Novel Immunobiology for a Lupus-Risk Gene
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sequence Analysis and Comparative Study of the Protein Subunits of Archaeal Rnase P
biomolecules Review Sequence Analysis and Comparative Study of the Protein Subunits of Archaeal RNase P Manoj P. Samanta 1,*,†, Stella M. Lai 2,3,†, Charles J. Daniels 3,4 and Venkat Gopalan 2,3,* 1 Systemix Institute, Redmond, WA 98053, USA 2 Department of Chemistry & Biochemistry, The Ohio State University, Columbus, OH 43210, USA; [email protected] 3 Center for RNA Biology, The Ohio State University, Columbus, OH 43210, USA; [email protected] 4 Department of Microbiology, The Ohio State University, Columbus, OH 43210, USA * Correspondence: [email protected] (M.P.S.); [email protected] (V.G.); Tel.: +1-425-898-8187 (M.P.S.); +1-614-292-1332 (V.G.) † These authors contributed equally to this work. Academic Editor: Denis Drainas Received: 1 March 2016; Accepted: 8 April 2016; Published: 20 April 2016 Abstract: RNase P, a ribozyme-based ribonucleoprotein (RNP) complex that catalyzes tRNA 51-maturation, is ubiquitous in all domains of life, but the evolution of its protein components (RNase P proteins, RPPs) is not well understood. Archaeal RPPs may provide clues on how the complex evolved from an ancient ribozyme to an RNP with multiple archaeal and eukaryotic (homologous) RPPs, which are unrelated to the single bacterial RPP. Here, we analyzed the sequence and structure of archaeal RPPs from over 600 available genomes. All five RPPs are found in eight archaeal phyla, suggesting that these RPPs arose early in archaeal evolutionary history. The putative ancestral genomic loci of archaeal RPPs include genes encoding several members of ribosome, exosome, and proteasome complexes, which may indicate coevolution/coordinate regulation of RNase P with other core cellular machineries. -

Association of Gene Ontology Categories with Decay Rate for Hepg2 Experiments These Tables Show Details for All Gene Ontology Categories
Supplementary Table 1: Association of Gene Ontology Categories with Decay Rate for HepG2 Experiments These tables show details for all Gene Ontology categories. Inferences for manual classification scheme shown at the bottom. Those categories used in Figure 1A are highlighted in bold. Standard Deviations are shown in parentheses. P-values less than 1E-20 are indicated with a "0". Rate r (hour^-1) Half-life < 2hr. Decay % GO Number Category Name Probe Sets Group Non-Group Distribution p-value In-Group Non-Group Representation p-value GO:0006350 transcription 1523 0.221 (0.009) 0.127 (0.002) FASTER 0 13.1 (0.4) 4.5 (0.1) OVER 0 GO:0006351 transcription, DNA-dependent 1498 0.220 (0.009) 0.127 (0.002) FASTER 0 13.0 (0.4) 4.5 (0.1) OVER 0 GO:0006355 regulation of transcription, DNA-dependent 1163 0.230 (0.011) 0.128 (0.002) FASTER 5.00E-21 14.2 (0.5) 4.6 (0.1) OVER 0 GO:0006366 transcription from Pol II promoter 845 0.225 (0.012) 0.130 (0.002) FASTER 1.88E-14 13.0 (0.5) 4.8 (0.1) OVER 0 GO:0006139 nucleobase, nucleoside, nucleotide and nucleic acid metabolism3004 0.173 (0.006) 0.127 (0.002) FASTER 1.28E-12 8.4 (0.2) 4.5 (0.1) OVER 0 GO:0006357 regulation of transcription from Pol II promoter 487 0.231 (0.016) 0.132 (0.002) FASTER 6.05E-10 13.5 (0.6) 4.9 (0.1) OVER 0 GO:0008283 cell proliferation 625 0.189 (0.014) 0.132 (0.002) FASTER 1.95E-05 10.1 (0.6) 5.0 (0.1) OVER 1.50E-20 GO:0006513 monoubiquitination 36 0.305 (0.049) 0.134 (0.002) FASTER 2.69E-04 25.4 (4.4) 5.1 (0.1) OVER 2.04E-06 GO:0007050 cell cycle arrest 57 0.311 (0.054) 0.133 (0.002) -

(P -Value<0.05, Fold Change≥1.4), 4 Vs. 0 Gy Irradiation
