ALWAYS THERE the Remarkable Life of Ruth Lillian Kirschstein, M.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cultural Anthropology Through the Lens of Wikipedia: Historical Leader Networks, Gender Bias, and News-Based Sentiment
Cultural Anthropology through the Lens of Wikipedia: Historical Leader Networks, Gender Bias, and News-based Sentiment Peter A. Gloor, Joao Marcos, Patrick M. de Boer, Hauke Fuehres, Wei Lo, Keiichi Nemoto [email protected] MIT Center for Collective Intelligence Abstract In this paper we study the differences in historical World View between Western and Eastern cultures, represented through the English, the Chinese, Japanese, and German Wikipedia. In particular, we analyze the historical networks of the World’s leaders since the beginning of written history, comparing them in the different Wikipedias and assessing cultural chauvinism. We also identify the most influential female leaders of all times in the English, German, Spanish, and Portuguese Wikipedia. As an additional lens into the soul of a culture we compare top terms, sentiment, emotionality, and complexity of the English, Portuguese, Spanish, and German Wikinews. 1 Introduction Over the last ten years the Web has become a mirror of the real world (Gloor et al. 2009). More recently, the Web has also begun to influence the real world: Societal events such as the Arab spring and the Chilean student unrest have drawn a large part of their impetus from the Internet and online social networks. In the meantime, Wikipedia has become one of the top ten Web sites1, occasionally beating daily newspapers in the actuality of most recent news. Be it the resignation of German national soccer team captain Philipp Lahm, or the downing of Malaysian Airlines flight 17 in the Ukraine by a guided missile, the corresponding Wikipedia page is updated as soon as the actual event happened (Becker 2012. -
April 20, NOTE
PRINCIPAL OFFICIALS in the V.XECUTIVE BRANCH Appointed January 20 - April 20, 1953 NOTE: This list is limited to appointments made after January 20, 1953. Names con- tained herein replace corre- sponding names appearing in the 1952-53 U.S. Government Organization Manual. Federal Register Division National Archives and Records Service General Services Administration Washington 25, D. C. MEMBERS OF THE CABINET TEE PRESIDENT John Foster Dulles, of New York, Secretary of State. President of the United States.-- Dwight D. Eisenhower George M. Humphrey, of Ohio, Secre- tary of the Treasury. EXECUTIVE OFFICE OF THE PRESIDENT Charles Erwin Wilson, of Michigan, Secretary of Defense. The White House Office Herbert Brownell, Jr., of New York, 1600 Pennsylvania Avenue NW. Attorney General. NAtional 8-1414 Arthur E. Summerfield, of Michigan, The Assistant to the President.-- Postmaster General. Sherman Adams Assistant to The Assistant to the Douglas McKay, of Oregon, Secretary President.--Maxwell M. Rabb of the Interior. Special Assistant to The Assistant to the President.--Roger Steffan Ezra Taft Benson, of Utah, Secretary Special Assistant to The Assistant of Agriculture. to the President.--Charles F. Willis, Jr. Sinclair Weeks, of Massachusetts, Special Assistants in the White Secretary of Commerce Haase Office: L. Arthur Minnich, Jr. Martin P. Durkin, of Maryland, James M. Lambie Secretary of Labor. Special Counsel to the President (Acting Secretary).--Thomas E. Mrs. Oveta Culp Hobby, of Texas, Stephens Secretary of Health, Education, Secretary to the President (Press).-- and Welfare James C. Hagerty Assistant Press Secretary.--Murray Snyder Acting Special Counsel to the Presi- For sale by the dent.--Bernard M. -
NIHAA Summer 1993
