Early Loss of Mitochondrial Complex I and Rewiring of Glutathione
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epigenetic Control of Mammalian Centromere Protein Binding: Does DNA Methylation Have a Role?
Journal of Cell Science 109, 2199-2206 (1996) 2199 Printed in Great Britain © The Company of Biologists Limited 1996 JCS3386 Epigenetic control of mammalian centromere protein binding: does DNA methylation have a role? Arthur R. Mitchell*, Peter Jeppesen, Linda Nicol†, Harris Morrison and David Kipling MRC Human Genetics Unit, Western General Hospital, Crewe Road, Edinburgh EH4 2XU, UK *Author for correspondence (internet [email protected]) †Present address: MRC Reproductive Biology Unit, Edinburgh, UK SUMMARY Chromosome 1 of the inbred mouse strain DBA/2 has a block of minor satellite DNA sequences on chromosome 1. polymorphism associated with the minor satellite DNA at The binding of the CENP-E protein does not appear to be its centromere. The more terminal block of satellite DNA affected by demethylation of the minor satellite sequences. sequences on this chromosome acts as the centromere as We present a model to explain these observations. This shown by the binding of CREST ACA serum, anti-CENP- model may also indicate the mechanism by which the B and anti-CENP-E polyclonal sera. Demethylation of the CENP-B protein recognises specific sites within the arrays minor satellite DNA sequences accomplished by growing of minor satellite DNA on mouse chromosomes. cells in the presence of the drug 5-aza-2′-deoxycytidine results in a redistribution of the CENP-B protein. This protein now binds to an enlarged area on the more terminal Key words: Centromere satellite DNA, Demethylation, Centromere block and in addition it now binds to the more internal antibody INTRODUCTION A common feature of many mammalian pericentromeric domains is that they contain families of repetitive DNA The centromere of mammalian chromosomes is recognised at sequences (Singer, 1982). -

Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers
Identification and Characterization of TPRKB Dependency in TP53 Deficient Cancers. by Kelly Kennaley A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Molecular and Cellular Pathology) in the University of Michigan 2019 Doctoral Committee: Associate Professor Zaneta Nikolovska-Coleska, Co-Chair Adjunct Associate Professor Scott A. Tomlins, Co-Chair Associate Professor Eric R. Fearon Associate Professor Alexey I. Nesvizhskii Kelly R. Kennaley [email protected] ORCID iD: 0000-0003-2439-9020 © Kelly R. Kennaley 2019 Acknowledgements I have immeasurable gratitude for the unwavering support and guidance I received throughout my dissertation. First and foremost, I would like to thank my thesis advisor and mentor Dr. Scott Tomlins for entrusting me with a challenging, interesting, and impactful project. He taught me how to drive a project forward through set-backs, ask the important questions, and always consider the impact of my work. I’m truly appreciative for his commitment to ensuring that I would get the most from my graduate education. I am also grateful to the many members of the Tomlins lab that made it the supportive, collaborative, and educational environment that it was. I would like to give special thanks to those I’ve worked closely with on this project, particularly Dr. Moloy Goswami for his mentorship, Lei Lucy Wang, Dr. Sumin Han, and undergraduate students Bhavneet Singh, Travis Weiss, and Myles Barlow. I am also grateful for the support of my thesis committee, Dr. Eric Fearon, Dr. Alexey Nesvizhskii, and my co-mentor Dr. Zaneta Nikolovska-Coleska, who have offered guidance and critical evaluation since project inception. -

