Trust-Open-Board-Meeting-Pack-26 February 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Suffolk's Framework for Growth
Suffolk’s Framework for Growth 1 Foreword Suffolk’s local authorities are working together to address our residents and businesses’ future needs and deliver our growth plans in an inclusive and integrated way. Responding to the Government’s ambitions to increase the nation’s overall prosperity and recognising past growth has not always benefitted all communities equally, our Framework sets out how we will utilise Suffolk’s potential to ensure we plan and achieve the growth that is right for us and our communities. A Framework provides a mechanism to bring together work across teams; including local planning, economic development, skills, and housing; alongside our partners at the University of Suffolk, Suffolk Chamber of Commerce and New Anglia LEP. It sets out how we are working across our administrative boundaries and with our key partners to deliver our physical development (homes, employment sites, public and private buildings) in a way that matches our communities’ aspirations for growth and ensures we can match this with the investment in our infrastructure both now and in the future. The Framework includes links where you can find further, more detailed information. It builds on our conversations with Government, our partners and our communities, which started with our proposals for devolution and have been built on through our responses to both the Industrial Strategy and the Housing White Paper. It will provide the mechanism for monitoring our successes and realigning work that is not achieving the outcomes we anticipate. This Framework has been agreed by all Suffolk Local Authority Leaders and the joint Suffolk Growth Portfolio Holders (GP/H). -

Support to Go Home Service
Information for patients, family, carers and staff Support to go home service What is this service? The Support to Go Home Service is comprised of health and care professionals working together to provide short term care provision for when you return home. Your social worker will have arranged a care package for you with a confirmed start date. When there is a delay to your start date, our service will be able to provide interim care to enable you to be discharged home. This service is hosted by West Suffolk Hospital and is provided in partnership with the West Suffolk NHS Foundation Trust and Suffolk County Council. There is no cost to you for this service for patients who are receiving a social care funded package of care. The team consists of an occupational therapist, care co-ordinator and support workers who will help you with your daily tasks, such as washing, dressing and meal preparation, within your home. They will work closely with you, your family, social care and the community teams, to ensure you experience a seamless service throughout your period of recovery. Aims of the service To enhance your recovery by not delaying your discharge, thus reducing your Source: Support To Go Home Service Reference No: 6306-2 Issue date: 29/4/19 Review date: 29/4/22 Page 1 of 3 risk of infections associated with a prolonged admission. To maximise your independence by offering early recovery support within your home. To provide advice, follow-up visits and referrals to external agencies as required. To ensure an appropriate level of care is provided according to your needs. -

Babergh and Mid Suffolk Joint Local Plan Statement of Common Ground
Babergh and Mid Suffolk Joint Local Plan Statement of Common Ground Between Babergh and Mid Suffolk District Councils and West Suffolk Council March 2021 1. Areas covered by the Statement of Common Ground The Statement of Common Ground relates to the area covered by the local planning authorities of Babergh District Council, Mid Suffolk District Council and West Suffolk Council. Page 1 of 10 2. Authorities covered by the Statement of Common Ground The signatories to this Statement of Common Ground are: • Babergh District Council, • Mid Suffolk District Council, and • West Suffolk Council. Ongoing engagement is being undertaken with Suffolk County Council, the West Suffolk Clinical Commissioning Group (CCG) and the West Suffolk NHS Foundation Trust and this Statement of Common Ground (SoCG) details the current position. An interim SoCG was published alongside the Joint Local Plan (JLP) Pre-Submission (Reg 19) Document (November 2020). 