Disorders of the Knee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Carpal-Instability-Slide-Summary.Pdf
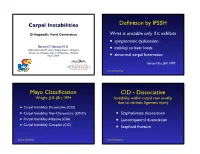
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

Examination of the Knee
Examination of the Knee The Examination For every joint of the lower extremity always begin with the patient in standing IN STANDING INSPECTION 1. Cutaneous Structures: Look for Erythema, scarring, bruising, and swelling in the following areas: a. Peripatellar grooves b. Suprapatellar bursa c. Prepatellar bursa d. Infrapatellar tendon e. Anserine bursa f. Popliteal fossa 2. Muscle & Soft Tissue: a. Quadriceps atrophy b. Hamstring atrophy c. Calf atrophy 3. Bones & Alignment: a. Patella position (Alta, Baha, Winking, Frog eyed), b. Varus or Valgus alignment c. Flexion contracture or Genu recurvatum RANGE OF MOTION - ACTIVE Standing is the best opportunity to assess active range of motion of the knee. 1. Ask the patient to squat into a deep knee bend. Both knees should bend symmetrically. 2. Ask the patient to then stand and extend the knee fully – lock the knee. The knee should straighten to 0 degrees of extension. Some people have increased extension referred to as genu recurvatum. GAIT 1. Look for a short stance phase on the affected limb and an awkward gait if a concomitant leg length discrepancy 2. Look for turning on block 3. Screening 1. Walk on the toes 2. Walk on the heels 3. Squat down – Active Range of Motion testing SPECIAL TESTS 1. Leg Length Discrepancy a. Look at patients back for evidence of a functional scoliosis b. Place your hands on the patients Iliac crests looking for inequality which may mean a leg length discrepancy IN SITTING NEUROLOGIC EXAMINATION 1. Test the reflexes a. L4 – Quadriceps reflex VASCULAR EXAMINATION 1. Feel for the posterior tibial artery SUPINE POSITION INSPECTION 1. -

Knee Pain in Children: Part I: Evaluation
Knee Pain in Children: Part I: Evaluation Michael Wolf, MD* *Pediatrics and Orthopedic Surgery, St Christopher’s Hospital for Children, Philadelphia, PA. Practice Gap Clinicians who evaluate knee pain must understand how the history and physical examination findings direct the diagnostic process and subsequent management. Objectives After reading this article, the reader should be able to: 1. Obtain an appropriate history and perform a thorough physical examination of a patient presenting with knee pain. 2. Employ an algorithm based on history and physical findings to direct further evaluation and management. HISTORY Obtaining a thorough patient history is crucial in identifying the cause of knee pain in a child (Table). For example, a history of significant swelling without trauma suggests bacterial infection, inflammatory conditions, or less likely, intra- articular derangement. A history of swelling after trauma is concerning for potential intra-articular derangement. A report of warmth or erythema merits consideration of bacterial in- fection or inflammatory conditions, and mechanical symptoms (eg, lock- ing, catching, instability) should prompt consideration of intra-articular derangement. Nighttime pain and systemic symptoms (eg, fever, sweats, night sweats, anorexia, malaise, fatigue, weight loss) are associated with bacterial infections, inflammatory conditions, benign and malignant musculoskeletal tumors, and other systemic malignancies. A history of rash or known systemic inflammatory conditions, such as systemic lupus erythematosus or inflammatory bowel disease, should raise suspicion for inflammatory arthritis. Ascertaining the location of the pain also can aid in determining the cause of knee pain. Anterior pain suggests patellofemoral syndrome or instability, quad- riceps or patellar tendinopathy, prepatellar bursitis, or apophysitis (patellar or tibial tubercle). -