A Common X-Linked Inborn Error of Carnitine Biosynthesis May Be a Risk Factor for Nondysmorphic Autism
A common X-linked inborn error of carnitine biosynthesis may be a risk factor for nondysmorphic autism Patrícia B. S. Celestino-Sopera,1, Sara Violanteb,c,1, Emily L. Crawfordd, Rui Luoe, Anath C. Lionelf, Elsa Delabyg, Guiqing Caih, Bekim Sadikovica, Kwanghyuk Leea, Charlene Loa, Kun Gaoe, Richard E. Persona, Timothy J. Mossa, Jennifer R. Germana, Ni Huangi, Marwan Shinawia,j,2, Diane Treadwell-Deeringj,k, Peter Szatmaril, Wendy Robertsm, Bridget Fernandezn, Richard J. Schroero, Roger E. Stevensono, Joseph D. Buxbaumh, Catalina Betancurg, Stephen W. Schererf,m, Stephan J. Sandersp, Daniel H. Geschwinde, James S. Sutcliffed, Matthew E. Hurlesi, Ronald J. A. Wandersb, Chad A. Shawa, Suzanne M. Leala, Edwin H. Cook, Jr.q, Robin P. Goin-Kochela,j,r, Frédéric M. Vazb,1, and Arthur L. Beaudeta,j,r,1,3 Departments of aMolecular and Human Genetics, kPsychiatry, and rPediatrics, Baylor College of Medicine, Houston, TX 77030; jTexas Children’s Hospital, Houston, TX 77030; bLaboratory Genetic Metabolic Disease, Departments of Clinical Chemistry and Pediatrics, Academic Medical Center, University of Amsterdam, 1105 AZ, Amsterdam, The Netherlands; cMetabolism and Genetics Group, Research Institute for Medicines and Pharmaceutical Sciences (iMed.UL), Faculdade de Farmácia, Universidade de Lisboa, 1649-003 Lisbon, Portugal; dDepartment of Molecular Physiology and Biophysics, Center for Molecular Neuroscience, Vanderbilt University, Nashville, TN 37232; eDepartment of Human Genetics, David Geffen School of Medicine, University of California, Los Angeles, -
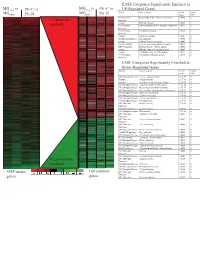
Supplement 1 Microarray Studies
EASE Categories Significantly Enriched in vs MG vs vs MGC4-2 Pt1-C vs C4-2 Pt1-C UP-Regulated Genes MG System Gene Category EASE Global MGRWV Pt1-N RWV Pt1-N Score FDR GO Molecular Extracellular matrix cellular construction 0.0008 0 110 genes up- Function Interpro EGF-like domain 0.0009 0 regulated GO Molecular Oxidoreductase activity\ acting on single dono 0.0015 0 Function GO Molecular Calcium ion binding 0.0018 0 Function Interpro Laminin-G domain 0.0025 0 GO Biological Process Cell Adhesion 0.0045 0 Interpro Collagen Triple helix repeat 0.0047 0 KEGG pathway Complement and coagulation cascades 0.0053 0 KEGG pathway Immune System – Homo sapiens 0.0053 0 Interpro Fibrillar collagen C-terminal domain 0.0062 0 Interpro Calcium-binding EGF-like domain 0.0077 0 GO Molecular Cell adhesion molecule activity 0.0105 0 Function EASE Categories Significantly Enriched in Down-Regulated Genes System Gene Category EASE Global Score FDR GO Biological Process Copper ion homeostasis 2.5E-09 0 Interpro Metallothionein 6.1E-08 0 Interpro Vertebrate metallothionein, Family 1 6.1E-08 0 GO Biological Process Transition metal ion homeostasis 8.5E-08 0 GO Biological Process Heavy metal sensitivity/resistance 1.9E-07 0 GO Biological Process Di-, tri-valent inorganic cation homeostasis 6.3E-07 0 GO Biological Process Metal ion homeostasis 6.3E-07 0 GO Biological Process Cation homeostasis 2.1E-06 0 GO Biological Process Cell ion homeostasis 2.1E-06 0 GO Biological Process Ion homeostasis 2.1E-06 0 GO Molecular Helicase activity 2.3E-06 0 Function GO Biological -

The Capacity of Long-Term in Vitro Proliferation of Acute Myeloid
