Uploads/NCLEX Test.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Improving the Quality of Life of the Elderly and Disabled
IMPROVING THE QUALITY OF LIFE OF THE ELDERLY AND DISABLED PEOPLE IN HUMAN SETTLEMENTS IMPROVING THE QUALITY OF LIFE OF ELDERLY AND DISABLED PEOPLE IN HUMAN SETTLEMENTS VOLUME I A Resource Book of Policy and Programmes from around the World United Nations Centre for Human Settlements (Habitat) Nairobi, 1993 HS/284/93E ISBN 92-1-131208-6 FOREWORD The world's population is ageing dramatically. The total number of people aged 60 and older grew from 200 million in 1950 to 400 million in 1982. Their number is expected to increase to 600 million in the year 2001 when 70 per cent of them will live in developing countries. This demographic revolution has major consequences on the way human settlements are designed, managed and used. The United Nations and its agencies have undertaken many activities that recognize this reality. The General Assembly adopted the World Programme of Action concerning Disabled Persons and proclaimed 1981 the International Year of Disabled Persons. In 1982, 124 Member States adopted the International Plan of Action on Aging at the World Assembly on Aging. These two landmark events launched a variety of activities and studies during the United Nations Decade of Elderly and Disabled Persons. The United Nations Centre for Human Settlements (Habitat) launched the decade with two important documents. Designing with Care - a Guide to Adaptation of the Built Environment for Disabled Persons was published as the result of cooperation between the United Nations, UNCHS (Habitat) and the Swedish International Development Agency (SIDA). This guide pointed out that implementation of suggested design guidelines and related policies and programmes would have to be undertaken by authorities, taking into consideration the economic, social and climatic conditions of the human settlement concerned. -
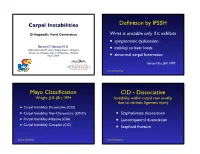
Carpal-Instability-Slide-Summary.Pdf
Carpal Instabilities Definition by IFSSH Orthopaedic Hand Conference Wrist is unstable only if it exhibits • symptomatic dysfunction Bernard F. Hearon, M.D. inability to bear loads Clinical Assistant Professor, Department of Surgery • University of Kansas School of Medicine - Wichita May 7, 2019 • abnormal carpal kinematics Garcia-Elias, JHS 1999 Carpal Instability Mayo Classification CID - Dissociative Wright, JHS (Br) 1994 Instability within carpal row usually due to intrinsic ligament injury • Carpal Instability Dissociative (CID) • Carpal Instability Non-Dissociative (CIND) • Scapholunate dissociation • Carpal Instability Adaptive (CIA) • Lunotriquetral dissociation • Carpal Instability Complex (CIC) • Scaphoid fracture Carpal Instability Carpal Instability CIND - Nondissociative Instability between carpal rows due CIA - Adaptive to extrinsic ligament injury Extra-carpal derangement causing carpal malalignment • CIND - Volar Intercalated Segment Instability (VISI) Midcarpal instability caused by malunited • CIND - Dorsal Intercalated fractures of the distal radius Segment Instability (DISI) Taleisnik, JHS 1984 • Combined CIND Carpal Instability Carpal Instability CIC - Complex Instability patterns with qualities of both CID and CIND patterns • Dorsal perilunate dislocations (lesser arc) Perilunate • Dorsal perilunate fracture-dislocations (greater arc injuries) Instability • Volar perilunate dislocations • Axial dislocations, fracture-dislocations Carpal Instability Carpal Instability Perilunate Dislocations Mayfield Classification Progressive -

