Not for Publication Or Presentation a G E N D a CIBMTR WORKING
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers
Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers. by Kelly Kennaley A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Molecular and Cellular Pathology) in the University of Michigan 2019 Doctoral Committee: Associate Professor Zaneta Nikolovska-Coleska, Co-Chair Adjunct Associate Professor Scott A. Tomlins, Co-Chair Associate Professor Eric R. Fearon Associate Professor Alexey I. Nesvizhskii Kelly R. Kennaley [email protected] ORCID iD: 0000-0003-2439-9020 © Kelly R. Kennaley 2019 Acknowledgements I have immeasurable gratitude for the unwavering support and guidance I received throughout my dissertation. First and foremost, I would like to thank my thesis advisor and mentor Dr. Scott Tomlins for entrusting me with a challenging, interesting, and impactful project. He taught me how to drive a project forward through set-backs, ask the important questions, and always consider the impact of my work. I’m truly appreciative for his commitment to ensuring that I would get the most from my graduate education. I am also grateful to the many members of the Tomlins lab that made it the supportive, collaborative, and educational environment that it was. I would like to give special thanks to those I’ve worked closely with on this project, particularly Dr. Moloy Goswami for his mentorship, Lei Lucy Wang, Dr. Sumin Han, and undergraduate students Bhavneet Singh, Travis Weiss, and Myles Barlow. I am also grateful for the support of my thesis committee, Dr. Eric Fearon, Dr. Alexey Nesvizhskii, and my co-mentor Dr. Zaneta Nikolovska-Coleska, who have offered guidance and critical evaluation since project inception. -

Smu1 and RED Are Required for Activation of Spliceosomal B Complexes Assembled on Short Introns
ARTICLE https://doi.org/10.1038/s41467-019-11293-8 OPEN Smu1 and RED are required for activation of spliceosomal B complexes assembled on short introns Sandra Keiper 1, Panagiotis Papasaikas 2,4,5, Cindy L. Will1, Juan Valcárcel2,3, Cyrille Girard1 & Reinhard Lührmann1 1234567890():,; Human pre-catalytic spliceosomes contain several proteins that associate transiently just prior to spliceosome activation and are absent in yeast, suggesting that this critical step is more complex in higher eukaryotes. We demonstrate via RNAi coupled with RNA-Seq that two of these human-specific proteins, Smu1 and RED, function both as alternative splicing regulators and as general splicing factors and are required predominantly for efficient splicing of short introns. In vitro splicing assays reveal that Smu1 and RED promote spliceosome activation, and are essential for this step when the distance between the pre-mRNA’s5′ splice site (SS) and branch site (BS) is sufficiently short. This Smu1-RED requirement can be bypassed when the 5′ and 3′ regions of short introns are physically separated. Our obser- vations suggest that Smu1 and RED relieve physical constraints arising from a short 5′SS-BS distance, thereby enabling spliceosomes to overcome structural challenges associated with the splicing of short introns. 1 Department of Cellular Biochemistry, Max Planck Institute for Biophysical Chemistry, Am Fassberg 11, 37077 Göttingen, Germany. 2 Centre de Regulació Genòmica, The Barcelona Institute of Science and Technology and Universitat Pompeu Fabra, Dr. Aiguader 88, 08003 Barcelona, Spain. 3 Institució Catalana de Recerca i Estudis Avançats (ICREA), Pg. Lluís Companys, 08010 Barcelona, Spain. 4Present address: Friedrich Miescher Institute for Biomedical Research (FMI), Maulbeerstrasse 66, 4058 Basel, Switzerland. -
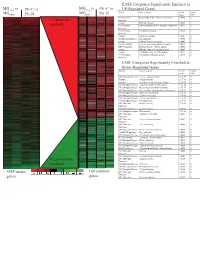
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