The Newsletter of the NIH Alumni Association Summer 1993 Vol. 5, No . 2 date Nobel Laureate Harold Varmus Nominated as 14th NIH Director Ruth Kirschstein Named Acting Director President Clinton on A ug. 3 announced his intention to nominate Dr. Harold Eliot Varmus as the 14th director of th e National Institutes of Health. A Senate confirmation process must precede Yarmus· taking over leadership of the institutes. Winner of the Nobel Prize in 1989 for his work in cancer research. Va1111us. 53. is a professor of microbi ology. biochemistry. and biophysics. and the American Cancer Society pro fessor vfmoh:cu/ur >1iro/O£)' iJI l/Je Uni versity of California, San Francisco. He is a leader in the stu dy of cancer causing genes called "oncogenes," and an intemationall-y fecogni:z.ed authof\t-y Dr. Ruth l. Kirschsteln , acting NIH director on retroviruses. the viruses that cause Dr. Harold E. Varmus , direclor-designale AIDS and many cancers in animnl.. FIC 25 Years Old In '93 Thirty-eight-year NIH veteran Dr. Research Festival '93 Schedule Ruth Kirschstein. director of NIGM S Scholars-in-Residence (See Director p. 6) NIHAA Members Invited Program Celebrates To Alumni Symposium In This Issue Tile fas\ morning ofNCH Rc:-.c;\rch Nursing cell/er /J1·1·111111•s Festival '93-Monday. Sept. 20-has This year. the Fogarty Intern ational 17th i11s1it11tc• 111 NII/ p. ? been designated National lnsritute of Center (FIC) is 25 years old . T he cen Greeri11gs from 1/,11 1w11• NII /AA prl'sidt'lll. Diabetes and Digestive and Kidney Tltolll(IS .I. -

UNIVERSITY of CALIFORNIA, IRVINE Unraveling Host and Parasite Pathways in Human Innate Immunity to Toxoplasma Gondii DISSERTATIO
UNIVERSITY OF CALIFORNIA, IRVINE Unraveling host and parasite pathways in human innate immunity to Toxoplasma gondii DISSERTATION submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in Biological Sciences by Lanny Gov Dissertation Committee: Assistant Professor Melissa B. Lodoen, Chair Professor Andrea J. Tenner Professor Craig M. Walsh 2014 Chapter 2 © 2013 American Society for Microbiology All other materials © 2014 Lanny Gov DEDICATION To My mother: my hero and my champion; Jonathan Farnworth: my better half; My loving and supportive family: brothers George and James, and sister-in-law Kelly; My dearest friends: Eugenia Hu, Quen Vong, Tracy Tang, and Erika Villaruel Thank you for so many years of love, laughter, and encouragement, and for helping me believe I could accomplish anything. “Promise me you’ll always remember: You’re braver than you believe, and stronger than you seem, and smarter than you think.” –A.A. Milne, Winnie-the-Pooh “You don’t have to know everything, but you should try to.” -Nori Ueno, on preparation for my Advancement exam ii TABLE OF CONTENTS Page LIST OF FIGURES iv LIST OF TABLES v ACKNOWLEDGMENTS vi CURRICULUM VITAE ix ABSTRACT OF THE DISSERTATION xii CHAPTER ONE: Introduction to Toxoplasma gondii Immunity 1 Toxoplasma gondii Biology 2 T. gondii Clinical Disease 6 T. gondii Invasion of Host Cells 9 Three Modes of T. gondii Intracellular Entry 12 Immunity to T. gondii 13 Toll-like Receptor Sensing of T. gondii 15 Nod-like Receptor Sensing of T. gondii 17 Modulation of Host Cell Pathways by T. gondii Effectors 19 Monocytes in Immunity to T. -
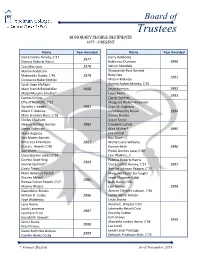
Honorary Degree Recipients 1977 – Present
Board of Trustees HONORARY DEGREE RECIPIENTS 1977 – PRESENT Name Year Awarded Name Year Awarded Claire Collins Harvey, C‘37 Harry Belafonte 1977 Patricia Roberts Harris Katherine Dunham 1990 Toni Morrison 1978 Nelson Mandela Marian Anderson Marguerite Ross Barnett Ruby Dee Mattiwilda Dobbs, C‘46 1979 1991 Constance Baker Motley Miriam Makeba Sarah Sage McAlpin Audrey Forbes Manley, C‘55 Mary French Rockefeller 1980 Jesse Norman 1992 Mabel Murphy Smythe* Louis Rawls 1993 Cardiss Collins Oprah Winfrey Effie O’Neal Ellis, C‘33 Margaret Walker Alexander Dorothy I. Height 1981 Oran W. Eagleson Albert E. Manley Carol Moseley Braun 1994 Mary Brookins Ross, C‘28 Donna Shalala Shirley Chisholm Susan Taylor Eleanor Holmes Norton 1982 Elizabeth Catlett James Robinson Alice Walker* 1995 Maya Angelou Elie Wiesel Etta Moten Barnett Rita Dove Anne Cox Chambers 1983 Myrlie Evers-Williams Grace L. Hewell, C‘40 Damon Keith 1996 Sam Nunn Pinkie Gordon Lane, C‘49 Clara Stanton Jones, C‘34 Levi Watkins, Jr. Coretta Scott King Patricia Roberts Harris 1984 Jeanne Spurlock* Claire Collins Harvey, C’37 1997 Cicely Tyson Bernice Johnson Reagan, C‘70 Mary Hatwood Futrell Margaret