3. Purpose of Statement of Common Ground Local planning authorities have a statutory duty to co-operate with specified bodies in relation to strategic planning matters. The National Planning Policy Framework (NPPF) and accompanying Planning Practice Guidance require local authorities to produce a Statement of Common Ground as a written record on progress made for strategic planning matters across local authority boundaries and for this to be kept under review. Prior to the publication of the JLP Pre-Submission (Reg 19) Document, West Suffolk Council raised concerns to planning applications being determined in Thurston and to a lesser extent in Elmswell and Woolpit and the cumulative impact of residential development on public services, especially health, highways and leisure. -

Bury Town INT Executive Summary
Bury Town INT: Executive summary Place-Based Needs Assessment (version 1.0, 2019) Executive Summary Public Health Suffolk Page 1 of 11 Bury Town INT: Executive summary Place-Based Needs Assessment (version 1.0, 2019) Main authors Tom Delaney, Alliance JSNA Researcher Alison Matthews, Senior JSNA researcher Tess Zermanos, Health and Care Programme Manager Main editors Natacha Bines, Head of Population Insight Anna Crispe, Head of Knowledge & Intelligence Consultant reviewers Dr Padmanabhan Badrinath, Consultant in Public Health Medicine Dr Jeptepkeny Ronoh, Consultant in Public Health Medicine With many thanks to Integrated Neighbourhood Team colleagues and wider Suffolk colleagues for their input, collaboration and consultation. This is version 1 created on 25th November 2019 Public Health Suffolk Page 2 of 11 Bury Town INT: Executive summary Place-Based Needs Assessment (version 1.0, 2019) Contents Executive summary .................................................................................................................................. 5 Demographics ..................................................................................................................................... 5 Population ....................................................................................................................................... 5 Age profile ....................................................................................................................................... 5 Population projections ................................................................................................................... -

Council Size Proposal for a Future Council for West Suffolk Submitted
Council Size Proposal for a Future Council for West Suffolk Submitted on behalf of Forest Heath District Council and St Edmundsbury Borough Council In September 2017, Forest Heath District Council (FHDC) and St Edmundsbury Borough Council (SEBC) agreed a business case that supports the formation of a single district-tier Council for West Suffolk. This business case has now been submitted to the Secretary of State, who, under s.15 of the Cities and Local Government Devolution Act 2016, has the power to issue an Order to create the new Council. The business case and associated appendices is available at http://svr-mgov-01:9070/ieListDocuments.aspx?CId=172&MId=3649&Ver=4 That Order will include those ancillary matters necessary to bring the new Council into being. One of the most important aspects is the number of Councillors necessary to operate the new council. Whilst this decision will be made by the Secretary of State, we consider it important that we submit our views, as the current District and Borough Councillors for West Suffolk, on the number of Councillors we believe the future Council should have. This paper covers: - Background to West Suffolk as a place - Background to West Suffolk councils - Forming our argument for council size, including: o The governance arrangements of the council o Regulatory decision making o Scrutiny and oversight arrangements o Responsibility to outside bodies o The representational role of councillors o Views of the residents of West Suffolk o How our argument creates a council size - Conclusion About West Suffolk West Suffolk is a growing area. -