Disorders of the Knee
DisordersDisorders ofof thethe KneeKnee PainPain Swelling,Swelling, effusioneffusion oror hemarthrosishemarthrosis LimitedLimited jointjoint motionmotion Screw home mechanism – pain, stiffness, fluid, muscular weakness, locking InstabilityInstability – giving way, laxity DeformityDeformity References: 1. Canale ST. Campbell’s operative orthopaedics. 10th edition 2003 Mosby, Inc. 2. Netter FH. The Netter collection of Medical illustrations – musculoskeletal system, Part I & II. 1997 Novartis Pharmaceuticals Corporation. 3. Magee DJ. Orthopedic Physical assessment. 2nd edition 1992 W. B. Saunders Company. 4. Hoppenfeld S. Physical examination of the spine and extremities. 1976 Appleton-century-crofts. AnteriorAnterior CruciateCruciate LigamentLigament Tibial insertion – broad, irregular, diamond-shaped area located directly in front of the intercondylar eminence Femoral attachment Femoral attachment Figure 43-24 In addition to their – semicircular area on the posteromedial synergistic functions, cruciate aspect of the lateral condyle and collateral ligaments exercise 33 mm in length basic antagonistic function 11 mm in diameter during rotation. A, In external Anteromedial bundle — tight in flexion rotation it is collateral ligaments that tighten and inhibit excessive Posterolateral bundle — tight in extension rotation by becoming crossed in 90% type I collagen space. B, In neutral rotation none 10% type III collagen of the four ligaments is under unusual tension. C, In internal Middle geniculate artery rotation collateral ligaments Fat -

Analysis of Rehabilitation Procedure Following Arthroplasty of the Knee with the Use of Complete Endoprosthesis
© Med Sci Monit, 2011; 17(3): CR165-168 WWW.MEDSCIMONIT.COM PMID: 21358604 Clinical Research CR Received: 2010.10.01 Accepted: 2010.12.23 Analysis of rehabilitation procedure following Published: 2011.03.01 arthroplasty of the knee with the use of complete endoprosthesis Authors’ Contribution: Magdalena Wilk-Frańczuk¹,²ACDEF, Wiesław Tomaszewski3ACDEF, Jerzy Zemła²ABDEF, A Study Design Henryk Noga4DEF, Andrzej Czamara3ADEF B Data Collection C Statistical Analysis 1 Andrzej Frycz Modrzewski Cracow University, Cracow, Poland D Data Interpretation 2 Cracow Rehabilitation Centre, Cracow, Poland E Manuscript Preparation 3 College of Physiotherapy, Wroclaw, Poland F Literature Search 4 Endoscopic Surgery Clinic and Sport Clinic Żory, Żory, Poland G Funds Collection Source of support: Departmental sources Summary Background: The use of endoprosthesis in arthroplasty requires adaptation of rehabilitation procedures in or- der to reinstate the correct model of gait, which enables the patient to recover independence and full functionality in everyday life, which in turn results in an improvement in the quality of life. Material/Methods: We studied 33 patients following an initial total arthroplasty of the knee involving endoprosthesis. The patients were divided into two groups according to age. The range of movement within the knee joints was measured for all patients, along with muscle strength and the subjective sensation of pain on a VAS, and the time required to complete the ‘up and go’ test was measured. The gait model and movement ability were evaluated. The testing was conducted at baseline and after com- pletion of the rehabilitation exercise cycle. Results: No significant differences were noted between the groups in the tests of the range of movement in the operated joint or muscle strength acting on the knee joint. -