Enzyme DHRS7
Toward the identification of a function of the “orphan” enzyme DHRS7 Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Selene Araya, aus Lugano, Tessin Basel, 2018 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Alex Odermatt (Fakultätsverantwortlicher) und Prof. Dr. Michael Arand (Korreferent) Basel, den 26.6.2018 ________________________ Dekan Prof. Dr. Martin Spiess I. List of Abbreviations 3α/βAdiol 3α/β-Androstanediol (5α-Androstane-3α/β,17β-diol) 3α/βHSD 3α/β-hydroxysteroid dehydrogenase 17β-HSD 17β-Hydroxysteroid Dehydrogenase 17αOHProg 17α-Hydroxyprogesterone 20α/βOHProg 20α/β-Hydroxyprogesterone 17α,20α/βdiOHProg 20α/βdihydroxyprogesterone ADT Androgen deprivation therapy ANOVA Analysis of variance AR Androgen Receptor AKR Aldo-Keto Reductase ATCC American Type Culture Collection CAM Cell Adhesion Molecule CYP Cytochrome P450 CBR1 Carbonyl reductase 1 CRPC Castration resistant prostate cancer Ct-value Cycle threshold-value DHRS7 (B/C) Dehydrogenase/Reductase Short Chain Dehydrogenase Family Member 7 (B/C) DHEA Dehydroepiandrosterone DHP Dehydroprogesterone DHT 5α-Dihydrotestosterone DMEM Dulbecco's Modified Eagle's Medium DMSO Dimethyl Sulfoxide DTT Dithiothreitol E1 Estrone E2 Estradiol ECM Extracellular Membrane EDTA Ethylenediaminetetraacetic acid EMT Epithelial-mesenchymal transition ER Endoplasmic Reticulum ERα/β Estrogen Receptor α/β FBS Fetal Bovine Serum 3 FDR False discovery rate FGF Fibroblast growth factor HEPES 4-(2-Hydroxyethyl)-1-Piperazineethanesulfonic Acid HMDB Human Metabolome Database HPLC High Performance Liquid Chromatography HSD Hydroxysteroid Dehydrogenase IC50 Half-Maximal Inhibitory Concentration LNCaP Lymph node carcinoma of the prostate mRNA Messenger Ribonucleic Acid n.d. -

Noelia Díaz Blanco
Effects of environmental factors on the gonadal transcriptome of European sea bass (Dicentrarchus labrax), juvenile growth and sex ratios Noelia Díaz Blanco Ph.D. thesis 2014 Submitted in partial fulfillment of the requirements for the Ph.D. degree from the Universitat Pompeu Fabra (UPF). This work has been carried out at the Group of Biology of Reproduction (GBR), at the Department of Renewable Marine Resources of the Institute of Marine Sciences (ICM-CSIC). Thesis supervisor: Dr. Francesc Piferrer Professor d’Investigació Institut de Ciències del Mar (ICM-CSIC) i ii A mis padres A Xavi iii iv Acknowledgements This thesis has been made possible by the support of many people who in one way or another, many times unknowingly, gave me the strength to overcome this "long and winding road". First of all, I would like to thank my supervisor, Dr. Francesc Piferrer, for his patience, guidance and wise advice throughout all this Ph.D. experience. But above all, for the trust he placed on me almost seven years ago when he offered me the opportunity to be part of his team. Thanks also for teaching me how to question always everything, for sharing with me your enthusiasm for science and for giving me the opportunity of learning from you by participating in many projects, collaborations and scientific meetings. I am also thankful to my colleagues (former and present Group of Biology of Reproduction members) for your support and encouragement throughout this journey. To the “exGBRs”, thanks for helping me with my first steps into this world. Working as an undergrad with you Dr. -
Essential Genes Shape Cancer Genomes Through Linear Limitation of Homozygous Deletions
ARTICLE https://doi.org/10.1038/s42003-019-0517-0 OPEN Essential genes shape cancer genomes through linear limitation of homozygous deletions Maroulio Pertesi1,3, Ludvig Ekdahl1,3, Angelica Palm1, Ellinor Johnsson1, Linnea Järvstråt1, Anna-Karin Wihlborg1 & Björn Nilsson1,2 1234567890():,; The landscape of somatic acquired deletions in cancer cells is shaped by positive and negative selection. Recurrent deletions typically target tumor suppressor, leading to positive selection. Simultaneously, loss of a nearby essential gene can lead to negative selection, and introduce latent vulnerabilities specific to cancer cells. Here we show that, under basic assumptions on positive and negative selection, deletion limitation gives rise to a statistical pattern where the frequency of homozygous deletions decreases approximately linearly between the deletion target gene and the nearest essential genes. Using DNA copy number data from 9,744 human cancer specimens, we demonstrate that linear deletion limitation exists and exposes deletion-limiting genes for seven known deletion targets (CDKN2A, RB1, PTEN, MAP2K4, NF1, SMAD4, and LINC00290). Downstream analysis of pooled CRISPR/Cas9 data provide further evidence of essentiality. Our results provide further insight into how the deletion landscape is shaped and identify potentially targetable vulnerabilities. 1 Hematology and Transfusion Medicine Department of Laboratory Medicine, BMC, SE-221 84 Lund, Sweden. 2 Broad Institute, 415 Main Street, Cambridge, MA 02142, USA. 3These authors contributed equally: Maroulio Pertesi, Ludvig Ekdahl. Correspondence and requests for materials should be addressed to B.N. (email: [email protected]) COMMUNICATIONS BIOLOGY | (2019) 2:262 | https://doi.org/10.1038/s42003-019-0517-0 | www.nature.com/commsbio 1 ARTICLE COMMUNICATIONS BIOLOGY | https://doi.org/10.1038/s42003-019-0517-0 eletion of chromosomal material is a common feature of we developed a pattern-based method to identify essential genes Dcancer genomes1. -

