSI Department of Rheumatology, Beaumont Hospital O’Byrne J, Downey R, Feeley R, Kelly M, Tiedt L, O’Byrne J, Murphy M, Stuart E, Kearns G. (2019) Musculoskeletal clinical vignettes: a case based text. Dublin, Ireland: RCSI. ISBN: 978-0-9926911-8-9 Image attribution: istock.com/mashuk CC Licence by NC-SA MUSCULOSKELETAL CLINICAL VIGNETTES Incorporating history, examination, investigations and management of commonly presenting musculoskeletal conditions 1131 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey Prof. John O'Byrne Mr. Iain Feeley Dr. Richie Downey Dr. Martin Kelly Mr. Iain Feeley Dr. Lauren Tiedt Dr. Martin Kelly Department of General Practice, RCSI Dr. Lauren Tiedt Dr. Mark Murphy Department of General Practice, RCSI Dr Ellen Stuart Dr. Mark Murphy Department of Rheumatology, Beaumont Hospital Dr Ellen Stuart Dr Grainne Kearns Department of Rheumatology, Beaumont Hospital Dr Grainne Kearns 2 2 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey TABLE OF CONTENTS Prof. John O'Byrne Mr. Iain Feeley Introduction ............................................................. 5 Dr. Richie Downey Dr. Martin Kelly General guidelines for musculoskeletal physical Mr. Iain Feeley examination of all joints .................................................. 6 Dr. Lauren Tiedt Dr. Martin Kelly Upper limb ............................................................. 10 Department of General Practice, RCSI Example of an upper limb joint examination ................. 11 Dr. Lauren Tiedt Shoulder osteoarthritis ................................................. 13 Dr. Mark Murphy Adhesive capsulitis (frozen shoulder) ............................ 16 Department of General Practice, RCSI Dr Ellen Stuart Shoulder rotator cuff pathology ................................... -

Mcmaster Musculoskeletal Clinical Skills Manual 1E
McMaster Musculoskeletal Clinical Skills Manual Authors Samyuktha Adiga Dr. Raj Carmona, MBBS, FRCPC Illustrator Jenna Rebelo Editors Caitlin Lees Dr. Raj Carmona, MBBS, FRCPC In association with the Medical Education Interest Group Narendra Singh and Jacqueline Ho (co-chairs) FOREWORD AND ACKNOWLEDGEMENTS The McMaster Musculoskeletal Clinical Skills Manual was produced by members of the Medical Education Interest Group (co-chairs Jacqueline Ho and Narendra Singh), and Dr. Raj Carmona, Assistant Professor of Medicine at McMaster University. Samyuktha Adiga and Dr. Carmona wrote the manual. Illustrations were done by Jenna Rebelo. Editing was performed by Caitlin Lees and Dr. Carmona. The Manual, completed in August 2012, is a supplement to the McMaster MSK Examination Video Series created by Dr. Carmona, and closely follows the format and content of these videos. The videos are available on Medportal (McMaster students), and also publicly accessible at RheumTutor.com and fhs.mcmaster.ca/medicine/rheumatology. McMaster Musculoskeletal Clinical Skills Manual S. Adiga, J. Rebelo, C. Lees, R. Carmona McMaster Musculoskeletal Clinical Skills Manual TABLE OF CONTENTS General Guide 1 Hip Examination 3 Knee Examination 6 Ankle and Foot Examination 12 Examination of the Back 15 Shoulder Examination 19 Elbow Examination 24 Hand and Wrist Examination 26 Appendix: Neurological Assessment 29 1 GENERAL GUIDE (Please see videos for detailed demonstration of examinations) Always wash your hands and then introduce yourself to the patient. As with any other exam, ensure adequate exposure while respecting patient's modesty. Remember to assess gait whenever doing an examination of the back or any part of the lower limbs. Inspection follows the format: ● S welling ● E rythema ● A trophy ● D eformities ● S cars, skin changes, etc. -

Clinical Examination of the Wrist TERRI M
Clinical Examination of the Wrist TERRI M. SKIRVEN, OTR/L, CHT AND A. LEE OSTERMAN, MD HISTORY OF THE INJURY OR ONSET PHYSICAL EXAMINATION INSPECTION OF THE WRIST GENERAL TESTS OBJECTIVE ASSESSMENTS SUMMARY DIAGNOSTIC INJECTION CRITICAL POINTS The wrist is a highly complex joint in a very compact space . Successful clinical evaluation of the wrist requires a 1. Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and thorough knowledge of wrist anatomy, biomechanics, pathology. Also required is knowledge of surface anatomy and pathology . and the corresponding underlying structures . The keys to a 2. The wrist examination includes a complete history, successful examination are to link the symptoms with the visual inspection, objective assessments, and a underlying palpable structures and to correlate the mecha- systematic physical examination, including palpation nism of the injury with the physical findings . Some common and provocative testing . conditions may be easily identified on the basis of the clinical 3. The keys to a successful examination are to link the examination, whereas others may require additional diagnos- symptoms with the underlying palpable structures and tic studies, imaging, and repeat evaluations . to correlate the mechanism of the injury with the The components of the wrist examination include a thor- physical findings . ough history, visual inspection, objective assessments, and a 4. Before the wrist is examined, a careful inspection of the systematic physical examination, including palpation and entire upper extremity should be performed to rule out provocative testing to identify tenderness and abnormal other extrinsic and more proximal causes for the wrist motion between bones. -