Taylor Burroughs Charles Merrill Jewel Plummer Cobb 1985 Romae Turner Powell, C‘47 Ruth Davis, C‘66 Maxine Waters Lani Guinier 1998 Gwendolyn Brooks Alexine Clement Jackson, C‘56 William H. Cosby 1986 Jackie Joyner Kersee Faye Wattleton Louis Stokes Lena Horne Aurelia E. Brazeal, C‘65 Jacob Lawrence Johnnetta Betsch Cole 1987 Leontyne Price Dorothy Cotton Earl Graves Donald M. Stewart 1999 Selma Burke Marcelite Jordan Harris, C‘64 1988 Pearl Primus Lee Lorch Dame Ruth Nita Barrow Jewel Limar Prestage 1989 Camille Hanks Cosby Deborah Prothrow-Stith, C‘75 * Former Student As of November 2019 Board of Trustees HONORARY DEGREE RECIPIENTS 1977 – PRESENT Name Year Awarded Name Year Awarded Max Cleland Herschelle Sullivan Challenor, C’61 Maxine D. -

Presidents Worksheet 43 Secretaries of State (#1-24)
PRESIDENTS WORKSHEET 43 NAME SOLUTION KEY SECRETARIES OF STATE (#1-24) Write the number of each president who matches each Secretary of State on the left. Some entries in each column will match more than one in the other column. Each president will be matched at least once. 9,10,13 Daniel Webster 1 George Washington 2 John Adams 14 William Marcy 3 Thomas Jefferson 18 Hamilton Fish 4 James Madison 5 James Monroe 5 John Quincy Adams 6 John Quincy Adams 12,13 John Clayton 7 Andrew Jackson 8 Martin Van Buren 7 Martin Van Buren 9 William Henry Harrison 21 Frederick Frelinghuysen 10 John Tyler 11 James Polk 6 Henry Clay (pictured) 12 Zachary Taylor 15 Lewis Cass 13 Millard Fillmore 14 Franklin Pierce 1 John Jay 15 James Buchanan 19 William Evarts 16 Abraham Lincoln 17 Andrew Johnson 7, 8 John Forsyth 18 Ulysses S. Grant 11 James Buchanan 19 Rutherford B. Hayes 20 James Garfield 3 James Madison 21 Chester Arthur 22/24 Grover Cleveland 20,21,23James Blaine 23 Benjamin Harrison 10 John Calhoun 18 Elihu Washburne 1 Thomas Jefferson 22/24 Thomas Bayard 4 James Monroe 23 John Foster 2 John Marshall 16,17 William Seward PRESIDENTS WORKSHEET 44 NAME SOLUTION KEY SECRETARIES OF STATE (#25-43) Write the number of each president who matches each Secretary of State on the left. Some entries in each column will match more than one in the other column. Each president will be matched at least once. 32 Cordell Hull 25 William McKinley 28 William Jennings Bryan 26 Theodore Roosevelt 40 Alexander Haig 27 William Howard Taft 30 Frank Kellogg 28 Woodrow Wilson 29 Warren Harding 34 John Foster Dulles 30 Calvin Coolidge 42 Madeleine Albright 31 Herbert Hoover 25 John Sherman 32 Franklin D. -
2008 Annual Report
2008 Annual Report NATIONAL ACADEMY OF ENGINEERING ENGINEERING THE FUTURE 1 Letter from the President 3 In Service to the Nation 3 Mission Statement 4 Program Reports 4 Engineering Education 4 Center for the Advancement of Scholarship on Engineering Education 6 Technological Literacy 6 Public Understanding of Engineering Developing Effective Messages Media Relations Public Relations Grand Challenges for Engineering 8 Center for Engineering, Ethics, and Society 9 Diversity in the Engineering Workforce Engineer Girl! Website Engineer Your Life Project Engineering Equity Extension Service 10 Frontiers of Engineering Armstrong Endowment for Young Engineers-Gilbreth Lectures 12 Engineering and Health Care 14 Technology and Peace Building 14 Technology for a Quieter America 15 America’s Energy Future 16 Terrorism and the Electric Power-Delivery System 16 U.S.-China Cooperation on Electricity from Renewables 17 U.S.-China Symposium on Science and Technology Strategic Policy 17 Offshoring of Engineering 18 Gathering Storm Still Frames the Policy Debate 20 2008 NAE Awards Recipients 22 2008 New Members and Foreign Associates 24 2008 NAE Anniversary Members 28 2008 Private Contributions 28 Einstein Society 28 Heritage Society 29 Golden Bridge Society 29 Catalyst Society 30 Rosette Society 30 Challenge Society 30 Charter Society 31 Other Individual Donors 34 The Presidents’ Circle 34 Corporations, Foundations, and Other Organizations 35 National Academy of Engineering Fund Financial Report 37 Report of Independent Certified Public Accountants 41 Notes to Financial Statements 53 Officers 53 Councillors 54 Staff 54 NAE Publications Letter from the President Engineering is critical to meeting the fundamental challenges facing the U.S. economy in the 21st century. -
