Knee Pain in Children: Part I: Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recurrent Knee Effusions in Gymnast
12-648 LC WHITE Mid Atlantic Regional Chapter of the American College of Sports Medicine Annual Scientific Meeting, November 2nd - 3rd, 2018 Conference Proceedings International Journal of Exercise Science, Issue 9, Volume 7 Recurrent Knee Effusions in Gymnast Stephanie A. Carey, Penn State Milton S. Hershey Medical Center, Hershey, PA. email: [email protected] (Sponsor: Shawn Phillips, MD) History: A 20-year-old current college freshman sustained a right knee effusion following a hyperextension injury approximately 8 years ago while participating in gymnastics. Per report, workup at the time was negative, and she returned to gymnastics. She participated in gymnastics for 2 additional years and retired due to other interests. While continuing regular exercise, and participation in marching band, she reports recurrent, intermittent right knee effusions since that time. She reports that these would occur more often with repetitive activity. Over the past few months, her knee has been more significantly and persistently swollen. She exercises often, but reports no specific inciting incident. She reports pain with end range flexion. She denies any instability or locking. Previous physical therapy has improved her pain. Physical Examination: Examination revealed significant effusion of right knee. No obvious effusions in other joints. Range of motion was normal and pain free. Negative Lachman, anterior drawer, posterior drawer, varus and valgus stress testing , patellar grind, McMurray, Thessaly. Neurovascularly intact. Differential Diagnosis: 1. Meniscal tear, 2 Infection including possible Lyme Disease or Gonococcal Infection; 3. Rheumatoid Arthritis; 4. Gout; 5. Pigmented Villonodular Synovitis; 6. Hemophilia Test and Results: Aspiration: Bloody - >10000 RBCs, no crystals, normal WBC. -
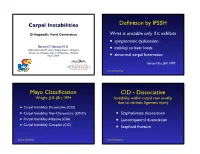
Carpal-Instability-Slide-Summary.Pdf
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

HYALURONIC ACID in KNEE OSTEOARTHRITIS Job Hermans
HYALURONIC ACID IN KNEE OSTEOARTHRITIS IN KNEE OSTEOARTHRITIS ACID HYALURONIC HYALURONIC ACID IN KNEE OSTEOARTHRITIS effectiveness and efficiency Job Hermans Job Hermans Hyaluronic Acid in Knee Osteoarthritis effectiveness and efficiency Job Hermans Part of the research described in this thesis was supported by a grant from ZonMW. Financial support for the publication of this thesis was kindly provided by: • Erasmus MC Department of Orthopaedics and Sports Medicine • Nederlandse Orthopaedische Vereniging • Anna Fonds | NOREF • Apotheekgroep Breda • Össur Eindhoven • Bioventus The e-book version of this thesis is available at www.orthopeden.org/downloads/proefschriften ISBN 978-94-6416-168-7 Coverdesign and layout: Publiss.nl Printing: Ridderprint | www.ridderprint.nl © Job Hermans 2020 All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any other information storage or retrieval system, without the prior written permission of the holder of the copyright. Hyaluronic Acid in Knee Osteoarthritis effectiveness and efficiency Hyaluronzuur bij Knieartrose effectiviteit en efficiëntie Thesis to obtain the degree of Doctor from the Erasmus University Rotterdam by command of the rector magnificus Prof.dr. R.C.M.E. Engels and in accordance with the decision of the Doctorate Board. The public defense shall be held on November 24 2020 at 13:30hrs by Job Hermans Born in Boxmeer, the Netherlands Doctoral Committee Promotors Prof.dr. S.M.A. Bierma-Zeinstra Prof.dr. J.A.N. Verhaar Other members Prof.dr. S.K. Bulstra Prof.dr. J.M.W. Hazes Prof.dr. B.W. -