Mcmaster Musculoskeletal Clinical Skills Manual 1E
McMaster Musculoskeletal Clinical Skills Manual Authors Samyuktha Adiga Dr. Raj Carmona, MBBS, FRCPC Illustrator Jenna Rebelo Editors Caitlin Lees Dr. Raj Carmona, MBBS, FRCPC In association with the Medical Education Interest Group Narendra Singh and Jacqueline Ho (co-chairs) FOREWORD AND ACKNOWLEDGEMENTS The McMaster Musculoskeletal Clinical Skills Manual was produced by members of the Medical Education Interest Group (co-chairs Jacqueline Ho and Narendra Singh), and Dr. Raj Carmona, Assistant Professor of Medicine at McMaster University. Samyuktha Adiga and Dr. Carmona wrote the manual. Illustrations were done by Jenna Rebelo. Editing was performed by Caitlin Lees and Dr. Carmona. The Manual, completed in August 2012, is a supplement to the McMaster MSK Examination Video Series created by Dr. Carmona, and closely follows the format and content of these videos. The videos are available on Medportal (McMaster students), and also publicly accessible at RheumTutor.com and fhs.mcmaster.ca/medicine/rheumatology. McMaster Musculoskeletal Clinical Skills Manual S. Adiga, J. Rebelo, C. Lees, R. Carmona McMaster Musculoskeletal Clinical Skills Manual TABLE OF CONTENTS General Guide 1 Hip Examination 3 Knee Examination 6 Ankle and Foot Examination 12 Examination of the Back 15 Shoulder Examination 19 Elbow Examination 24 Hand and Wrist Examination 26 Appendix: Neurological Assessment 29 1 GENERAL GUIDE (Please see videos for detailed demonstration of examinations) Always wash your hands and then introduce yourself to the patient. As with any other exam, ensure adequate exposure while respecting patient's modesty. Remember to assess gait whenever doing an examination of the back or any part of the lower limbs. Inspection follows the format: ● S welling ● E rythema ● A trophy ● D eformities ● S cars, skin changes, etc. -

Clinical Examination of the Wrist TERRI M
Clinical Examination of the Wrist TERRI M. SKIRVEN, OTR/L, CHT AND A. LEE OSTERMAN, MD HISTORY OF THE INJURY OR ONSET PHYSICAL EXAMINATION INSPECTION OF THE WRIST GENERAL TESTS OBJECTIVE ASSESSMENTS SUMMARY DIAGNOSTIC INJECTION CRITICAL POINTS The wrist is a highly complex joint in a very compact space . Successful clinical evaluation of the wrist requires a 1. Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and thorough knowledge of wrist anatomy, biomechanics, pathology. Also required is knowledge of surface anatomy and pathology . and the corresponding underlying structures . The keys to a 2. The wrist examination includes a complete history, successful examination are to link the symptoms with the visual inspection, objective assessments, and a underlying palpable structures and to correlate the mecha- systematic physical examination, including palpation nism of the injury with the physical findings . Some common and provocative testing . conditions may be easily identified on the basis of the clinical 3. The keys to a successful examination are to link the examination, whereas others may require additional diagnos- symptoms with the underlying palpable structures and tic studies, imaging, and repeat evaluations . to correlate the mechanism of the injury with the The components of the wrist examination include a thor- physical findings . ough history, visual inspection, objective assessments, and a 4. Before the wrist is examined, a careful inspection of the systematic physical examination, including palpation and entire upper extremity should be performed to rule out provocative testing to identify tenderness and abnormal other extrinsic and more proximal causes for the wrist motion between bones. -

Abdominal Distension
2003 OSCE Handbook The world according to Kelly, Marshall, Shaw and Tripp Our OSCE group, like many, laboured away through 5th year preparing for the OSCE exam. The main thing we learnt was that our time was better spent practising our history taking and examination on each other, rather than with our noses in books. We therefore hope that by sharing the notes we compiled you will have more time for practice, as well as sparing you the trauma of feeling like you‟ve got to know everything about everything on the list. You don‟t! You can‟t swot for an OSCE in a library! This version is the same as the 2002 OSCE Handbook, except for the addition of the 2002 OSCE stations. We have used the following books where we needed reference material: th Oxford Handbook of Clinical Medicine, 4 Edition, R A Hope, J M Longmore, S K McManus and C A Wood-Allum, Oxford University Press, 1998 Oxford Handbook of Clinical Specialties, 5th Edition, J A B Collier, J M Longmore, T Duncan Brown, Oxford University Press, 1999 N J Talley and S O‟Connor, Clinical Examination – a Systematic Guide to Physical Diagnosis, Third Edition, MacLennan & Petty Pty Ltd, 1998 J. Murtagh, General Practice, McGraw-Hill, 1994 These are good books – buy them! Warning: This document is intended to help you cram for your OSEC. It is not intended as a clinical reference, and should not be used for making real life decisions. We‟ve done our best to be accurate, but don‟t accept any responsibility for exam failure as a result of bloopers…. -