Sprague Ted in North East
Sprague Ted in North East 2 Freeport Rd, North East, PA 16428 Cross Streets: Near the intersection of Freeport Rd and Freeport Ln (814) 725-2319 We found Ted Sprague in 17 states. See Ted's 1) contact info 2) public records 3) Twitter & social profiles 4) background check. Search free at BeenVerified. Seen As: Ted Sprague IV. Addresses: 11078 Freeport Ln, North East, PA. View Profile. Ted G Sprague. As a child growing up in North Korea, Hyeonseo Lee thought her country was "the best on the planet." It wasn't until the famine of the 90s that she began to wonder. She escaped the country at 14, to begin a life in hiding, as a refugee in China. Hers is a harrowing, personal tale of survival and hope â” and a powerful reminder of those who face constant danger, even when the border is far behind. Ted Sprague was a resident of Los Angeles, CA. He was the son of Mindy Sprague and the husband of Karen Sprague. He was an evolved human who had the ability to emit radiation from his body. He was killed by Sylar. Matt and Audrey are investigating the murder of Robert Fresco, an oncologist at UCLA. His body was found burned to a char and emitting 1,800 curies of radiation. A fingerprint found seared into the man's bone is matched using the FBI's CODIS system to Theodore Sprague. Ted Sprague has the ability of radiation. He was mistaken as Sylar a several times. He previously teamed-up with Matt Parkman and Wireless in order to bring down the Company. -

Poliomyelitis in the Lone Star State
POLIOMYELITIS IN THE LONE STAR STATE: A BRIEF EXAMINATION IN RURAL AND URBAN COMMUNITIES THESIS Presented to the Graduate Council of Texas State University in Partial Fulfillment of the Requirements For the Degree Master of Arts By Jason C. Lee San Marcos, Texas December, 2005 Insert signature page here ii COPYRIGHT By Jason Chu Lee 2005 iii ACKNOWLEDGEMENTS It leaves me in a stupor to contemplate all those I have to thank for aiding me in this effort. If I leave anybody out, please accept my most humble apologies, as the list is long. I will be the first to admit that this work is flawed, despite the best efforts of my committee to save me from myself. Had I utilized them more, this piece would only be improved. I had never undertaken a project of this scope before and though I believe I have accomplished much, the experience has been humbling. Never again will I utter the phrase, “just a thesis.” My biggest thanks go out to Dr. Mary Brennan, my committee chair and mentor. Without her guidance I most certainly would have needed to take comprehensive finals to graduate. She helped me salvage weeks of research that I thought had no discernable use. But Dr. Brennan, despite her very, very busy schedule with the department and her family, still found the time to help me find my thesis in all the data. She is well loved in the department for obvious reasons, as she has a gift for being firm and professional while remaining compassionate. Dr. James Wilson and Dr. -

Thursday, July 7, 2016 Email: [email protected] Vol
4040 yearsyears ofof coveringcovering SouthSouth BeltBelt Voice of Community-Minded People since 1976 Thursday, July 7, 2016 Email: [email protected] www.southbeltleader.com Vol. 41, No. 23 Vacation photos sought The Leader is seeking readers’ 2016 vaca- Hughes Road construction causes headaches tion photos for possible publication. A first- and second-place prize of Schlitterbahn tickets Construction work along Hughes Road con- least one shop owner has temporarily shuttered tomobile accidents at the corner of Beamer and vide key upgrades such as water lines, sanitary will be awarded monthly during June, July and tinues to irk local residents and business owners, his doors until the traffi c situation improves. Hughes. While the offi cial number of collisions sewers, new concrete pavement, sidewalks and August to the best submissions. Each