The Capacity of Long-Term in Vitro Proliferation of Acute Myeloid Leukemia Cells Supported Only by Exogenous Cytokines Is Associated with a Patient Subset with Adverse Outcome Annette K. Brenner, Elise Aasebø, Maria Hernandez-Valladares, Frode Selheim, Frode Berven, Ida-Sofie Grønningsæter, Sushma Bartaula-Brevik and Øystein Bruserud Supplementary Material S2 of S31 Table S1. Detailed information about the 68 AML patients included in the study. # of blasts Viability Proliferation Cytokine Viable cells Change in ID Gender Age Etiology FAB Cytogenetics Mutations CD34 Colonies (109/L) (%) 48 h (cpm) secretion (106) 5 weeks phenotype 1 M 42 de novo 241 M2 normal Flt3 pos 31.0 3848 low 0.24 7 yes 2 M 82 MF 12.4 M2 t(9;22) wt pos 81.6 74,686 low 1.43 969 yes 3 F 49 CML/relapse 149 M2 complex n.d. pos 26.2 3472 low 0.08 n.d. no 4 M 33 de novo 62.0 M2 normal wt pos 67.5 6206 low 0.08 6.5 no 5 M 71 relapse 91.0 M4 normal NPM1 pos 63.5 21,331 low 0.17 n.d. yes 6 M 83 de novo 109 M1 n.d. wt pos 19.1 8764 low 1.65 693 no 7 F 77 MDS 26.4 M1 normal wt pos 89.4 53,799 high 3.43 2746 no 8 M 46 de novo 26.9 M1 normal NPM1 n.d. n.d. 3472 low 1.56 n.d. no 9 M 68 MF 50.8 M4 normal D835 pos 69.4 1640 low 0.08 n.d. -

An Evaluation of Host Factors As Novel Therapeutic Targets During Influenza Infection Using RNA Technologies
California State University, San Bernardino CSUSB ScholarWorks Electronic Theses, Projects, and Dissertations Office of aduateGr Studies 6-2018 An Evaluation of Host Factors as Novel Therapeutic Targets During Influenza Infection Using RNA Technologies Michael Ryan Haden Thompson California State University - San Bernardino Follow this and additional works at: https://scholarworks.lib.csusb.edu/etd Part of the Virology Commons Recommended Citation Thompson, Michael Ryan Haden, "An Evaluation of Host Factors as Novel Therapeutic Targets During Influenza Infection Using RNA Technologies" (2018). Electronic Theses, Projects, and Dissertations. 721. https://scholarworks.lib.csusb.edu/etd/721 This Thesis is brought to you for free and open access by the Office of aduateGr Studies at CSUSB ScholarWorks. It has been accepted for inclusion in Electronic Theses, Projects, and Dissertations by an authorized administrator of CSUSB ScholarWorks. For more information, please contact [email protected]. AN EVALUATION OF HOST FACTORS AS NOVEL THERAPEUTIC TARGETS DURING INFLUENZA INFECTION USING RNA TECHNOLOGIES _____________________ A Thesis Presented to the Faculty of California State University, San Bernardino _____________________ In Partial Fulfillment of the Requirements for the Degree Master of Science in Biology _____________________ by Michael Ryan Haden Thompson June 2018 AN EVALUATION OF HOST FACTORS AS NOVEL THERAPEUTIC TARGETS DURING INFLUENZA INFECTION USING RNA TECHNOLOGIES _____________________ A Thesis Presented to the Faculty of California State University, San Bernardino _____________________ By Michael Ryan Haden Thompson June 2018 Approved by: Dr. Laura L Newcomb, Committee Chair, Biology Dr. Nicole Bournias-Vardiabasis, Committee Member Dr. Daniel Nickerson, Committee Member © 2018 Michael Ryan Haden Thompson ABSTRACT Influenza A is a single-stranded, multi-segmented, negative sense RNA virus of the family Orthomyxoviridae and is the causative agent of seasonal Influenza. -

Enzyme DHRS7