Spine to Move Mobile Lumbar Spine 7) Cauda Equina Syndrome
13rd EDITION by Anika A Alhambra PERIPHERAL NERVE INJURY SEDDON classification: I. NEUROPRAXIA. − Transient disorder (spontan recovery), several weeks. − EMG of the distal lession usually normal. − Caused by mechanical pressure, exp: − Crutch paralysis − Good prognosis. II. AXONOTMESIS − A discontinuity of the axon, with intact endoneurium. − Wallerian degenration on the distal side. − There is an axon regeneration : 1 – 3 mm/day − Good prognosis III. NEUROTMESIS − Nerve trunk has distrupted, include endoneural tube − Regeneration process Æ neuroma − Prognosis: depend on the surgery technique. SUNDERLAND Classifications: I. Loss of axonal conduction. II. Loss of continuity of the axon, with intact endoneurium. III. Transection of nerve fiber (axon & sheath), with intact perineurium. IV. Loss of perineurium and fascicular continuity. V. Loss of continuity of entire nerve trunk. DEGREE DISCONTINUITY DAMAGE TREATMENT PROGNOSIS 1st None, conduction block Distal nerve fibers Observation Excellent (neuroprxia) remain intact 2nd Axon (axonotmesis) Based on fibrosis Observation Good 3rd Axon & endoneurium Based on fibrosis Lysis Ok 4th Axon, Fibrotic Nerve graft Marginal endoneurium,perineurium connective tissue connects 5th Complete (neurotmesis) Complete Graft/transfer Poor PATOPHYSIOLOGY on the nerve compression injury: 23rd EDITION by Anika A Alhambra 1. Disturb to microcirculation Æ ischemia 2. Disturb to axoplasmic transport Æ neruroaxonal transport Intravascular edema (Increase of vascular permeability) (Degeneration process) Proliferating fibroblast Separation nerve fiber One week (Demyelination) Note: compression 20-30 mmHg Æ pathology on epineurium >80 mmHg Æ completely stop 30 mmHg (8j); 50 mmHg (2j) Æ reverse after 24 hours 400 mmHg (2j) Æ reverse after 1 week ‘Tinnel sign’, is happened on injury and compression, it is sign of regeneration process (continuity sign) Pathological changes on ‘PRIMARY NERVE REPAIR’ 1. -

Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee
To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. S E C T I O N X Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee 31-1 Author: Noyes; Noyes_Section X_main.indd 1 9/23/2015 5:53:34 PM To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. 31 c00031 Knee Articular Cartilage Restoration Procedures Joshua D. Harris, MD, Brian J. Cole, MD, MBA OUTLINE u0010 Indications, 31-2 Preoperative Planning, 31-7 u0045 u0015 Contraindications, 31-4 Intraoperative Evaluation and Operative Technique, 31-8 u0050 u0020 Clinical Biomechanics, 31-4 Clinical Outcomes, 31-9 u0055 u0025 Clinical Evaluation, 31-5 u0030 History, 31-5 u0035 Physical Examination, 31-6 u0040 Diagnostic Tests, 31-7 Once the determination that a defect is symptomatic has p0120 s0010 INDICATIONS been made, conservative treatment options may commence. These Management of symptomatic focal chondral and osteochondral include, but are not limited to, rest, activity modification (typically defects in the knee is complex and multifactorial. -

Knee Injury Medical Treatment Guidelines©
Knee Injury Medical Treatment Guidelines© Proposed by the State of New York Department of Insurance to the Workers’ Compensation Board ©Algorithm 1 and Tables 1 and 2 are taken from the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints published and copyrighted by the American College of Occupational and Environmental Medicine. Copyright 2008, 2007, 2004, 1997 by the American College of Occupational and Environmental Medicine (ACOEM). Commercial reproduction or other use beyond fair use prohibited without explicit ACOEM permission. The American College of Occupational and Environmental Medicine has granted the Workers’ Compensation Board permission to publish Algorithm 1 and Tables 1 and 2 of the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints in connection with the adoption of the New York Knee Injury Medical Treatment Guidelines, including making this guideline available in print and on its website for informational and educational purposes. Use of Algorithm 1 and Tables 1 and 2 of this guideline beyond fair use or for commercial purpose, or both may only occur upon receipt of explicit permission from ACOEM. December 2007 Draft Knee Injury Medical Treatment Guidelines TABLE OF CONTENTS SECTION DESCRIPTION PAGE A. INITIAL DIAGNOSTIC PROCEDURES............................................................ 1. HISTORY-TAKING AND PHYSICIAL EXAMINATION (Hx & PE) .......... a. History of Present Injury ......................................................................... b. Past History ........................................................................................... -