Knee Pain in Children: Part I: Evaluation
Knee Pain in Children: Part I: Evaluation Michael Wolf, MD* *Pediatrics and Orthopedic Surgery, St Christopher’s Hospital for Children, Philadelphia, PA. Practice Gap Clinicians who evaluate knee pain must understand how the history and physical examination findings direct the diagnostic process and subsequent management. Objectives After reading this article, the reader should be able to: 1. Obtain an appropriate history and perform a thorough physical examination of a patient presenting with knee pain. 2. Employ an algorithm based on history and physical findings to direct further evaluation and management. HISTORY Obtaining a thorough patient history is crucial in identifying the cause of knee pain in a child (Table). For example, a history of significant swelling without trauma suggests bacterial infection, inflammatory conditions, or less likely, intra- articular derangement. A history of swelling after trauma is concerning for potential intra-articular derangement. A report of warmth or erythema merits consideration of bacterial in- fection or inflammatory conditions, and mechanical symptoms (eg, lock- ing, catching, instability) should prompt consideration of intra-articular derangement. Nighttime pain and systemic symptoms (eg, fever, sweats, night sweats, anorexia, malaise, fatigue, weight loss) are associated with bacterial infections, inflammatory conditions, benign and malignant musculoskeletal tumors, and other systemic malignancies. A history of rash or known systemic inflammatory conditions, such as systemic lupus erythematosus or inflammatory bowel disease, should raise suspicion for inflammatory arthritis. Ascertaining the location of the pain also can aid in determining the cause of knee pain. Anterior pain suggests patellofemoral syndrome or instability, quad- riceps or patellar tendinopathy, prepatellar bursitis, or apophysitis (patellar or tibial tubercle). -

DOCUMENT RESUME Essential Skills for the Care Team. A
DOCUMENT RESUME ED 419 937 CE 076 574 TITLE Essential Skills for the Care Team. A Program for New Employees in Residential and Home Care. INSTITUTION State Univ. of New York, Albany. Rockefeller Coll.; Eddy/Northeast Health, Troy, NY. SPONS AGENCY Office of Vocational and Adult Education (ED), Washington, DC. National Workplace Literacy Program. PUB DATE 1998-00-00 NOTE 456p.; For a related document, see CE 076 575. CONTRACT V198A40098-96 PUB TYPE GuideS Classroom Teacher (052) EDRS PRICE MF01/PC19 Plus Postage. DESCRIPTORS Adult Basic Education; Allied Health Occupations Education; Classroom Techniques; Competence; Competency Based Education; *Home Health Aides; *Nurses Aides; *On the Job Training; Postsecondary Education; Teaching Methods; Units of Study; *Workplace Literacy ABSTRACT This document contains modules for two types of training. It provides 20 hours of training to newly hired Nursing Assistant Trainees (NATs) in residential care settings preparing to become state Certified Nursing Assistants (CNAs), using eight stand-alone modules supported by training process guides. It also includes 7 hours of training for newly hired NATs in the home care settings preparing to become state certified Home Health Aides (HHAs), using five stand-alone modules with training process guides. The materials are suitable for workplace literacy programs for adults with low levels of English literacy skills. A learning strategies module serves as an introduction to both programs. The CNA program contains the following modules: understanding your -

Clinical Examination of the Wrist TERRI M
Clinical Examination of the Wrist TERRI M. SKIRVEN, OTR/L, CHT AND A. LEE OSTERMAN, MD HISTORY OF THE INJURY OR ONSET PHYSICAL EXAMINATION INSPECTION OF THE WRIST GENERAL TESTS OBJECTIVE ASSESSMENTS SUMMARY DIAGNOSTIC INJECTION CRITICAL POINTS The wrist is a highly complex joint in a very compact space . Successful clinical evaluation of the wrist requires a 1. Successful clinical examination of the wrist requires a thorough knowledge of wrist anatomy, biomechanics, and thorough knowledge of wrist anatomy, biomechanics, pathology. Also required is knowledge of surface anatomy and pathology . and the corresponding underlying structures . The keys to a 2. The wrist examination includes a complete history, successful examination are to link the symptoms with the visual inspection, objective assessments, and a underlying palpable structures and to correlate the mecha- systematic physical examination, including palpation nism of the injury with the physical findings . Some common and provocative testing . conditions may be easily identified on the basis of the clinical 3. The keys to a successful examination are to link the examination, whereas others may require additional diagnos- symptoms with the underlying palpable structures and tic studies, imaging, and repeat evaluations . to correlate the mechanism of the injury with the The components of the wrist examination include a thor- physical findings . ough history, visual inspection, objective assessments, and a 4. Before the wrist is examined, a careful inspection of the systematic physical examination, including palpation and entire upper extremity should be performed to rule out provocative testing to identify tenderness and abnormal other extrinsic and more proximal causes for the wrist motion between bones. -