Table S1: Significant differentially expressed genes (P -Value<0.05, Fold Change≥1.4), 4 vs. 0 Gy irradiation Genbank Fold Change P -Value Gene Symbol Description Accession Q9F8M7_CARHY (Q9F8M7) DTDP-glucose 4,6-dehydratase (Fragment), partial (9%) 6.70 0.017399678 THC2699065 [THC2719287] 5.53 0.003379195 BC013657 BC013657 Homo sapiens cDNA clone IMAGE:4152983, partial cds. [BC013657] 5.10 0.024641735 THC2750781 Ciliary dynein heavy chain 5 (Axonemal beta dynein heavy chain 5) (HL1). 4.07 0.04353262 DNAH5 [Source:Uniprot/SWISSPROT;Acc:Q8TE73] [ENST00000382416] 3.81 0.002855909 NM_145263 SPATA18 Homo sapiens spermatogenesis associated 18 homolog (rat) (SPATA18), mRNA [NM_145263] AA418814 zw01a02.s1 Soares_NhHMPu_S1 Homo sapiens cDNA clone IMAGE:767978 3', 3.69 0.03203913 AA418814 AA418814 mRNA sequence [AA418814] AL356953 leucine-rich repeat-containing G protein-coupled receptor 6 {Homo sapiens} (exp=0; 3.63 0.0277936 THC2705989 wgp=1; cg=0), partial (4%) [THC2752981] AA484677 ne64a07.s1 NCI_CGAP_Alv1 Homo sapiens cDNA clone IMAGE:909012, mRNA 3.63 0.027098073 AA484677 AA484677 sequence [AA484677] oe06h09.s1 NCI_CGAP_Ov2 Homo sapiens cDNA clone IMAGE:1385153, mRNA sequence 3.48 0.04468495 AA837799 AA837799 [AA837799] Homo sapiens hypothetical protein LOC340109, mRNA (cDNA clone IMAGE:5578073), partial 3.27 0.031178378 BC039509 LOC643401 cds. [BC039509] Homo sapiens Fas (TNF receptor superfamily, member 6) (FAS), transcript variant 1, mRNA 3.24 0.022156298 NM_000043 FAS [NM_000043] 3.20 0.021043295 A_32_P125056 BF803942 CM2-CI0135-021100-477-g08 CI0135 Homo sapiens cDNA, mRNA sequence 3.04 0.043389246 BF803942 BF803942 [BF803942] 3.03 0.002430239 NM_015920 RPS27L Homo sapiens ribosomal protein S27-like (RPS27L), mRNA [NM_015920] Homo sapiens tumor necrosis factor receptor superfamily, member 10c, decoy without an 2.98 0.021202829 NM_003841 TNFRSF10C intracellular domain (TNFRSF10C), mRNA [NM_003841] 2.97 0.03243901 AB002384 C6orf32 Homo sapiens mRNA for KIAA0386 gene, partial cds. -

Nuclear PTEN Safeguards Pre-Mrna Splicing to Link Golgi Apparatus for Its Tumor Suppressive Role
ARTICLE DOI: 10.1038/s41467-018-04760-1 OPEN Nuclear PTEN safeguards pre-mRNA splicing to link Golgi apparatus for its tumor suppressive role Shao-Ming Shen1, Yan Ji2, Cheng Zhang1, Shuang-Shu Dong2, Shuo Yang1, Zhong Xiong1, Meng-Kai Ge1, Yun Yu1, Li Xia1, Meng Guo1, Jin-Ke Cheng3, Jun-Ling Liu1,3, Jian-Xiu Yu1,3 & Guo-Qiang Chen1 Dysregulation of pre-mRNA alternative splicing (AS) is closely associated with cancers. However, the relationships between the AS and classic oncogenes/tumor suppressors are 1234567890():,; largely unknown. Here we show that the deletion of tumor suppressor PTEN alters pre-mRNA splicing in a phosphatase-independent manner, and identify 262 PTEN-regulated AS events in 293T cells by RNA sequencing, which are associated with significant worse outcome of cancer patients. Based on these findings, we report that nuclear PTEN interacts with the splicing machinery, spliceosome, to regulate its assembly and pre-mRNA splicing. We also identify a new exon 2b in GOLGA2 transcript and the exon exclusion contributes to PTEN knockdown-induced tumorigenesis by promoting dramatic Golgi extension and secretion, and PTEN depletion significantly sensitizes cancer cells to secretion inhibitors brefeldin A and golgicide A. Our results suggest that Golgi secretion inhibitors alone or in combination with PI3K/Akt kinase inhibitors may be therapeutically useful for PTEN-deficient cancers. 1 Department of Pathophysiology, Key Laboratory of Cell Differentiation and Apoptosis of Chinese Ministry of Education, Shanghai Jiao Tong University School of Medicine (SJTU-SM), Shanghai 200025, China. 2 Institute of Health Sciences, Shanghai Institutes for Biological Sciences of Chinese Academy of Sciences and SJTU-SM, Shanghai 200025, China. -

Different Requirements for EDS1 and NDR1 by Disease Resistance Genes Define at Least Two R Gene-Mediated Signaling Pathways in Arabidopsis