Mcqs and Emqs in Surgery
1 The metabolic response to injury Multiple choice questions ➜ Homeostasis B Every endocrine gland plays an equal 1. Which of the following statements part. about homeostasis are false? C They produce a model of several phases. A It is defined as a stable state of the D The phases occur over several days. normal body. E They help in the process of repair. B The central nervous system, heart, lungs, ➜ kidneys and spleen are the essential The recovery process organs that maintain homeostasis at a 4. With regard to the recovery process, normal level. identify the statements that are true. C Elective surgery should cause little A All tissues are catabolic, resulting in repair disturbance to homeostasis. at an equal pace. D Emergency surgery should cause little B Catabolism results in muscle wasting. disturbance to homeostasis. C There is alteration in muscle protein E Return to normal homeostasis after breakdown. an operation would depend upon the D Hyperalimentation helps in recovery. presence of co-morbid conditions. E There is insulin resistance. ➜ Stress response ➜ Optimal perioperative care 2. In stress response, which of the 5. Which of the following statements are following statements are false? true for optimal perioperative care? A It is graded. A Volume loss should be promptly treated B Metabolism and nitrogen excretion are by large intravenous (IV) infusions of related to the degree of stress. fluid. C In such a situation there are B Hypothermia and pain are to be avoided. physiological, metabolic and C Starvation needs to be combated. immunological changes. D Avoid immobility. D The changes cannot be modified. -

Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee
To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. S E C T I O N X Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee 31-1 Author: Noyes; Noyes_Section X_main.indd 1 9/23/2015 5:53:34 PM To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. 31 c00031 Knee Articular Cartilage Restoration Procedures Joshua D. Harris, MD, Brian J. Cole, MD, MBA OUTLINE u0010 Indications, 31-2 Preoperative Planning, 31-7 u0045 u0015 Contraindications, 31-4 Intraoperative Evaluation and Operative Technique, 31-8 u0050 u0020 Clinical Biomechanics, 31-4 Clinical Outcomes, 31-9 u0055 u0025 Clinical Evaluation, 31-5 u0030 History, 31-5 u0035 Physical Examination, 31-6 u0040 Diagnostic Tests, 31-7 Once the determination that a defect is symptomatic has p0120 s0010 INDICATIONS been made, conservative treatment options may commence. These Management of symptomatic focal chondral and osteochondral include, but are not limited to, rest, activity modification (typically defects in the knee is complex and multifactorial. -

Journal Pre-Proof
Mayo Clinic Proceedings Telemedicine Musculoskeletal Examination The Telemedicine Musculoskeletal Examination Edward R. Laskowski, MD; Shelby E. Johnson, MD; Randy A. Shelerud, MD; Jason A. Lee, DO; Amy E. Rabatin, MD; Sherilyn W. Driscoll, MD; Brittany J. Moore, MD; Michael C. Wainberg, DO; Carmen M. Terzic, MD, PhD All authors listed are members of the Department of Physical Medicine and Rehabilitation, Mayo Clinic Rochester, and additionally, Dr. Laskowski and Dr. Lee are members of the Division of Sports Medicine of the Department of Orthopedics, Mayo Clinic Rochester. Corresponding Author: Edward R. Laskowski, MD Physical Medicine and Rehabilitation Mayo Clinic 200 First Street SW Rochester, MN 55905 [email protected] Abstract Telemedicine uses modern telecommunication technology to exchange medical information and provide clinical care to individuals at a distance. Initially intended to improve health care to patients in remote settings, telemedicine now has a broad clinical scope with the generalJournal purpose of providing Pre-Proofconvenient, safe, time and cost-efficient care. The Corona Virus Disease 2019 (COVID-19) pandemic has created significant nationwide changes to health care access and delivery. Elective appointments and procedures have been cancelled or delayed, and multiple states still have some degree of shelter-in-place orders. Many institutions are now relying more heavily on telehealth services to continue to provide medical care to individuals while also preserving the © 2020 Mayo Foundation for Medical Education and Research. Mayo Clin Proc. 2020;95(x):xx-xx. Mayo Clinic Proceedings Telemedicine Musculoskeletal Examination safety of healthcare professionals and patients. Telemedicine can also help reduce the surge in health care needs and visits as restrictions are lifted.