Disorders of the Knee
DisordersDisorders ofof thethe KneeKnee PainPain Swelling,Swelling, effusioneffusion oror hemarthrosishemarthrosis LimitedLimited jointjoint motionmotion Screw home mechanism – pain, stiffness, fluid, muscular weakness, locking InstabilityInstability – giving way, laxity DeformityDeformity References: 1. Canale ST. Campbell’s operative orthopaedics. 10th edition 2003 Mosby, Inc. 2. Netter FH. The Netter collection of Medical illustrations – musculoskeletal system, Part I & II. 1997 Novartis Pharmaceuticals Corporation. 3. Magee DJ. Orthopedic Physical assessment. 2nd edition 1992 W. B. Saunders Company. 4. Hoppenfeld S. Physical examination of the spine and extremities. 1976 Appleton-century-crofts. AnteriorAnterior CruciateCruciate LigamentLigament Tibial insertion – broad, irregular, diamond-shaped area located directly in front of the intercondylar eminence Femoral attachment Femoral attachment Figure 43-24 In addition to their – semicircular area on the posteromedial synergistic functions, cruciate aspect of the lateral condyle and collateral ligaments exercise 33 mm in length basic antagonistic function 11 mm in diameter during rotation. A, In external Anteromedial bundle — tight in flexion rotation it is collateral ligaments that tighten and inhibit excessive Posterolateral bundle — tight in extension rotation by becoming crossed in 90% type I collagen space. B, In neutral rotation none 10% type III collagen of the four ligaments is under unusual tension. C, In internal Middle geniculate artery rotation collateral ligaments Fat -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

Adult and Adolescent Knee Pain Guideline Overview
Adult and Adolescent Knee Pain Guideline Overview This Guideline was adapted from and used with the permission of The UW Medical Foundation, UW Hospitals and Clinics, Meriter Hospital, University of Wisconsin Department of Family Medicine, Unity Health Insurance, Physicians Plus Insurance Corporation, and Group Health Cooperative, who created this guideline on May 18, 2007 as the result of a multidisciplinary work group comprised of health care practitioners from orthopedics, sports medicine, and rheumatology. This Guideline was reviewed and approved by Aspirus Network’s Medical Management Committee on May 7, 2013. The Knee Pain Work Group, a multidisciplinary work group comprised of health care practitioners from family practice, internal medicine, pediatric, and orthopedic surgery, participated in the development of this guideline. This guideline is intended to assist the patient-provider team to achieve the “Triple Aim”: quality, cost-efficient care with improved patient experiences / outcomes (i.e. do what’s best for the patient). Any distribution outside of Aspirus Network, Inc. is prohibited. Page 1 of 6 Adult and Adolescent Knee Pain Guideline Overview Guidelines are designed to assist clinicians by providing a framework for the evaluation and treatment of patients. This guideline outlines the preferred approach for most patients. It is not intended to replace a clinician’s judgment or to establish a protocol for all patients. It is understood that some patients will not fit the clinical condition contemplated by a guideline and that a guideline will rarely establish the only appropriate approach to a problem. TABLE OF CONTENTS 1. Patient Presents with Knee Pain ...................................................................... 3 2. History and Physical Exam ............................................................................. -

Pseudogout at the Knee Joint Will Frequently Occur After Hip Fracture
Harato and Yoshida Journal of Orthopaedic Surgery and Research (2015) 10:4 DOI 10.1186/s13018-014-0145-9 RESEARCH ARTICLE Open Access Pseudogout at the knee joint will frequently occur after hip fracture and lead to the knee pain in the early postoperative period Kengo Harato1,3*† and Hiroki Yoshida2† Abstract Background: Symptomatic knee joint effusion is frequently observed after hip fracture, which may lead to postoperative knee pain during rehabilitation after hip fracture surgery. However, unfortunately, very little has been reported on this phenomenon in the literature. The purpose of the current study was to investigate the relationship between symptomatic knee effusion and postoperative knee pain and to clarify the reason of the effusion accompanied by hip fracture. Methods: A total of 100 patients over 65 years of age with an acute hip fracture after fall were prospectively followed up. Knee effusion was assessed on admission and at the operating room before the surgery. If knee effusion was observed at thetimeofthesurgery,synovialfluidwascollectedintosyringes to investigate the cause of the effusion using a compensated polarized light microscope. Furthermore, for each patient, we evaluated age, sex, radiographic knee osteoarthritis (OA), type of the fracture, laterality, severity of the fracture, and postoperative knee pain during rehabilitation. These factors were compared between patients with and without knee effusion at the time of the surgery. As a statistical analysis, we used Mann–Whitney U-test for patients’ age and categorical variables were analyzed by chi-square test or Fisher’sexacttest. Results: A total of 30 patients presented symptomatic knee effusion at the time of the surgery. -