Toward the identification of a function of the “orphan” enzyme DHRS7 Inauguraldissertation zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Selene Araya, aus Lugano, Tessin Basel, 2018 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Alex Odermatt (Fakultätsverantwortlicher) und Prof. Dr. Michael Arand (Korreferent) Basel, den 26.6.2018 ________________________ Dekan Prof. Dr. Martin Spiess I. List of Abbreviations 3α/βAdiol 3α/β-Androstanediol (5α-Androstane-3α/β,17β-diol) 3α/βHSD 3α/β-hydroxysteroid dehydrogenase 17β-HSD 17β-Hydroxysteroid Dehydrogenase 17αOHProg 17α-Hydroxyprogesterone 20α/βOHProg 20α/β-Hydroxyprogesterone 17α,20α/βdiOHProg 20α/βdihydroxyprogesterone ADT Androgen deprivation therapy ANOVA Analysis of variance AR Androgen Receptor AKR Aldo-Keto Reductase ATCC American Type Culture Collection CAM Cell Adhesion Molecule CYP Cytochrome P450 CBR1 Carbonyl reductase 1 CRPC Castration resistant prostate cancer Ct-value Cycle threshold-value DHRS7 (B/C) Dehydrogenase/Reductase Short Chain Dehydrogenase Family Member 7 (B/C) DHEA Dehydroepiandrosterone DHP Dehydroprogesterone DHT 5α-Dihydrotestosterone DMEM Dulbecco's Modified Eagle's Medium DMSO Dimethyl Sulfoxide DTT Dithiothreitol E1 Estrone E2 Estradiol ECM Extracellular Membrane EDTA Ethylenediaminetetraacetic acid EMT Epithelial-mesenchymal transition ER Endoplasmic Reticulum ERα/β Estrogen Receptor α/β FBS Fetal Bovine Serum 3 FDR False discovery rate FGF Fibroblast growth factor HEPES 4-(2-Hydroxyethyl)-1-Piperazineethanesulfonic Acid HMDB Human Metabolome Database HPLC High Performance Liquid Chromatography HSD Hydroxysteroid Dehydrogenase IC50 Half-Maximal Inhibitory Concentration LNCaP Lymph node carcinoma of the prostate mRNA Messenger Ribonucleic Acid n.d. -

Low Abundance of the Matrix Arm of Complex I in Mitochondria Predicts Longevity in Mice
ARTICLE Received 24 Jan 2014 | Accepted 9 Apr 2014 | Published 12 May 2014 DOI: 10.1038/ncomms4837 OPEN Low abundance of the matrix arm of complex I in mitochondria predicts longevity in mice Satomi Miwa1, Howsun Jow2, Karen Baty3, Amy Johnson1, Rafal Czapiewski1, Gabriele Saretzki1, Achim Treumann3 & Thomas von Zglinicki1 Mitochondrial function is an important determinant of the ageing process; however, the mitochondrial properties that enable longevity are not well understood. Here we show that optimal assembly of mitochondrial complex I predicts longevity in mice. Using an unbiased high-coverage high-confidence approach, we demonstrate that electron transport chain proteins, especially the matrix arm subunits of complex I, are decreased in young long-living mice, which is associated with improved complex I assembly, higher complex I-linked state 3 oxygen consumption rates and decreased superoxide production, whereas the opposite is seen in old mice. Disruption of complex I assembly reduces oxidative metabolism with concomitant increase in mitochondrial superoxide production. This is rescued by knockdown of the mitochondrial chaperone, prohibitin. Disrupted complex I assembly causes premature senescence in primary cells. We propose that lower abundance of free catalytic complex I components supports complex I assembly, efficacy of substrate utilization and minimal ROS production, enabling enhanced longevity. 1 Institute for Ageing and Health, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 2 Centre for Integrated Systems Biology of Ageing and Nutrition, Newcastle University, Newcastle upon Tyne NE4 5PL, UK. 3 Newcastle University Protein and Proteome Analysis, Devonshire Building, Devonshire Terrace, Newcastle upon Tyne NE1 7RU, UK. Correspondence and requests for materials should be addressed to T.v.Z. -

Microcephaly Genes and Risk of Late-Onset Alzheimer Disease