Rodappendix1.Docx
Appendix 1 Background West Suffolk Council, formed from the former Forest Heath and St Edmundsbury areas, came into being on 1 April 2019. West Suffolk Council has 'inherited' the local plans that were prepared for and adopted by the former St Edmundsbury and Forest Heath councils. These existing documents include both strategic policies and policies specific to the area. Preparing the West Suffolk Local Plan (WSLP) will include reviewing existing planning policies, updating, deleting and adding where appropriate to the current context and future needs. The preparation of the plan can be described in three key stages: • This issues and options stage is the very beginning of the process of producing a plan for West Suffolk. Its scope is to identify the key strategic issues. The plan should address and set out options and initial ideas for the strategic policies in areas such as housing and economic growth and where the growth might take place (distribution), and the provision of strategic infrastructure. • Further research and studies need to be carried out to provide the evidence to develop strategic and local policies. This work and responses to this issues and options stage will contribute to the next stage, the preferred options draft of the plan. It is anticipated that consultation will take place in 2021. • Responses to consultation on the second document will inform the submission draft of the local plan (anticipated publication date January 2022). It is this draft, together with the responses to it that will be examined by an independent inspector appointed by the Secretary of State. The Issues and Options consultation document lists strategic objectives under the following headings: • Business and the local economy • Climate change mitigation and adaptation • Homes • Rural areas • Environment • Communities, wellbeing and culture • Connectivity and activity The consultation document identifies three strategic issues: • Climate change West Suffolk declared a climate emergency in 2019 with the target to be net-zero carbon by 2030. -

A3131. Expenditure Over Threshold
West Suffolk Clinical Commissioning Group over £25k spend report July 2014 Entity Date Expense Type Expense area Supplier Transaction number AP Amount (£) Purchase invoice number NHS West Suffolk CCG 31/07/2014 Equipment Additions CAPITAL EXPENDITURE MILLAR WEST LTD 3449386 29,974.08 91391 NHS West Suffolk CCG 31/07/2014 Healthcare PLANNED CARE BMI HEALTHCARE COLLECTIONS 4124208 70,872.25 27151 NHS West Suffolk CCG 31/07/2014 Healthcare ACUTE HEALTHCARE WEST SUFFOLK NHS FOUNDATION TRUST 4124212 36,445.00 233397 NHS West Suffolk CCG 31/07/2014 Healthcare COMMUNITY SERVICES SUFFOLK COUNTY COUNCIL 4124361 39,947.00 9132282 NHS West Suffolk CCG 31/07/2014 Healthcare COMMUNITY SERVICES SUFFOLK COUNTY COUNCIL 4124368 39,947.00 9132279 NHS West Suffolk CCG 31/07/2014 Healthcare COMMUNITY SERVICES SUFFOLK COUNTY COUNCIL 4124373 39,947.00 9132281 NHS West Suffolk CCG 31/07/2014 Healthcare PLANNED CARE BMI HEALTHCARE COLLECTIONS 4124378 45,206.59 27468 NHS West Suffolk CCG 31/07/2014 Computer Maintenance IM&T NORFOLK & SUFFOLK NHS FOUNDATION TRUST 4124565 112,692.00 I0009467 NHS West Suffolk CCG 31/07/2014 Grants CAPITAL GUILDHALL & BARROW SURGERY 4124669 28,105.00 23062014 NHS West Suffolk CCG 31/07/2014 Grants CAPITAL CHRISTMAS MALTINGS & CLEMENTS PRACTICE 4124690 44,250.00 OVER75CCG062014 NHS West Suffolk CCG 31/07/2014 Healthcare CHILDRENS SERVICES SUFFOLK COUNTY COUNCIL 4124694 35,772.44 9133357 NHS West Suffolk CCG 31/07/2014 Healthcare ACUTE HEALTHCARE PATHOLOGY PARTNERSHIP 4137459 302,821.00 77000102 NHS West Suffolk CCG 31/07/2014 Healthcare -

Anticoagulant Monitoring Service