Proc. Natl. Acad. Sci. USA Vol. 95, pp. 10306–10311, August 1998 Plant Biology Different requirements for EDS1 and NDR1 by disease resistance genes define at least two R gene-mediated signaling pathways in Arabidopsis NICOLE AARTS*, MATTHEW METZ†,ERIC HOLUB‡,BRIAN J. STASKAWICZ†,MICHAEL J. DANIELS*, AND JANE E. PARKER*§ *Sainsbury Laboratory, John Innes Centre, Colney Lane, Norwich NR4 7UH, United Kingdom; †Department of Plant Biology, Koshland Hall, University of California, Berkeley, CA 94720-3102; and ‡Horticultural Research International, Wellesbourne, Warwick CV35 9EF, United Kingdom Edited by Frederick M. Ausubel, Harvard Medical School, Boston, MA, and approved June 11, 1998 (received for review April 3, 1998) ABSTRACT The Arabidopsis genes EDS1 and NDR1 were localized either extracellularly or within the cytoplasm are shown previously by mutational analysis to encode essential structurally different to Pto and contain leucine-rich repeats components of race-specific disease resistance. Here, we ex- (LRRs) (5), implicating protein–protein interactions as part of amined the relative requirements for EDS1 and NDR1 by a the recognition process. In the putatively cytoplasmic R pro- broad spectrum of Resistance (R) genes present in three tein members, the LRRs lie adjacent to sequences that con- Arabidopsis accessions (Columbia, Landsberg-erecta, and stitute a nucleotide binding site (NBS) (5). The NBSyLRR Wassilewskija). We show that there is a strong requirement class of R proteins can be subdivided into members that for EDS1 by a subset of R loci (RPP2, RPP4, RPP5, RPP21, and possess an amino-terminal leucine zipper (LZ) motif or those RPS4), conferring resistance to the biotrophic oomycete Per- that have amino-terminal similarity to the cytoplasmic do- onospora parasitica, and to Pseudomonas bacteria expressing mains of the Drosophila Toll and mammalian interleukin 1 the avirulence gene avrRps4. -

Computational Prediction of Associations Between Long Non
Lu et al. BMC Genomics 2013, 14:651 http://www.biomedcentral.com/1471-2164/14/651 METHODOLOGY ARTICLE Open Access Computational prediction of associations between long non-coding RNAs and proteins Qiongshi Lu1,2,5, Sijin Ren1,3, Ming Lu1, Yong Zhang4, Dahai Zhu4, Xuegong Zhang2 and Tingting Li1,3* Abstract Background: Though most of the transcripts are long non-coding RNAs (lncRNAs), little is known about their functions. lncRNAs usually function through interactions with proteins, which implies the importance of identifying the binding proteins of lncRNAs in understanding the molecular mechanisms underlying the functions of lncRNAs. Only a few approaches are available for predicting interactions between lncRNAs and proteins. In this study, we introduce a new method lncPro. Results: By encoding RNA and protein sequences into numeric vectors, we used matrix multiplication to score each RNA–protein pair. This score can be used to measure the interactions between an RNA–protein pair. This method effectively discriminates interacting and non-interacting RNA–protein pairs and predicts RNA–protein interactions within a given complex. Applying this method on all human proteins, we found that the long non- coding RNAs we collected tend to interact with nuclear proteins and RNA-binding proteins. Conclusions: Compared with the existing approaches, our method shortens the time for training matrix and obtains optimal results based on the model being used. The ability of predicting the associations between lncRNAs and proteins has also been enhanced. Our method provides an idea on how to integrate different information into the prediction process. Keywords: Long non-coding RNA, RNA–protein interaction, Computation Background biological processes, including epigenetic regulation, Recent studies show that only a small part of the human chromatin remodeling, and cell proliferation and differ- transcriptome is involved in the protein-coding process entiation, the molecular mechanisms underlying the [1]. -