month’s who say the project is causing widespread confu- The Leader has put a request in to the City of was unavailable at press time Wednesday, the curbs, street lighting, traffi c control and new sig- first-place winner will be awarded eight tick- sion and traffi c congestion. Houston Public Works and Engineering Depart- Leader has heard from multiple Houston police nage. ets, while each month’s second-place winner A primary concern is the added traffi c when ment to see if the signals can be adjusted at the offi cers that at least one crash takes place per day Despite all of the current issues, construction will be awarded six. traveling north on Beamer toward Hughes from intersection to improve traffi c fl ow. According to at the intersection – some of which are serious in is reportedly on schedule and set to be complete All submissions should include where and Scarsdale. -

Copyrighted Material
PART ON E F IS FOR FORTUNE COPYRIGHTED MATERIAL CCH001.inddH001.indd 7 99/18/10/18/10 77:13:28:13:28 AAMM CCH001.inddH001.indd 8 99/18/10/18/10 77:13:28:13:28 AAMM LOST IN LOST ’ S TIMES Richard Davies Lost and Losties have a pretty bad reputation: they seem to get too much fun out of telling and talking about stories that everyone else fi nds just irritating. Even the Onion treats us like a bunch of fanatics. Is this fair? I want to argue that it isn ’ t. Even if there are serious problems with some of the plot devices that Lost makes use of, these needn ’ t spoil the enjoyment of anyone who fi nds the series fascinating. Losing the Plot After airing only a few episodes of the third season of Lost in late 2007, the Italian TV channel Rai Due canceled the show. Apparently, ratings were falling because viewers were having diffi culty following the plot. Rai Due eventually resumed broadcasting, but only after airing The Lost Survivor Guide , which recounts the key moments of the fi rst two seasons and gives a bit of background on the making of the series. Even though I was an enthusiastic Lostie from the start, I was grateful for the Guide , if only because it reassured me 9 CCH001.inddH001.indd 9 99/18/10/18/10 77:13:28:13:28 AAMM 10 RICHARD DAVIES that I wasn’ t the only one having trouble keeping track of who was who and who had done what. -

Dr Sabin's Legacy to the World Jaime Sepulveda
World Health • 46th Year, No . 3, Moy-June 1993 IS Dr Sabin's legacy to the world Jaime Sepulveda oliomyelitis has been eradicated Poliomyelitis acquired epidemic from the Americas and other proportions in the Americas at the end Pareas, and is expected to be of the last century, mainly in the most eliminated from the world by 1995. developed regions. In Mexico, the first This outstanding achievement has epidemic outbreaks started in the been made possible thanks to the 1940s and caused many victims. The availability of an excellent vaccine oral poliovaccine was made available coupled with successful vaccination in Mexico in the early 1960s. programmes. Few actions in public Coverage was low then, and mainly health have become so deservedly concentrated among well-to-do prestigious as the vaccination children. In the 1970s, a new national campatgns. programme reached much greater The first major achievement of the numbers of children and poliomyelitis immunization effort was the cases began to drop. eradication from the world of However, it was not until1985 that smallpox in the late 1970s. But the a new polio immunization initiative success with smallpox is only the took place, with the goal of reaching all children, regardless of social status Or Albert Bruce Sobin, who perfected the first most visible component of all the viable live vaccine against polio. many benefits conferred by or geographic location. This new immunization programmes strategy, focusing on "National worldwide. Not only have they Vaccination Days", was originally brought about the survival of children proposed by Professor Albert Sabin, who would otherwise have died; they the US scientist who developed the have greatly enhanced the quality of oral poliomyelitis vaccine.