Anticoagulation Service Introduction This is a brief guide to some important facts about warfarin and how our service works. Please read this leaflet with care and keep it for future reference. Information pack The accompanying information pack includes a booklet called Oral Anticoagulant Therapy: Important Information for Patients. This booklet provides general information about taking warfarin, side effects and things which can affect your anticoagulation control. Please read this booklet carefully and keep it for future reference. The information pack also includes an alert card; please carry this card with you at all times in case of emergency and to show to healthcare professionals such as doctors, dentists and pharmacists when you see them. Warfarin counselling We will contact you to arrange a counselling session with an Anticoagulation Nurse Specialist. The purpose of the counselling session is to ensure that you have all the information that you need to understand what you can do to help keep your anticoagulation at a safe and effective level. We will also discuss possible side effects with you and what to do in an emergency. We will also tell you how our service works and how to contact us when you need to. Blood tests We need to monitor your anticoagulation therapy to ensure that is stays at the right level for you. We monitor your anticoagulation using a blood test called the INR (International Normalised Ratio). A blood sample may be taken from a vein in the arm (a venous sample) or by finger-prick. A venous sample can be taken in most Source: Department of Specialist Medicine Reference No: 5464-6 Issue date: 15/10/18 Review date: 15/10/20 Page 1 of 4 GP practices (your GP practice can confirm whether they offer this service) and at other locations such as the West Suffolk Hospital, Newmarket Hospital and Sudbury Community Health Centre (see How to Book a Blood Test below for further information). -
SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with Demand Adjustments
Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with demand adjustments SCC LP 9.2 OCTOBER 2020 PUBLIC Suffolk County Council SUFFOLK LOCAL PLAN MODELLING Forecasting Report - Forecasts with demand adjustments TYPE OF DOCUMENT (VERSION) PUBLIC PROJECT NO. 70044944 OUR REF. NO. SCC LP 9.2 DATE: OCTOBER 2020 WSP WSP House 70 Chancery Lane London WC2A 1AF Phone: +44 20 7314 5000 Fax: +44 20 7314 5111 WSP.com PUBLIC QUALITY CONTROL Issue/revision First issue Revision 1 Revision 2 Revision 3 Remarks Draft Draft Final Date July 2020 September 2020 October 2020 Prepared by Louise Murray- Leonardo Mendes Leonardo Mendes Bruce Signature Checked by Leonardo Mendes Charlotte Herridge Charlotte Herridge Signature Authorised by Michael Johns Michael Johns Michael Johns Signature Project number 70044944 70044944 70044944 Report number SCC_LP 9.0 SCC_LP 9.1 SCC_LP 9.2 File reference SUFFOLK LOCAL PLAN MODELLING PUBLIC | WSP Project No.: 70044944 | Our Ref No.: SCC LP 9.2 October 2020 Suffolk County Council CONTENTS EXECUTIVE SUMMARY 1 GLOSSARY 1 2 INTRODUCTION 4 2.1 BACKGROUND 4 2.2 TRANSPORT MODEL 4 2.3 STUDY AREA 6 2.4 FUTURE HIGHWAY SCHEMES 11 2.5 FORECAST DEVELOPMENT ASSUMPTIONS 14 3 RESULTS 16 3.1 SUFFOLK HIGHWAY FOCUS 16 3.2 VOLUME TO CAPACITY RATIO 16 3.3 MODEL RUNS COMPARED 16 3.4 PASSENGER CAR UNIT HOUR DELAY REDUCTION BY LPA – DEMAND ADJUSTMENT IMPACT 17 3.5 OVERALL JUNCTION V/C SUMMARY BY LPA – DEMAND ADJUSTMENT IMPACT 22 3.6 OVERALL LINK V/C SUMMARY BY LPA – DEMAND ADJUSTMENT IMPACT 25 3.7 RESULTS SUMMARIES -

County Moth Recorders
County Moth Recorders VC1 & VC2 West Cornwall & East Cornwall All species Leon Truscott, 59 Cremyll Road, Torpoint, Cornwall PL11 2DZ Email: [email protected] Tel: 01752 812023 VC3 & VC4 South Devon & North Devon All species Barry Henwood, 6 Lakeland, Abbotskerswell, Devon, TQ12 5YF Email: [email protected] Tel: 01626 364080 VC5 & VC6 South Somerset and North Somerset Macro moths Chris Iles Email: [email protected] Micro moths Neale Mellersh, 40 Carlingford Terrace, Radstock, Bath And North East Somerset, BA3 3QA Email: [email protected] Tel: 01761 753297 VC7 & VC8 North Wiltshire & South Wiltshire All species Wayne Clinch, 3 The Buntings, Covingham, Swindon, Wiltshire, SN3 5AS Email: [email protected] Tel: 07803 366378 VC9 Dorset All species Record submission: [email protected] VC10 Isle of Wight All species Jim Baldwin, 21 Hillcrest Road, Rookley, Ventnor, Isle of Wight, PO38 3PB Email: [email protected] Tel. 01983 721137 or 07528 586683 VC11 & VC12 South Hampshire & North Hampshire All species Mike Wall, 11 Waterloo