WO 2013/064702 A2 10 May 2013 (10.05.2013) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2013/064702 A2 10 May 2013 (10.05.2013) P O P C T (51) International Patent Classification: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, C12Q 1/68 (2006.01) BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (21) International Application Number: HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, PCT/EP2012/071868 KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, (22) International Filing Date: ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, 5 November 20 12 (05 .11.20 12) NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (25) Filing Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, (26) Publication Language: English ZM, ZW. (30) Priority Data: (84) Designated States (unless otherwise indicated, for every 1118985.9 3 November 201 1 (03. 11.201 1) GB kind of regional protection available): ARIPO (BW, GH, 13/339,63 1 29 December 201 1 (29. 12.201 1) US GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (71) Applicant: DIAGENIC ASA [NO/NO]; Grenseveien 92, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, N-0663 Oslo (NO). -

S41598-018-23749-W.Pdf
www.nature.com/scientificreports OPEN De novo draft assembly of the Botrylloides leachii genome provides further insight into Received: 6 September 2017 Accepted: 20 March 2018 tunicate evolution Published: xx xx xxxx Simon Blanchoud1,2, Kim Rutherford 1, Lisa Zondag1, Neil J. Gemmell 1 & Megan J. Wilson1 Tunicates are marine invertebrates that compose the closest phylogenetic group to the vertebrates. These chordates present a particularly diverse range of regenerative abilities and life-history strategies. Consequently, tunicates provide an extraordinary perspective into the emergence and diversity of these traits. Here we describe the genome sequencing, annotation and analysis of the Stolidobranchian Botrylloides leachii. We have produced a high-quality 159 Mb assembly, 82% of the predicted 194 Mb genome. Analysing genome size, gene number, repetitive elements, orthologs clustering and gene ontology terms show that B. leachii has a genomic architecture similar to that of most solitary tunicates, while other recently sequenced colonial ascidians have undergone genome expansion. In addition, ortholog clustering has identifed groups of candidate genes for the study of colonialism and whole-body regeneration. By analysing the structure and composition of conserved gene linkages, we observed examples of cluster breaks and gene dispersions, suggesting that several lineage-specifc genome rearrangements occurred during tunicate evolution. We also found lineage-specifc gene gain and loss within conserved cell-signalling pathways. Such examples of genetic changes within conserved cell-signalling pathways commonly associated with regeneration and development that may underlie some of the diverse regenerative abilities observed in tunicates. Overall, these results provide a novel resource for the study of tunicates and of colonial ascidians. -