Eating Disorders
What to Expect… Medical Stabilization Program for Eating Disorders CHOC has developed a multidisciplinary approach in the treatment of acute medical instability related to eating disorders. Admission is designed to: Assess and treat medical disorders resulting from abnormal eating. Provide nutritional rehabilitation Prevent long-term and life threatening complications The patient’s stay depends on the level of medical instability. Once medically stable, we will help facilitate treatment arrangements to continue treatment for the eating disorder following discharge. Treatment includes: Complete physical examination and laboratory testing Individualized medical treatment plan including vitamin and mineral supplements Cardio-respiratory monitoring Nutritional assessment and management Growth and development evaluation Psychological evaluation and monitoring Psychiatric medication evaluation and monitoring as needed What to expect during hospitalization: Patients will receive one-to-one supervision of activity at all times, including meals and snacks and bathroom privileges. Visitors limited to parents, unless otherwise authorized by the multidisciplinary team. Activity level based on vitals o Strict medical bedrest: complete bedrest with commode at bedside. May stand only for daily weight and vitals; sit in chair for linen change; bed bath only, no shower. o Bedrest with wheelchair privileges: If vital signs stable, may be pushed in a wheelchair by staff on the floor; may take seated shower, use toilet in bathroom, sit at sink. o Bedrest with ambulation privileges – may use toilet in bathroom and may shower. If vital signs stable, may be pushed in a wheelchair by staff on the floor and may be up in room for short periods, otherwise on bedrest. Outside foods are not allowed unless approved by Nutrition. -

Cruising Game Space
CRUISING GAME SPACE Game Level Design, Gay Cruising and the Queer Gothic in The Rawlings By Tommy Ting A thesis exhibition presented to OCAD University in partial fulfillment of the requirements for the degree of Master of Fine Arts in Digital Futures Toronto Media Arts Centre 32 Lisgar Street., April 12, 13, 14 Toronto, Ontario, Canada April 2019 Tommy Ting 2019 This work is licensed under the Creative Commons Attribution-Non Commercial-ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc- sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. Copyright Notice Author’s Declaration This work is licensed under the Creative Commons Attribution-NonCommercial- ShareAlike 4.0 International License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/ or send a letter to Creative Commons, 444 Castro Street, Suite 900, Mountain View, California, 94041, USA. You are free to: Share – copy and redistribute the material in any medium or format Adapt – remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms. Under the follower terms: Attribution – You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use. NonCommericial – You may not use the material for commercial purposes. ShareAlike – If you remix, transform, or build upon the material, you must distribute you contributions under the same license as the original. -

Spine to Move Mobile Lumbar Spine 7) Cauda Equina Syndrome
13rd EDITION by Anika A Alhambra PERIPHERAL NERVE INJURY SEDDON classification: I. NEUROPRAXIA. − Transient disorder (spontan recovery), several weeks. − EMG of the distal lession usually normal. − Caused by mechanical pressure, exp: − Crutch paralysis − Good prognosis. II. AXONOTMESIS − A discontinuity of the axon, with intact endoneurium. − Wallerian degenration on the distal side. − There is an axon regeneration : 1 – 3 mm/day − Good prognosis III. NEUROTMESIS − Nerve trunk has distrupted, include endoneural tube − Regeneration process Æ neuroma − Prognosis: depend on the surgery technique. SUNDERLAND Classifications: I. Loss of axonal conduction. II. Loss of continuity of the axon, with intact endoneurium. III. Transection of nerve fiber (axon & sheath), with intact perineurium. IV. Loss of perineurium and fascicular continuity. V. Loss of continuity of entire nerve trunk. DEGREE DISCONTINUITY DAMAGE TREATMENT PROGNOSIS 1st None, conduction block Distal nerve fibers Observation Excellent (neuroprxia) remain intact 2nd Axon (axonotmesis) Based on fibrosis Observation Good 3rd Axon & endoneurium Based on fibrosis Lysis Ok 4th Axon, Fibrotic Nerve graft Marginal endoneurium,perineurium connective tissue connects 5th Complete (neurotmesis) Complete Graft/transfer Poor PATOPHYSIOLOGY on the nerve compression injury: 23rd EDITION by Anika A Alhambra 1. Disturb to microcirculation Æ ischemia 2. Disturb to axoplasmic transport Æ neruroaxonal transport Intravascular edema (Increase of vascular permeability) (Degeneration process) Proliferating fibroblast Separation nerve fiber One week (Demyelination) Note: compression 20-30 mmHg Æ pathology on epineurium >80 mmHg Æ completely stop 30 mmHg (8j); 50 mmHg (2j) Æ reverse after 24 hours 400 mmHg (2j) Æ reverse after 1 week ‘Tinnel sign’, is happened on injury and compression, it is sign of regeneration process (continuity sign) Pathological changes on ‘PRIMARY NERVE REPAIR’ 1. -

Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee
To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. S E C T I O N X Articular Cartilage Procedures and Rehabilitation of the Arthritic Knee 31-1 Author: Noyes; Noyes_Section X_main.indd 1 9/23/2015 5:53:34 PM To protect the rights of the author(s) and publisher we inform you that this PDF is an uncorrected proof for internal business use only by the author(s), editor(s), reviewer(s), Elsevier and typesetter Toppan Best-set. It is not allowed to publish this proof online or in print. This proof copy is the copyright property of the publisher and is confidential until formal publication. 31 c00031 Knee Articular Cartilage Restoration Procedures Joshua D. Harris, MD, Brian J. Cole, MD, MBA OUTLINE u0010 Indications, 31-2 Preoperative Planning, 31-7 u0045 u0015 Contraindications, 31-4 Intraoperative Evaluation and Operative Technique, 31-8 u0050 u0020 Clinical Biomechanics, 31-4 Clinical Outcomes, 31-9 u0055 u0025 Clinical Evaluation, 31-5 u0030 History, 31-5 u0035 Physical Examination, 31-6 u0040 Diagnostic Tests, 31-7 Once the determination that a defect is symptomatic has p0120 s0010 INDICATIONS been made, conservative treatment options may commence. These Management of symptomatic focal chondral and osteochondral include, but are not limited to, rest, activity modification (typically defects in the knee is complex and multifactorial. -

Knee Injury Medical Treatment Guidelines©
Knee Injury Medical Treatment Guidelines© Proposed by the State of New York Department of Insurance to the Workers’ Compensation Board ©Algorithm 1 and Tables 1 and 2 are taken from the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints published and copyrighted by the American College of Occupational and Environmental Medicine. Copyright 2008, 2007, 2004, 1997 by the American College of Occupational and Environmental Medicine (ACOEM). Commercial reproduction or other use beyond fair use prohibited without explicit ACOEM permission. The American College of Occupational and Environmental Medicine has granted the Workers’ Compensation Board permission to publish Algorithm 1 and Tables 1 and 2 of the Occupational Medicine Practice Guidelines, 2nd Edition: Knee Complaints in connection with the adoption of the New York Knee Injury Medical Treatment Guidelines, including making this guideline available in print and on its website for informational and educational purposes. Use of Algorithm 1 and Tables 1 and 2 of this guideline beyond fair use or for commercial purpose, or both may only occur upon receipt of explicit permission from ACOEM. December 2007 Draft Knee Injury Medical Treatment Guidelines TABLE OF CONTENTS SECTION DESCRIPTION PAGE A. INITIAL DIAGNOSTIC PROCEDURES............................................................ 1. HISTORY-TAKING AND PHYSICIAL EXAMINATION (Hx & PE) .......... a. History of Present Injury ......................................................................... b. Past History ...........................................................................................