Avenue, Basingstoke, Hampshire, RG23 8DL Email: [email protected] Tel: 01256 819631 VC13 & VC14 West Sussex & East Sussex All species Colin Pratt, 5 View Road, Peacehaven, East Sussex, BN10 8DE Email: [email protected] Tel: 01273 586780 Page 1 of 13 Updated 30/11/2020 VC15 East Kent Macro-moths Ian Hunter, 25 Sandown Road, Sandwich, Kent, CT13 9NY Email: [email protected] Micro-moths Dave Shenton, 25 Ratling Road, Aylesham, Kent, CT3 3BA Email: [email protected] VC16 West Kent Macro-moths Ian Hunter, 25 Sandown Road, Sandwich, Kent, CT13 9NY Email: [email protected] Micro-moths Dave Shenton, 25 Ratling Road, Aylesham, Kent, CT3 3BA Email: [email protected] VC17 Surrey All species Graham Collins, 15 Hurst Way, South Croydon, Surrey, CR2 7AP Email: [email protected] VC18 & VC19 South Essex & North Essex All species Peter R. -

Lead Area Local Authorities Covered by Funding Provisional 2020/21
Lead area Local authorities covered by funding Provisional 2020/21 funding allocation Adur and Worthing £421,578.00 Arun £318,817.00 Ashford £257,000.00 Babergh Babergh and Mid Suffolk (lead) £163,498.00 West Suffolk Barking and Dagenham £184,703.00 Barnet £636,845.00 Barnsley £102,900.00 Basildon £474,871.00 Basingstoke and Deane £199,850.00 Bath and North East Somerset £417,151.00 Bedford £986,915.00 Birmingham £684,666.00 Blackburn with Darwen Hyndburn BC £184,000.00 Ribble Valley BC Burnley BC Pendle BC Rossendale BC Blackpool £200,000.00 Bolton £124,997.00 Boston £385,451.00 Bournemouth, Christchurch and £1,401,333.00 Poole Bracknell Forest £356,141.00 Bradford £461,320.00 Breckland £106,500.00 Brent £827,422.00 Brighton and Hove £2,042,637.00 Bristol, City of £2,814,768.00 Bromley £103,654.00 Broxbourne £119,380.00 Buckinghamshire Aylesbury Vale £576,500.00 Wycombe Chiltern South Bucks Bury £40,000.00 Calderdale £253,945.00 Cambridge £486,457.00 Cambridgeshire County Council £229,500.00 Camden £1,327,000.00 Canterbury £584,739.00 Carlisle (lead for all Cumbrian Allerdale Borough Council £416,340.00 authorities) Barrow Borough Council Carlisle City Council Copeland Borough Council Cumbria County Council Eden District Council South Lakeland District Council Central Bedfordshire £329,938.00 Cheshire East £438,329.30 Cheshire West and Chester £731,034.00 Chichester £230,465.00 City of London £590,300.00 Colchester £296,144.00 Corby East Northamptonshire £113,000.00 Kettering Wellingborough Cornwall £1,696,467.00 County Durham £269,128.35 -
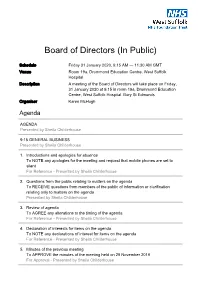
Board of Directors (In Public)
Board of Directors (In Public) Schedule Friday 31 January 2020, 9:15 AM — 11:30 AM GMT Venue Room 19a, Drummond Education Centre, West Suffolk Hospital Description A meeting of the Board of Directors will take place on Friday, 31 January 2020 at 9.15 in room 19a, Drummond Education Centre, West Suffolk Hospital, Bury St Edmunds Organiser Karen McHugh Agenda AGENDA Presented by Sheila Childerhouse 9:15 GENERAL BUSINESS Presented by Sheila Childerhouse 1. Introductions and apologies for absence To NOTE any apologies for the meeting and request that mobile phones are set to silent For Reference - Presented by Sheila Childerhouse 2. Questions from the public relating to matters on the agenda To RECEIVE questions from members of the public of information or clarification relating only to matters on the agenda Presented by Sheila Childerhouse 3. Review of agenda To AGREE any alterations to the timing of the agenda For Reference - Presented by Sheila Childerhouse 4. Declaration of interests for items on the agenda To NOTE any declarations of interest for items on the agenda For Reference - Presented by Sheila Childerhouse 5. Minutes of the previous meeting To APPROVE the minutes of the meeting held on 29 November 2019 For Approval - Presented by Sheila Childerhouse 6. Matters arising action sheet To ACCEPT updates on actions not covered elsewhere on the agenda For Report - Presented by Sheila Childerhouse 7. Chief Executive’s report To ACCEPT a report on current issues from the Chief Executive For Report - Presented by Stephen Dunn 9:40 DELIVER FOR TODAY 8. Integrated quality and performance report To ACCEPT the report For Report - Presented by Rowan Procter and Helen Beck 9.