ORIGINAL ARTICLE Microcephaly Genes and Risk of Late-onset Alzheimer Disease Deniz Erten-Lyons, MD,*w Beth Wilmot, PhD,zy Pavana Anur, BS,z Shannon McWeeney, PhD,zyJ Shawn K. Westaway, PhD,w Lisa Silbert, MD,w Patricia Kramer, PhD,w and Jeffrey Kaye, MD*w Alzheimer’s Disease Neuroimaging Initiative ratio=3.41; confidence interval, 1.77-6.57). However, this associa- Abstract: Brain development in the early stages of life has been tion was not replicated using another case-control sample research suggested to be one of the factors that may influence an individual’s participants from the Alzheimer Disease Neuroimaging Initiative. risk of Alzheimer disease (AD) later in life. Four microcephaly We conclude that the common variations we measured in the 4 genes, which regulate brain development in utero and have been microcephaly genes do not affect the risk of AD or that their effect suggested to play a role in the evolution of the human brain, were size is small. selected as candidate genes that may modulate the risk of AD. We examined the association between single nucleotide polymorphisms Key Words: Alzheimer disease, microcephaly genes, cognitive tagging common sequence variations in these genes and risk of AD reserve in two case-control samples. We found that the G allele of (Alzheimer Dis Assoc Disord 2011;25:276–282) rs2442607 in microcephalin 1 was associated with an increased risk of AD (under an additive genetic model, P=0.01; odds Received for publication June 2, 2010; accepted December 2, 2010. enetics has been suggested to play a role in variations From the *Portland Veterans Affairs Medical Center; wDepartment of Gin cognitive function in late life.1 One way in which Neurology; zOregon Clinical and Translational Research Center; genes may play a role in cognitive function in late life is yDivision of Bioinformatics and Computational Biology, Depart- through providing an “initial endowment” that is more ment of Medical Informatics and Clinical Epidemiology; and JDivision of Biostatistics, Department of Public Health and resistant to age-related changes. -

Mir-17-92 Fine-Tunes MYC Expression and Function to Ensure
ARTICLE Received 31 Mar 2015 | Accepted 22 Sep 2015 | Published 10 Nov 2015 DOI: 10.1038/ncomms9725 OPEN miR-17-92 fine-tunes MYC expression and function to ensure optimal B cell lymphoma growth Marija Mihailovich1, Michael Bremang1, Valeria Spadotto1, Daniele Musiani1, Elena Vitale1, Gabriele Varano2,w, Federico Zambelli3, Francesco M. Mancuso1,w, David A. Cairns1,w, Giulio Pavesi3, Stefano Casola2 & Tiziana Bonaldi1 The synergism between c-MYC and miR-17-19b, a truncated version of the miR-17-92 cluster, is well-documented during tumor initiation. However, little is known about miR-17-19b function in established cancers. Here we investigate the role of miR-17-19b in c-MYC-driven lymphomas by integrating SILAC-based quantitative proteomics, transcriptomics and 30 untranslated region (UTR) analysis upon miR-17-19b overexpression. We identify over one hundred miR-17-19b targets, of which 40% are co-regulated by c-MYC. Downregulation of a new miR-17/20 target, checkpoint kinase 2 (Chek2), increases the recruitment of HuR to c- MYC transcripts, resulting in the inhibition of c-MYC translation and thus interfering with in vivo tumor growth. Hence, in established lymphomas, miR-17-19b fine-tunes c-MYC activity through a tight control of its function and expression, ultimately ensuring cancer cell homeostasis. Our data highlight the plasticity of miRNA function, reflecting changes in the mRNA landscape and 30 UTR shortening at different stages of tumorigenesis. 1 Department of Experimental Oncology, European Institute of Oncology, Via Adamello 16, Milan 20139, Italy. 2 Units of Genetics of B cells and lymphomas, IFOM, FIRC Institute of Molecular Oncology Foundation, Milan 20139, Italy. -

Aneuploidy: Using Genetic Instability to Preserve a Haploid Genome?