Identification, Expression and Evolution of Short-Chain Dehydrogenases/Reductases in Nile Tilapia (Oreochromis Niloticus)
International Journal of Molecular Sciences Article Identification, Expression and Evolution of Short-Chain Dehydrogenases/Reductases in Nile Tilapia (Oreochromis niloticus) Shuai Zhang 1,†, Lang Xie 1,† , Shuqing Zheng 1, Baoyue Lu 1, Wenjing Tao 1, Xiaoshuang Wang 1, Thomas D Kocher 2 , Linyan Zhou 1,* and Deshou Wang 1,* 1 Key Laboratory of Freshwater Fish Reproduction and Development (Ministry of Education), Key Laboratory of Aquatic Science of Chongqing, School of Life Sciences, Southwest University, Chongqing 400715, China; [email protected] (S.Z.); [email protected] (L.X.); [email protected] (S.Z.); [email protected] (B.L.); [email protected] (W.T.); [email protected] (X.W.) 2 Department of Biology, University of Maryland, College Park, MD 20742, USA; [email protected] * Correspondence: [email protected] (L.Z.); [email protected] (D.W.); Tel.: +86-23-68253702 (D.W.) † These authors contributed equally to this work. Abstract: The short-chain dehydrogenases/reductases (SDR) superfamily is involved in multiple physiological processes. In this study, genome-wide identification and comprehensive analysis of SDR superfamily were carried out in 29 animal species based on the latest genome databases. Overall, the number of SDR genes in animals increased with whole genome duplication (WGD), suggesting the expansion of SDRs during evolution, especially in 3R-WGD and polyploidization of teleosts. Phylogenetic analysis indicated that vertebrates SDRs were clustered into five categories: classical, Citation: Zhang, S.; Xie, L.; Zheng, S.; extended, undefined, atypical, and complex. Moreover, tandem duplication of hpgd-a, rdh8b and Lu, B.; Tao, W.; Wang, X.; Kocher, T.D; Zhou, L.; Wang, D. -

Transposable Element Polymorphisms and Human Genome Regulation
TRANSPOSABLE ELEMENT POLYMORPHISMS AND HUMAN GENOME REGULATION A Dissertation Presented to The Academic Faculty by Lu Wang In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in Bioinformatics in the School of Biological Sciences Georgia Institute of Technology December 2017 COPYRIGHT © 2017 BY LU WANG TRANSPOSABLE ELEMENT POLYMORPHISMS AND HUMAN GENOME REGULATION Approved by: Dr. I. King Jordan, Advisor Dr. John F. McDonald School of Biological Sciences School of Biological Sciences Georgia Institute of Technology Georgia Institute of Technology Dr. Fredrik O. Vannberg Dr. Victoria V. Lunyak School of Biological Sciences Aelan Cell Technologies Georgia Institute of Technology San Francisco, CA Dr. Greg G. Gibson School of Biological Sciences Georgia Institute of Technology Date Approved: November 6, 2017 To my family and friends ACKNOWLEDGEMENTS I am truly grateful to my advisor Dr. I. King Jordan for his guidance and support throughout my time working with him as a graduate student. I am fortunate enough to have him as my mentor, starting from very basic, well-defined research tasks, and guided me step-by-step into the exciting world of scientific research. Throughout my PhD training, I have been always impressed by his ability to explain complex ideas – sometimes brilliant ideas of his own – in short and succinct sentences in such a way that his students could easily understand. I am also very impressed and inspired by his diligence and passion for his work. It is my great honor to have Dr. Greg Gibson, Dr. Victoria Lunyak, Dr. John McDonald, Dr. Fredrik Vannberg as my committee members. I really appreciate the guidance they provided me throughout my PhD study and the insightful thoughts they generously share with me during our discussions. -