Coexpression Networks Based on Natural Variation in Human Gene Expression at Baseline and Under Stress
University of Pennsylvania ScholarlyCommons Publicly Accessible Penn Dissertations Fall 2010 Coexpression Networks Based on Natural Variation in Human Gene Expression at Baseline and Under Stress Renuka Nayak University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/edissertations Part of the Computational Biology Commons, and the Genomics Commons Recommended Citation Nayak, Renuka, "Coexpression Networks Based on Natural Variation in Human Gene Expression at Baseline and Under Stress" (2010). Publicly Accessible Penn Dissertations. 1559. https://repository.upenn.edu/edissertations/1559 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/edissertations/1559 For more information, please contact [email protected]. Coexpression Networks Based on Natural Variation in Human Gene Expression at Baseline and Under Stress Abstract Genes interact in networks to orchestrate cellular processes. Here, we used coexpression networks based on natural variation in gene expression to study the functions and interactions of human genes. We asked how these networks change in response to stress. First, we studied human coexpression networks at baseline. We constructed networks by identifying correlations in expression levels of 8.9 million gene pairs in immortalized B cells from 295 individuals comprising three independent samples. The resulting networks allowed us to infer interactions between biological processes. We used the network to predict the functions of poorly-characterized human genes, and provided some experimental support. Examining genes implicated in disease, we found that IFIH1, a diabetes susceptibility gene, interacts with YES1, which affects glucose transport. Genes predisposing to the same diseases are clustered non-randomly in the network, suggesting that the network may be used to identify candidate genes that influence disease susceptibility. -

Phenotype Relationship
Downloaded from genome.cshlp.org on September 25, 2021 - Published by Cold Spring Harbor Laboratory Press Perspective Recognition of the polycistronic nature of human genes is critical to understanding the genotype- phenotype relationship Marie A. Brunet,1,2,3 Sébastien A. Levesque,4 Darel J. Hunting,5 Alan A. Cohen,2 and Xavier Roucou1,3 1Biochemistry Department, Université de Sherbrooke, Quebec J1E 4K8, Canada; 2Groupe de recherche PRIMUS, Department of Family and Emergency Medicine, Quebec J1H 5N4, Canada; 3PROTEO, Quebec Network for Research on Protein Function, Structure, and Engineering, Université Laval, Quebec G1V 0A6, Canada; 4Pediatric Department, Centre Hospitalier de l’Université de Sherbrooke, Quebec J1H 5N4, Canada; 5Department of Nuclear Medicine & Radiobiology, Université de Sherbrooke, Quebec J1H 5N4, Canada Technological advances promise unprecedented opportunities for whole exome sequencing and proteomic analyses of pop- ulations. Currently, data from genome and exome sequencing or proteomic studies are searched against reference genome annotations. This provides the foundation for research and clinical screening for genetic causes of pathologies. However, current genome annotations substantially underestimate the proteomic information encoded within a gene. Numerous studies have now demonstrated the expression and function of alternative (mainly small, sometimes overlapping) ORFs within mature gene transcripts. This has important consequences for the correlation of phenotypes and genotypes. Most alternative ORFs are -

Computational Studies of the Genome Dynamics of Mammalian Transposable Elements and Their Relationships to Genes