Health Science Campus FINAL APPROVAL OF DISSERTATION Doctor of Philosophy in Biomedical Science (Cancer Biology) Aneuploidy: Using genetic instability to preserve a haploid genome? Submitted by: Ramona Ramdath In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Examination Committee Signature/Date Major Advisor: David Allison, M.D., Ph.D. Academic James Trempe, Ph.D. Advisory Committee: David Giovanucci, Ph.D. Randall Ruch, Ph.D. Ronald Mellgren, Ph.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: April 10, 2009 Aneuploidy: Using genetic instability to preserve a haploid genome? Ramona Ramdath University of Toledo, Health Science Campus 2009 Dedication I dedicate this dissertation to my grandfather who died of lung cancer two years ago, but who always instilled in us the value and importance of education. And to my mom and sister, both of whom have been pillars of support and stimulating conversations. To my sister, Rehanna, especially- I hope this inspires you to achieve all that you want to in life, academically and otherwise. ii Acknowledgements As we go through these academic journeys, there are so many along the way that make an impact not only on our work, but on our lives as well, and I would like to say a heartfelt thank you to all of those people: My Committee members- Dr. James Trempe, Dr. David Giovanucchi, Dr. Ronald Mellgren and Dr. Randall Ruch for their guidance, suggestions, support and confidence in me. My major advisor- Dr. David Allison, for his constructive criticism and positive reinforcement. -

Numerical Chromosome 1, 7, 9, and 11 Aberrations in Bladder Cancer Detected by in Situ Hybridization1
[CANCER RESEARCH 51, 644-651, January 15. 1991] Numerical Chromosome 1, 7, 9, and 11 Aberrations in Bladder Cancer Detected by in Situ Hybridization1 Anton H. N. Hopman,2 Olof Moesker, A. Wim G. B. Smeets, Ruud P. E. Pauwels, G. Peter Vooijs, and Frans C. S. Ramaekers Department of Pathology, L'niversity //ospitai Nijmegen, fieert Grooteplein Zulu 24, 6525 (iA, .\ijmegen ¡A.H. N. H., O. .\t., C. P. ('./.' Stickling Ziekenkuisapotkeek en Klinisch Laboratorium l'enray [A. H'. G. B. S.J; Department of Urology, Hospital I enlo-1 'enray [R. P. K. P.], and Department of Molecular Cell Biology, L'nirersity ofLimhurg, Maastricht ¡A.H. N. H., F. C. S. R.], The Netherlands. ABSTRACT studies we demonstrated that this approach enables a routine screening of large tumor cell populations in, for example, Forty transitional cell carcinomas of the human urinary bladder (TCCs) TCCs4 (5, 10). Furthermore, ISH enables the detection of minor were examined for numerical aberrations of chromosomes 1, 7, 9, and 11 by in situ hybridization using chromosome-specific probes. Our inter- cell populations or imbalance in chromosome copy number phase cytogenetic study of 24 low-grade, noninvasive TCCs, which were within one tumor. near-diploid by flow cytometry, showed a numerical aberration for at By means of conventional karyotyping nonrandom chromo least I of these chromosomes in 14 of these cases. Most strikingly, a some aberrations involving chromosomes 1, 7, 9, and 11 have monosomy for chromosome 9 was found in 9 of 24 low-grade TCCs. A been detected in bladder cancer.