The Neurodegenerative Diseases ALS and SMA Are Linked at The
Nucleic Acids Research, 2019 1 doi: 10.1093/nar/gky1093 The neurodegenerative diseases ALS and SMA are linked at the molecular level via the ASC-1 complex Downloaded from https://academic.oup.com/nar/advance-article-abstract/doi/10.1093/nar/gky1093/5162471 by [email protected] on 06 November 2018 Binkai Chi, Jeremy D. O’Connell, Alexander D. Iocolano, Jordan A. Coady, Yong Yu, Jaya Gangopadhyay, Steven P. Gygi and Robin Reed* Department of Cell Biology, Harvard Medical School, 240 Longwood Ave. Boston MA 02115, USA Received July 17, 2018; Revised October 16, 2018; Editorial Decision October 18, 2018; Accepted October 19, 2018 ABSTRACT Fused in Sarcoma (FUS) and TAR DNA Binding Protein (TARDBP) (9–13). FUS is one of the three members of Understanding the molecular pathways disrupted in the structurally related FET (FUS, EWSR1 and TAF15) motor neuron diseases is urgently needed. Here, we family of RNA/DNA binding proteins (14). In addition to employed CRISPR knockout (KO) to investigate the the RNA/DNA binding domains, the FET proteins also functions of four ALS-causative RNA/DNA binding contain low-complexity domains, and these domains are proteins (FUS, EWSR1, TAF15 and MATR3) within the thought to be involved in ALS pathogenesis (5,15). In light RNAP II/U1 snRNP machinery. We found that each of of the discovery that mutations in FUS are ALS-causative, these structurally related proteins has distinct roles several groups carried out studies to determine whether the with FUS KO resulting in loss of U1 snRNP and the other two members of the FET family, TATA-Box Bind- SMN complex, EWSR1 KO causing dissociation of ing Protein Associated Factor 15 (TAF15) and EWS RNA the tRNA ligase complex, and TAF15 KO resulting in Binding Protein 1 (EWSR1), have a role in ALS. -

View and Standard Neuropathological Analysis of Brain Sections from Affected Pedigree Members
BMC Neurology BioMed Central Research article Open Access Pedigree with frontotemporal lobar degeneration – motor neuron disease and Tar DNA binding protein-43 positive neuropathology: genetic linkage to chromosome 9 Agnes A Luty1,2,3, John BJ Kwok1,2,3, Elizabeth M Thompson4, Peter Blumbergs5, William S Brooks1,2, Clement T Loy1,2,3, Carol Dobson- Stone1,2, Peter K Panegyres6,7, Jane Hecker8, Garth A Nicholson9,10, Glenda M Halliday1,2 and Peter R Schofield*1,2,3 Address: 1Prince of Wales Medical Research Institute, Sydney, NSW, Australia, 2University of New South Wales, Sydney, NSW, Australia, 3Garvan Institute of Medical Research, Sydney, NSW, Australia, 4SA Clinical Genetics Service, Women's and Children's Hospital, Adelaide, SA, Australia, 5Institute of Medical and Veterinary Science, Adelaide, SA, Australia, 6Neurosciences Unit, Department of Health, Perth, WA, Australia, 7Neurodegenerative Disorders Research, Subiaco, WA, Australia, 8College Grove Private Hospital, Adelaide, SA, Australia, 9Northcott Neuroscience Laboratory, ANZAC Research Institute, Concord Hospital, Sydney, NSW, Australia and 10Faculty of Medicine, University of Sydney, Sydney, Australia Email: Agnes A Luty - [email protected]; John BJ Kwok - [email protected]; Elizabeth M Thompson - [email protected]; Peter Blumbergs - [email protected]; William S Brooks - [email protected]; Clement T Loy - [email protected]; Carol Dobson-Stone - [email protected]; Peter K Panegyres - [email protected]; Jane Hecker - [email protected]; Garth A Nicholson - [email protected]; Glenda M Halliday - [email protected]; Peter R Schofield* - [email protected] * Corresponding author Published: 29 August 2008 Received: 20 June 2008 Accepted: 29 August 2008 BMC Neurology 2008, 8:32 doi:10.1186/1471-2377-8-32 This article is available from: http://www.biomedcentral.com/1471-2377/8/32 © 2008 Luty et al; licensee BioMed Central Ltd.