Physical Esxam
Pearls in the Musculoskeletal Exam Frank Caruso MPS, PA-C, EMT-P Skin, Bones, Hearts & Private Parts 2019 Examination Key Points • Area that needs to be examined, gown your patients - well exposed • Understand normal functional anatomy • Observe normal activity • Palpation • Range of Motion • Strength/neuro-vascular assessment • Special Tests General Exam Musculoskeletal Overview Physical Exam Preview Watch Your Patients Walk!! Inspection • Posture – Erectness – Symmetry – Alignment • Skin and subcutaneous tissues – Swelling – Redness – Masses Inspection • Extremities – Size – Deformities – Enlargement – Alignment – Contour – Symmetry Inspection • Muscles – Bilateral symmetry – Hypertrophy – Atrophy – Fasciculations – Spasms Palpation • Palpate bones, joints, and surrounding muscles for the following: – Heat – Tenderness – Swelling – Fluctuation – Crepitus – Resistance to pressure – Muscle tone Muscles • Size and strength affected by the following: – Genetics – Exercise – Nutrition • Muscles move joints through range of motion (ROM). Muscle Strength • Compare bilateral muscles – Strength – Symmetry – Equality – Resistance End Feel Think About It!! • The sensation the examiner feels in the joint as it reaches the end of the range of motion of each passive movement • Bone to bone: This is hard, unyielding – normal would be elbow extension. • Soft–tissue approximation: yielding compression that stops further movement – elbow and knee flexion. End Feel • Tissue stretch: hard – springy type of movement with a slight give – toward the end of range of motion – most common type of normal end feel : knee extension and metacarpophalangeal joint extension. Abnormal End Feel • Muscle spasm: invoked by movement with a sudden dramatic arrest of movement often accompanied by pain - sudden hard – “vibrant twang” • Capsular: Similar to tissue stretch but it does not occur where one would expect – range of motion usually reduced. -

Examination of the Knee
Examination of the Knee The Examination For every joint of the lower extremity always begin with the patient in standing IN STANDING INSPECTION 1. Cutaneous Structures: Look for Erythema, scarring, bruising, and swelling in the following areas: a. Peripatellar grooves b. Suprapatellar bursa c. Prepatellar bursa d. Infrapatellar tendon e. Anserine bursa f. Popliteal fossa 2. Muscle & Soft Tissue: a. Quadriceps atrophy b. Hamstring atrophy c. Calf atrophy 3. Bones & Alignment: a. Patella position (Alta, Baha, Winking, Frog eyed), b. Varus or Valgus alignment c. Flexion contracture or Genu recurvatum RANGE OF MOTION - ACTIVE Standing is the best opportunity to assess active range of motion of the knee. 1. Ask the patient to squat into a deep knee bend. Both knees should bend symmetrically. 2. Ask the patient to then stand and extend the knee fully – lock the knee. The knee should straighten to 0 degrees of extension. Some people have increased extension referred to as genu recurvatum. GAIT 1. Look for a short stance phase on the affected limb and an awkward gait if a concomitant leg length discrepancy 2. Look for turning on block 3. Screening 1. Walk on the toes 2. Walk on the heels 3. Squat down – Active Range of Motion testing SPECIAL TESTS 1. Leg Length Discrepancy a. Look at patients back for evidence of a functional scoliosis b. Place your hands on the patients Iliac crests looking for inequality which may mean a leg length discrepancy IN SITTING NEUROLOGIC EXAMINATION 1. Test the reflexes a. L4 – Quadriceps reflex VASCULAR EXAMINATION 1. Feel for the posterior tibial artery SUPINE POSITION INSPECTION 1. -