COMPUTATIONAL STUDIES OF THE GENOME DYNAMICS OF MAMMALIAN TRANSPOSABLE ELEMENTS AND THEIR RELATIONSHIPS TO GENES by Ying Zhang M.Sc., Katholieke Universiteit Leuven (BELGIUM), 2004 B.E., Harbin Institute of Technology (CHINA), 1993 A THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY in THE FACULTY OF GRADUATE STUDIES (Genetics) THE UNIVERSITY OF BRITISH COLUMBIA (Vancouver) May, 2012 © Ying Zhang, 2012 Abstract Sequences derived from transposable elements (TEs) comprise nearly 40 - 50% of the genomic DNA of most mammalian species, including mouse and human. However, what impact they may exert on their hosts is an intriguing question. Originally considered as merely genomic parasites or “selfish DNA”, these mobile elements show their detrimental effects through a variety of mechanisms, from physical DNA disruption to epigenetic regulation. On the other hand, evidence has been mounting to suggest that TEs sometimes may also play important roles by participating in essential biological processes in the host cell. The dual-roles of TE-host interactions make it critical for us to understand the relationship between TEs and the host, which may ultimately help us to better understand both normal cellular functions and disease. This thesis encompasses my three genome-wide computational studies of TE-gene dynamics in mammals. In the first, I identified high levels of TE insertional polymorphisms among inbred mouse strains, and systematically analyzed their distributional features and biological effects, through mining tens of millions of mouse genomic DNA sequences. In the second, I examined the properties of TEs located in introns, and identified key factors, such as the distance to the intron-exon boundary, insertional orientation, and proximity to splice sites, that influence the probability that TEs will be retained in genes. -

Oxygen and Glucose Deprivation Induces Widespread Alterations In
Andreev et al. Genome Biology (2015) 16:90 DOI 10.1186/s13059-015-0651-z RESEARCH Open Access Oxygen and glucose deprivation induces widespread alterations in mRNA translation within 20 minutes Dmitry E Andreev1,2†, Patrick BF O’Connor1†, Alexander V Zhdanov1, Ruslan I Dmitriev1, Ivan N Shatsky2, Dmitri B Papkovsky1,3 and Pavel V Baranov1* Abstract Background: Oxygen and glucose metabolism play pivotal roles in many (patho)physiological conditions. In particular, oxygen and glucose deprivation (OGD) during ischemia and stroke results in extensive tissue injury and cell death. Results: Using time-resolved ribosome profiling, we assess gene expression levels in a neural cell line, PC12, during the first hour of OGD. The most substantial alterations are seen to occur within the first 20 minutes of OGD. While transcription of only 100 genes is significantly altered during one hour of OGD, the translation response affects approximately 3,000 genes. This response involves reprogramming of initiation and elongation rates, as well as the stringency of start codon recognition. Genes involved in oxidative phosphorylation are most affected. Detailed analysis of ribosome profiles reveals salient alterations of ribosome densities on individual mRNAs. The mRNA-specific alterations include increased translation of upstream open reading frames, site-specific ribosome pauses, and production of alternative protein isoforms with amino-terminal extensions. Detailed analysis of ribosomal profiles also reveals six mRNAs with translated ORFs occurring downstream of annotated coding regions and two examples of dual coding mRNAs, where two protein products are translated from the same long segment of mRNA, but in two different frames. Conclusions: These findings uncover novel regulatory mechanisms of translational response to OGD in mammalian cells that are different from the classical pathways such as hypoxia inducible factor (HIF) signaling, while also revealing sophisticated organization of protein coding information in certain genes. -