Grafts in Rhinoplasty
Al - Azhar University Center for Virus Studies and Research Grafts in Rhinoplasty Mohamed Rashad Abdel-Hady1, Olfat Abdel-Aziz Sayed2 and Khaled Mohamed Ahmed Abdel-Rahman3 [email protected], [email protected] and [email protected] 1. Prof. of Otolaryngology, Faculty of medicine, Al-Azhar University. 2. Ass.Prof. of Otolaryngology, Faculty of medicine, Al- Azhar University. 3 Specialist of otolaryngology, Helwan University Hospital. Abstract Old rhinoplasty practice has been often relied on resection of the nasal framework in order to achieve aesthetic and/ or functional objectives. Nowadays, careful dissection, conservative resection, planned framework remodeling, & judicious use of properly selected grafts for augmentation comprise the basis for a structural approach to grafting in rhinoplasty. Aim of the work is to present and evaluate outcomes of using grafts in rhinoplasty. Grafts types, techniques were reviewed. Complications, if encountered, were mentioned. Patient satisfaction was evaluated. Methodology is a prospective study utilized the open rhinoplasty technique, upon 35 patients that suffered from various nasal deformities. Their ages ranged between 18 and 45 years. The followed principles consisted of: 1) A precise definition of the type and cause of abnormality. 2) Definition of the goals. 3) Adequate exposure. 4) Preservation or restoration of normal anatomy 5) Incremental and planned correction. 6) Maintenance of nasal airway. Results are 35 patients operated by the open technique, 23 were males while 12 were females. Of them, 32 cases were fully corrected while, 3 cases were partially corrected. Complications were minimal, occurred in 3 cases. The majority of cases (32 cases) were satisfied while 3 cases were unsatisfied. -

Rheumatology and Rehabilitation
Basics of Rheumatology and Rehabilitation STAFF OF Rheumatology and Rehabilitation Department Mansoura Faculty of Medicine 2020- 2021 1 Preface This book is written by the staff members of Rheumatology, Physical Medicine and Rehabilitation Department, Faculty of Medicine, Mansoura University. It has been made to provide, in brief, the basic knowledge of this specialty in a systemic, concisely written, well- illustrated and comprehensive manner to be easily memorized by the undergraduate students. We hope that this book provides our students with adequate basic rheumatological knowledge to make accurate clinical observations, arrive at a diagnosis and be aware of relevant differential diagnosis. We hope that this book can also provide our students with different modalities of physical medicine and role of interdisciplinary rehabilitation program in different medical conditions. Also we hope that this book will be beneficial to general practitioner helping them to diagnose and manage some medical disease with rheumatological manifestation (how to deal with! And when to consult!). STAFF OF Rheumatology and Rehabilitation Department Mansoura Faculty of Medicine 2 STAFF MEMBERS of Rheumatology, Physical Medicine and Rehabilitation Department Faculty of Medicine Mansoura University Prof. Mona Mohsen Dr. Reham Magdy Prof. Atif El.Ghaweet Dr. Rehab Abd-Elraof Prof. Seif Eldein Farag Dr. Abeer Fekry Prof. Amir Abd-Elrahman Dr. Amany El.Bahnasawy Prof. Salah Hawas Dr. Iman Abd-Elrazik Prof. Ibraheem El.Boghdady Dr. Ola Gharbia Prof. Basma El.Kady Dr. Sherein Gaafar Prof. Manal Awad Dr. Yasmin Adel Prof. Adel Abd-Elsalam Dr. Eman Bakr Prof. Abd-Elmoety Afify Dr. Dena Abdel Ghafar Prof. Mohammed Kamal Dr. Doaa Mosaad Prof.