SIMMONDS TEST: Patient Is Prone Doctor Flexes the Patients Knee to 90 Degrees Doctor Squeezes the Patient’S Calf
Clinical Orthopedic Testing Review SIMMONDS TEST: Patient is prone Doctor flexes the patients knee to 90 degrees Doctor squeezes the patient’s calf. Classical response: Failure of ankle plantarflexion Classical Importance= torn Achilles tendon Test is done bilaterally ACHILLES TAP: Patient is prone Doctor flexes the patient’s knee to 90 degree Doctor dorsiflexes the ankle and then strikes the Achilles tendon with a percussion hammer Classical response: Plantar response Classical Importance= Intact Achilles tendon Test is done bilaterally FOOT DRAWER TEST: Patient is supine with their ankles off the edge of the examination table Doctor grasps the heel of the ankle being tested with one hand and the tibia just above the ankle with the other. Doctor applies and anterior to posterior and then a posterior to anterior sheer force. Classical response: Anterior or posterior translation of the ankle Classical Importance= Anterior talofibular or posterior talofibular ligament laxity. Test is done bilaterally LATERAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other. Doctor rotates the foot into inversion Classical response: Excessive inversion Classical Importance= Anterior talofibular ligament sprain Test is done bilaterally MEDIAL STABILITY TEST: Patient is supine Doctor grasps the tibia with one hand and the foot with the other Doctor rotates the foot into eversion Classical response: Excessive eversion Classical Importance= Deltoid ligament sprain Test is done bilaterally 1 Clinical Orthopedic Testing Review KLEIGER’S TEST: Patient is seated with the legs and feet dangling off the edge of the examination table. Doctor grasps the patient’s foot while stabilizing the tibia with the other hand Doctor pulls the ankle laterally. -

Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions
Review Article Physical Examination of the Knee: Meniscus, Cartilage, and Patellofemoral Conditions Abstract Robert D. Bronstein, MD The knee is one of the most commonly injured joints in the body. Its Joseph C. Schaffer, MD superficial anatomy enables diagnosis of the injury through a thorough history and physical examination. Examination techniques for the knee described decades ago are still useful, as are more recently developed tests. Proper use of these techniques requires understanding of the anatomy and biomechanical principles of the knee as well as the pathophysiology of the injuries, including tears to the menisci and extensor mechanism, patellofemoral conditions, and osteochondritis dissecans. Nevertheless, the clinical validity and accuracy of the diagnostic tests vary. Advanced imaging studies may be useful adjuncts. ecause of its location and func- We have previously described the Btion, the knee is one of the most ligamentous examination.1 frequently injured joints in the body. Diagnosis of an injury General Examination requires a thorough knowledge of the anatomy and biomechanics of When a patient reports a knee injury, the joint. Many of the tests cur- the clinician should first obtain a rently used to help diagnose the good history. The location of the pain injured structures of the knee and any mechanical symptoms were developed before the avail- should be elicited, along with the ability of advanced imaging. How- mechanism of injury. From these From the Division of Sports Medicine, ever, several of these examinations descriptions, the structures that may Department of Orthopaedics, are as accurate or, in some cases, University of Rochester School of have been stressed or compressed can Medicine and Dentistry, Rochester, more accurate than state-of-the-art be determined and a differential NY. -

Joint Range of Motion
JOINT RANGE OF MOTION In addition to joint integrity, adequate muscle length and other soft tissue extensibility must be The amount of motion available at a synovial joint maintained to optimize joint function.3 Most muscles is called the range of motion (ROM). Normal cross more than one joint to allow for shortening ROM varies among individuals and is influenced by over one joint and lengthening over the other during age, gender, body habitus, and whether motion is movement. However, there is potential for a muscle performed actively or passively.1 The type and amount or muscle group to become excessively lengthened of movement that occurs throughout the ROM is or shortened when it crosses more than one joint. If unique to each joint of the body and is dependent a muscle is rendered weak because it is shortened as primarily upon the shape of the articular surfaces. much as it can be as it crosses each joint, it is said to Other factors include the integrity and flexibility of be actively insufficient. An example of this occurs the periarticular soft tissues. when an individual lies prone with the hip extended Joint motion involves rotation or translation of or in neutral, and the individual is asked to perform one articular surface relative to the other about an a “leg curl” to flex the knee as much as possible. axis known as the instantaneous, helical, or screw axis. Active insufficiency occurs in the hamstrings in this Both rotation around the joint axis and translation example because they are shortened over the knee along the instantaneous axis must occur to provide and hip at the same time, and full flexion of the knee normal joint kinematics.2 Joint movements that are may be difficult.