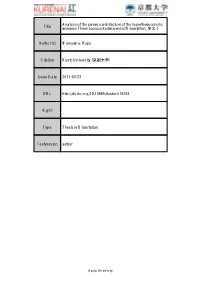
Title Analysis of the Genome Architecture of The
Analysis of the genome architecture of the hyperthermopholic Title archaeon Thermococcus kodakarensis( Dissertation_全文 ) Author(s) Maruyama, Hugo Citation Kyoto University (京都大学) Issue Date 2011-03-23 URL http://dx.doi.org/10.14989/doctor.k16233 Right Type Thesis or Dissertation Textversion author Kyoto University Analysis of the genome architecture of the hyperthermophilic archaeon Thermococcus kodakarensis Hugo Maruyama 要旨 ゲノム DNA は細胞内で高度に折りたたまれ、この染色体高次構造は転写・複製・染色体分 配といった機構と密接に結びついている。染色体の主要な構成タンパク質は真核生物では ヒストン、バクテリアでは HU と全く異なるが、一様な基本構造を基にゲノム DNA が階層 的に折りたたまれている点で両者の染色体構造は共通している。アーキアは真核生物・バ クテリアと並ぶ生命の第三のドメインであり、遺伝情報の発現(複製・転写・翻訳)の機 構は真核生物に、代謝経路はバクテリアに近い。アーキアには染色体を構成するタンパク 質として真核生物のヒストンに相同なもの、バクテリアの HU に相同なもの、アーキア特有 の Alba と呼ばれるタンパク質などが存在し、種によってゲノムがコードするタンパク質の 組合せが異なる。様々なアーキアのゲノムがどのような高次構造を形成しているかを明ら かにすることで、三つのドメインにわたるゲノム構造の共通性あるいは多様性を明らかに できる。本研究ではその第一歩としてヒストンを持つ超好熱性アーキア Thermococcus kodakarensis の染色体構造を解析した。 T. kodakarensis の染色体に含まれるタンパク質を質量分析により同定した結果、ヒ ストン、Alba、TK0471(TrmBL2)、 RNA ポリメラーゼ等の DNA 結合タンパク質が含まれ ることが分かった。TK0471 は転写因子 TrmB と相同な機能未知の DNA 結合タンパク質で あった。次に、染色体をミクロコッカルヌクレアーゼで部分消化した後、5%-20%のショ糖 密度勾配遠心により構成タンパク質の異なる染色体断片が分離された。原子間力顕微鏡に よる解析から、ヒストンは DNA 上に beads-on-a-string 構造を、TK0471 は線維状の構造を形 成することが示された。また大腸菌で発現させた組換えタンパク質(ヒストンおよび TK0471)を用いて同様の構造が DNA 上に再構成された。ショ糖密度勾配で分離されたそ れぞれの染色体断片に含まれる DNA 配列を超並列シークエンサーで同定した結果、ヒスト ンおよび TK0471 はゲノム上のプロモーター領域にもコーディング領域にも偏りなく存在 するが、両者の存在する領域は重複しない傾向があった。以上の結果から、T. kodakarensis の染色体上には、構成タンパク質および構造の異なる領域が存在することが明らかとなっ た。相同組換えにより TK0471 遺伝子を破壊すると染色体の DNA 消化酵素に対する感受性 が高まった。また、約 100 個の遺伝子の転写産物量が増加した。TK0471 -

Recognition of the Polycistronic Nature of Human Genes Is Critical to Understanding the Genotype-Phenotype Relationship
Downloaded from genome.cshlp.org on October 7, 2021 - Published by Cold Spring Harbor Laboratory Press 1 Recognition of the polycistronic nature of human genes is critical 2 to understanding the genotype-phenotype relationship 3 4 Marie A. Brunet1, 2, 3, Sébastien A. Levesque4, Darel J. Hunting5, Alan A. Cohen2, and Xavier 5 Roucou1, 3 6 7 1 Biochemistry Department; 2 Groupe de Recherche PRIMUS, Department of Family and 8 Emergency Medicine; 3 PROTEO, Quebec Network for Research on Protein Function, Structure, 9 and Engineering; 4 Pediatrics Department, Centre Hospitalier de l’Université de Sherbrooke; 10 5 Department of Nuclear Medicine & Radiobiology, Université de Sherbrooke, Quebec, Canada. 11 12 Corresponding authors: 13 Xavier Roucou: Biochemistry department, Université de Sherbrooke, 3201 Jean Mignault, 14 Sherbrooke, Québec J1E 4K8, Canada, Tel. (819) 821-8000x72240; E-Mail: 15 [email protected] 16 Marie Brunet: Biochemistry department, Université de Sherbrooke, 3201 Jean Mignault, 17 Sherbrooke, Québec J1E 4K8, Canada, Tel. (819) 821-8000x72189; E-Mail: 18 [email protected] 19 1 Downloaded from genome.cshlp.org on October 7, 2021 - Published by Cold Spring Harbor Laboratory Press 20 Abstract: 21 Technological advances promise unprecedented opportunities for whole exome sequencing and 22 proteomic analyses of populations. Currently, data from genome and exome sequencing, or 23 proteomic studies are searched against reference genome annotations. This provides the 24 foundation for research and clinical screening for genetic causes of pathologies. However, 25 current genome annotations substantially underestimate the proteomic information encoded 26 within a gene. Numerous studies have now demonstrated the expression and function of 27 alternative (mainly small, sometimes overlapping) ORFs within mature gene transcripts.